Multiple Cutaneous Tuberculous Abscess: A Case Report
Rahul Suna1, Ramu Duttaluri2
1 Senior Resident, Department of Orthopaedics, Durgabai Deshmukh Hospital, Hyderabad, Telangana, India.
2 Professor and Head, Department of Orthopaedics, Durgabai Deshmukh Hospital, Hyderabad, Telangana, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rahul Suna, Flat No B-208, Pranit Happy Homes, Subhodaya Colony, Nizampet, Kukatpally, Hyderabad-500072, Telangana, India.
E-mail: drsunarahul@gmail.com
Cutaneous tuberculosis is a relatively rare form of extrapulmonary tuberculosis. It usually manifests secondary to haematogenous spread or from an underlying focus of infection. We report a case of multiple tuberculous abscesses without any primary focus. A 26-year-old female, presented with polyarthalgia since four months and multiple abscesses over the body since three months. No response was seen after taking various courses of antibiotics and analgesics, which was misdiagnosed as bacterial abscesses. Skin biopsy showed multiple epitheloid cell granulomas with multinucleated giant cells suggestive of tuberculosis. After treating the patient with antitubercular therapy, complete resolution of the lesions occurred within four weeks.
Tuberculosis with unusual presentations is common in endemic countries like India. A high index of suspicion with regard to cutaneous tuberculosis presenting as multiple abscess and nodule without any underlying lesion is essential.
Biopsy, Extrapulmonary, Granuloma, Polyarthalgia, Skin
Case Report
A 26-year-old female, reported with a chief complaint of polyarthalgia since four months and multiple swelling over body since three months. She had swelling over left wrist, left leg, left foot, right foot, right gluteal region which were previously diagnosed as bacterial abscesses. She received various courses of antibiotics for which she was not responding. The swellings were initially small sized, but continued to increase in size and evolved into an ulcer on right foot. She had a recent history of weight loss, with no history of fever and cough. No co-morbities like HIV, diabetes or any history of tuberculosis or significant disease in the past was noted. She had no history of Koch’s contact and belongs to lower middle socioeconomic status. Her general condition was stable.
On local examination there were papulo-pustular lesions on the dorsal aspect of left wrist 2 cm × 2 cm [Table/Fig-1], left leg middle one third 1 cm × 1 cm on lateral aspect, lateral border of left foot 2 cm × 1 cm, right gluteal region 2 cm × 2 cm and ulcer of 1 cm ×1 cm on right foot. The ulcer over right foot had undermined edge with indurated margin surrounded by a zone of hyperpigmentation with mild serosanguinous discharge and granulation at the base of the ulcer [Table/Fig-2]. There was no local rise of temperature and tenderness. No palpable lymph nodes in the body.
Papulo-pustular swelling of 2 cm × 2 cm over dorsal aspect of left wrist.

Tuberculous ulcer of 1×1 cm over dorsal aspect of right foot.

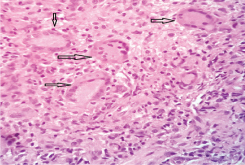
Routine investigations showed normal blood counts with raised Erythrocyte Sedimentation Rate (ESR) which was 60 mm/after one hour and Mantoux test was positive. Ulcer edge biopsy from the lesion was done and subjected to histopathological examination, which showed multiple epitheloid cell granulomas and multinucleated giant cells in deeper region with focal necrosis, suggestive of tuberculosis [Table/Fig-3]. Diagnosis of multiple cutaneous tuberculosis was made. Chest X-ray and corresponding X-ray of hand, foot and leg was taken, no underlying primary lesion was identified. The patient was started on a daily regimen of four-drug Antitubercular Therapy (ATT) consisting of isoniazid (H) 300 mg/d, rifampicin (R)450 mg/d, pyrazinamide (Z)1500 mg/d and ethambutol (E)800 mg/d which was given for two months followed by HR daily regimen for four months. Patient became asymptomatic of polyarthalgia within two weeks, swellings and ulcer healed within four weeks after starting ATT and there was no recurrence after completion of six months ATT treatment [Table/Fig-4].
Histopathological examination of ulcer edge biopsy shows multiple epithelioid cell granuloma and multinucleated giant cells in the deeper region with focal necrosis (40X).
Healed tuberculous ulcer after four weeks of antituberculosis therapy.

