Semilobarholoprosencephaly – A Dreading Congenital Anomaly
Bhushita B Lakhkar1, Bhushan N Lakhkar2, Bhavana B Lakhkar3
1 Assistant Professor, Department of Radiology, Shri B M Patil Medical College, Hospital and Research Center, Bijapur, Karnataka, India.
2 Profeesor and Head, Department of Radiology, Shri B M Patil Medical College, Hospital and Research Center, Bijapur, Karnataka, India.
3 Professor, Department of Paediatrics, Shri B M Patil Medical College, Hospital and Research Center, Bijapur, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Bhushita B Lakhkar, Staff Quarter No. 22 Bldeu Campus Smt Bangaramma Sajjan Campus Sholapur Road, Bijapur, Karnataka, India.
E-mail: bhushitalakhkar@gmail.com
Holoprosencephaly (HPE) is a group of structural abnormalities of brain that is an important cause of childhood mortality and morbidity. They usually occur due to impaired midline cleavage of embryonic forebrain i.e., failure of differentiation of the prosencephalon into the telecephalon and diencephalon. De Myer classified this anomaly ranging from alobar to semilobar and lobar type. It can be associated with microcephaly and midline facial anomalies. We present a case of semilobar holoprosencephaly with corpus callosal agenesis.
Corpus callosal agenesis, Failure of midline cleavage, Fused basal ganglia
Case Report
A 14-month-old female child presented in the Department of Paediatrics with complaints of delay in attaining milestones such as sitting, standing, speaking monosyllables and was labelled to have global developmental delay. On examination, she was found to have microcephaly however no facial malformations were seen. She was subsequently referred to Department of Radiodiagnosis for Computed Tomography (CT) of brain.
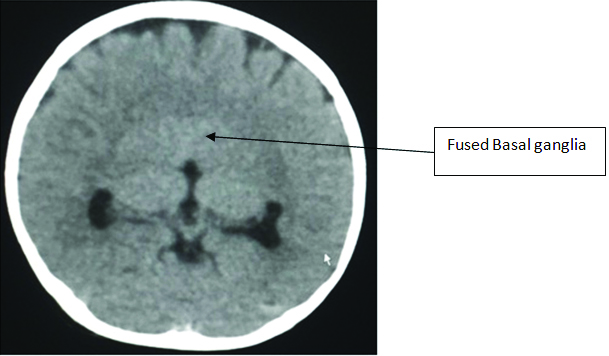
CT brain showed fusion of bilateral frontal lobes with absence of anterior falx cerebri, posteriorly falxcerebri was present [Table/Fig-1]. Bilateral frontal horns of lateral ventricles were absent [Table/Fig-2] with presence of colpocephaly and dilated third ventricle. Bilateral basal ganglia were partially fused although the thalami were separate and normal [Table/Fig-3]. Complete agenesis of corpus callosum was noted [Table/Fig-4]. All these findings were in favour of semilobar-holoprosencephaly with associated corpus callosum agenesis.
a) Absence of anterior falx with presence of falx cerebri posteriorly; b) fusion of bilateral frontal lobes.

Absent frontal horns of lateral ventricle with fused bilateral basal ganglia. Bilateral occipital horns are formed.

Bilaterally separated thalami with fused basal ganglia.
Agenesis of corpus callosum.

Discussion
Holoprosencephaly (HPE) is a group of structural abnormalities of brain and an important cause of childhood mortality and morbidity. It was often thought as lethal but in fact it is a spectrum of malformations with widely variable outcome. Embryologically the cephalic end of the neural tube forms three primary vesicles: the forebrain (prosencephalon), midbrain (mesencephalon) and hindbrain (rhombencephalon). The prosencephalon undergoes the following sequential events: formation, cleavage, and midline development [1]. Absence of these divisions of prosencephalon leads to a spectrum of holoprosencephaly anomalies. It can be associated with midline developmental anomalies like agenesis of the corpus callosum, septo-optic dysplasia and isolated absence of the cavum septum pellucidum. De Myer classified this anomaly ranging from alobar to semilobar and lobar types [2]. The aetiology of holoprosencephaly is still unknown. However, few suggested causal agents are hypoxia and transplacental infection. Alobar is the most severe form followed by semilobar and lobar holoprosencephaly [3].
In alobar holoprosencephaly, a rim of cerebral tissue is present anteriorly surrounding a large monoventricle. The basal ganglia, thalami are fused along with absence of interhemispheric fissure [3].
Lobar HPE, the least severe subtype; the falxcerebri is present along the entire midline and the thalami are completely separated. The corpus callosum may be normal or incomplete, but the cavum septum pellucidum is always absent. Some frontal horns of lateral ventricle are present, and only the most inferior portions of the frontal lobes are fused. The differentiation between semilobar and lobar HPE may create problem but if there is presence of third ventricle, rudimentary frontal horns, the splenium and posterior body of the corpus callosum are present then we can call this entity as lobar [4].
In semilobar holoprosencephaly, the anterior inter-hemispheric fissure/falx cerebri are absent however they are present posteriorly.
The corpus callosum may be seen in the region of separated hemispheres, or it may be entirely absent. Due to absence of falxcerebri anteriorly, the frontal lobes are mostly fused [4]. HPE is usually associated with midline facial anomalies however; it may or may not be present. Facial anomalies which are associated with HPE are usually mild like cleft lip, cleft palate, and hypotelorism [5]. These infants are usually microcephalic but if there is presence of a large dorsal cyst macrocephaly can also be seen [3].
Our case is a representative of semilobar holoprosencephaly with fused basal ganglia, fused frontal lobes, absent anterior falxcerebri, absent frontal horn of lateral ventricle and absent corpus callosum. No craniofacial abnormalities were found in our patient. Similar type of cases were also reported in literature with few different findings like Patil V et al., reported a case of semilobar holoprosencephaly with a ’H’ shaped monoventricle, partially developed temporal and occipital horns and partially fused thalami. Rudimentary falx and interhemispheric fissure were present along with partial agenesis of corpus callosum [6]. Zikou A et al., reported a two-month-old baby with anteriorly fused cerebral lobes and fused thalami. There was agenesis of the genu and the body of corpus callosum [7]. Pallangyor P et al., reported a 12-month-old baby with presentations of global developmental delay, erratic sleep patterns and poor weight gain. MRI shows incompletely formed interhemispheric fissure, a monoventricle with partially developed temporal and occipital horns, partial fusion of frontal lobe, hypoplastic corpus callosum [8].
A recent fourth subtype of holoprosencephaly, namely middle hemispheric variant was added. In this condition, the interhemispheric fissure is formed in frontal and occipital regions but absent in parietal regions along with fusion of the hemispheres [9].
The severity of the craniofacial abnormalities tends to mirror the severity of the brain malformations. The most severe facial malformations include microcephaly, cyclopia, synophthalmia, proboscis (a tube-like nasal appendage with a single nostril located above the ocular region). Less severe facial malformations can include microcephaly (except in cases of hydrocephalus, which can cause macrocephaly), hypotelorism, midface hypoplasia with a flat nasal bridge, cleft lip and/or palate, ocular colobomas, and a single maxillary central incisor [9].
HPE is generally diagnosed prenatally by prenatal transabdominal or transvaginal ultrasound [10]. Ultrasound is the gold standard modality to diagnose alobar and semilobar holoprosencephaly in as early as the first trimester. However, in our case of HPE it was missed on antenatal ultrasound and later it was diagnosed on CT scan after birth. Holoprosencephaly are one of the most common conditions missed on prenatal ultrasound scan and we believe that CT is an ideal modality to detect and classify them after birth. As MRI due to cost effect cannot be used by all patients but still it is considered the best modality to diagnose and classify HPE [10,11]. On MRI, alobar HPE results in a horseshoe shaped monoventricle and an absent hemispheric fissure. Semilobar HPE shows single ventricular cavity with partial separation and a partial interhemispheric fissure or falx (mostly posterior) [10,12]. Though management of HPE is mainly supportive but requires a multidisciplinary approach with main aim at managing symptoms and complications, and avoiding added disability to improve the overall quality of life [8].
The prognosis of such patients depends on the severity of holoprosencephaly. Alobar and semilobar HPE have a very poor prognosis, all infants with the more severe form die in infancy. Few children with semilobar HPE may survive into infancy with amentia. In lobar HPE patients mental impairment, visual and olfactory abnormalities are often present but they can lead a normal life [13].
Conclusion
Holoprosencephaly is a rare disorder and involves both the brain and the face. Diagnosis of this anomaly is often challenging. It is important to diagnose the case of HPE and its type prenatally so that its severity and its complications can be determined and proper counselling can be done for parents.
[1]. Blaas HG, Eik-Nes SH, Sonoembryology and early prenatal diagnosis of neural anomaliesPrenat Diagn 2009 29(4):312-25. [Google Scholar]
[2]. Hahn JS, Barnes PD, Neuroimaging advances in holoprosencephaly: refining the spectrum of the midline malformationAm J Med Genet C Semin Med Genet 2010 154(C1):120-32. [Google Scholar]
[3]. Volpe O, Campobasso G, De Robertis V, Rembouskos G, Disorders of prosencephalic developmentPrenat Diagn 2009 29(4):340-54. [Google Scholar]
[4]. Winter TC, Kennedy AM, Woodward PJ, Holoprosencephaly: a survey of the entity, with embryology and fetal imagingRadiographics 2015 35(1):275-90. [Google Scholar]
[5]. Raman R, Jagadesh G, Antenatal diagnosis of Alobar holoprosencephalyCase reports in Radiology 2014 2014:724671 [Google Scholar]
[6]. Patil V, Taori K, Sardesai N, Ingle V, Semi lobar holoprosencephaly- a case reportIndian J Radiol Imaging 2005 15(4):576 [Google Scholar]
[7]. Zikou A, Tzoufi M, Nakou I, Xydis V, Argyropoulou M, Semilobar holoprosencephaly with a median cleft: case reportEuro Rad 2015 Last accessed 3/13/2017URL: http://www.eurorad.org/case.php?id=12630 [Google Scholar]
[8]. Pallangyor P, Lyimo F, Nicholaus P, Makungu H, Mtolera M, Mawenya I, Semilobar holoprosencephaly in a 12-month-old baby boy born to a primigravida patient with type 1 diabetes mellitus: a case reportJournal of Medical Case Reports 2016 10:358 [Google Scholar]
[9]. Albayram S, Melhem ER, Mori S, Zinreich SJ, Barkovich AJ, Kinsman SL, Holoprosencephaly in children: diffusion tensore MR imaging of white matter tracts of the brainstem: initial experienceRadiology 2002 223(3):645-51. [Google Scholar]
[10]. Tegay DH, Cohen HL, Rosovsky M, HoloprosencephalyMedicine 2005 Last accessed 3/13/2017http://emedicine.medscape.com/article/409265-overview [Google Scholar]
[11]. Cohen MM, Holoprosencephaly: clinical, anatomic, and molecular dimensionsBirth Defects Res A Clin Mol Teratol 2006 76:658-73. [Google Scholar]
[12]. Hahn JS, Plawner LL, Evaluation and management of children with holoprosencephalyPediatr Neurol 2004 31:79-88. [Google Scholar]
[13]. Fowlie A, Constantine G, Dewbury K, Meire H, Cosgrove D, Holoprosencephaly, the central nervous systemUltrasound in obstetrics and gynaecology 1993 292Churchill Livingstone-294. [Google Scholar]