Discussion
Tuberculosis is a major health problem in India. Cutaneous tuberculosis is a rare form accounting for 1.5% of all cases of extrapulmonary tuberculosis and occurs in 0.15% of all cases of skin disease [1]. It is often misdiagnosed because of a low index of suspicion. Cutaneous tuberculous abscesses are a rare and unusual presentation of TB that is commonly located on the extremities trunk or head and commonly found in the immunocompromised [2]. It is characterized by nodule and abscess formation throughout the body after haematogenous spread of Mycobacterium tuberculosis from a primary focus during a period of impaired immunity [3]. It poses a serious challenge to the clinician, who must differentiate this condition from several other diseases of the skin presenting as papules, nodules, or ulcers [4]. The initial presentation may resemble that of common bacterial infection, but antibiotics targeting Gram-positive cocci exert no effect on the lesion [4]. The disease is usually slow growing, and has an insidious course and an unusual presentation; a chronically discharging sinus or a non-healing ulcer is possible [5]. Tuberculous ulcer is characteristically a non-healing ulcer with undermined edge and indurated margin, surrounded by a zone of hyperpigmentation with serosanguinous discharge and granulation at the base of the ulcer. In our case, tuberculosis was suspected based on clinical presentation of ulcer, which is characteristic. Histopathological finding and good response to ATT further confirmed our diagnosis. However, a high index of suspicion is necessary in such atypical clinical presentations.
On histopathology, multiple epitheloid cell granulomas is often suggestive of tuberculosis, however it should be differentiated from Nontuberculous Mycobacteria (NTM) which also presents as granulomatous lesion on biopsy. NTM is a milder form than tuberculous mycobacteria and often has a history of open wound or surgical procedure or injections. NTM are usually resistant to routine antitubercular medicines [6]. In the present case there were no history of trauma or injections and good response to antituberculous drugs within two to four weeks of treatment. Even though culture of biopsy sample is gold standard for diagnosing tuberculosis, many times culture is absent for any growth due to the paucibacillary status of extrapulmonary tuberculosis. In endemic country like India, diagnosis of extrapulmonary tuberculosis is based on the clinical suspicion and histopathological examination [7].
Case reports are published with multiple cutaneous tubercular abscess with pulmonary tuberculosis [2,8], and skeletal tuberculosis [3,9,10], however there are reports showing that it may occur without any underlying tuberculous focus [11-13], as occurred in our patient with multiple abscesses without any underlying focus. During subclinical or latent phase of tuberculous infection, bacilli are seeded at various organs like skin, some are healed completely, and some may remain quiescent containing viable bacilli to become active during the period of impaired immunity [11]. This probably explains the absence of active primary focus in our case.
The standard six months regimen for adults includes isoniazid, rifampin, pyrazinamide, and ethambutol for the initial two months followed by isoniazid and rifampin for a further four months in the continuation phase [14]. A clinical response should be expected between weeks fourth week and six week of treatment [1]. In our case, response of treatment was seen within four weeks of starting antituberculosis therapy.
Conclusion
Multiple cutaneous tuberculous abscesses is an extremely rare presentation leading to misdiagnosis as bacterial abscesses. Diagnosing multiple tuberculous abscesses in absence of underlying primary focus is difficult. High index of suspicion and awareness regarding tuberculous abscesses even without underlying lesion is essential.
[1]. Pacheco C, Silva E, Miranda J, Duarte R, Cutaneous tuberculosis as metastatic tuberculous abscessJ Bras Pneumol 2015 41(2):200-02. [Google Scholar]
[2]. Parker L, Babu S, Tuberculous gumma: a forgotten entity in the UKBMJ Case Rep 2013 2013:bcr2013010462 [Google Scholar]
[3]. Sezgin B, Atilganoglu U, Yigit O, Ergun SS, Cambaz N, Demirkesen C, Concomitant cutaneous metastatic tuberculous abscesses and multifocal skeletal tuberculosisIndian J Dermatol 2008 53(3):149-53. [Google Scholar]
[4]. Casalini C, Mattelli A, Saleri N, Caligaris S, Graifemberhi S, Pizzocolo C, Nodular lesions of the skin as primary cutaneous tuberculosisJ Travel Med 2003 10(5):306-08. [Google Scholar]
[5]. Kim G-W, Park H-J, Kim H-S, Kim S-H, Ko H-C, Kim B-S, Delayed diagnosis of scrofuloderma misdiagnosed as a bacterial abscessAnn Dermatol 2012 24(1):70-73. [Google Scholar]
[6]. Gundavda MK, Patil HG, Agashe VM, Soman R, Rodriques C, Deshpande RB, Nontuberculous mycobacterial infection of the musculoskeletal system in immunocompetent hostsIndian J Orthop 2017 51(2):205-12. [Google Scholar]
[7]. Purohit M, Mustafa T, Laboratory diagnosis of extra-pulmonary tuberculosis (EPTB) in resource constrained setting: state of the art, challenges and the needJ Clin Diagn Res 2015 9(4):EE01-EE06. [Google Scholar]
[8]. Petit A, Maslo C, Herschkovitch D, Perrin P, Janier M, Civatte J, Multiple subcutaneous abscesses due to Mycobacterium tuberculosis in an immunocompetent hostDermatologica 1989 179:207-10. [Google Scholar]
[9]. Saral Y, Coskun BK, Ozturk P, Bulut Y, Cobanoglu B, Multiple metastatic tuberculosis abscesses in a patient with pott disease and lung tuberculosis: a case reportJ Cutan Pathol 2005 32(9):629-33. [Google Scholar]
[10]. Pereira A, Miranda A, Santo FE, Fernandes P, Cutaneous and skeletal simultaneous locations as a rare clinical presentation of tuberculosisCase Reports in Infectious Diseases 2015 (2015):618546 [Google Scholar]
[11]. Banashankari GS, Rudresh HK, Harsha AH, Bharathi R, Kamble P, An unusual presentation of cutaneous tuberculosis for surgeons—review of literatureIndian J Surg 2012 74(4):314-17. [Google Scholar]
[12]. Samitas K, Marinakis E, Birbilis C, Thanos L, Zervas E, Gaga M, Multiple tuberculous abscesses and mediastinal lymphadenitis with no pulmonary involvement in an immunocompetent patientIndian J Tuberc 2012 59:235-39. [Google Scholar]
[13]. Mehta M, Anjaneyan G, Rathod K, Vora RV, Multifocal Cutaneous Tuberculosis in Immunocompetent IndividualJ Clin Diagn Res 2015 9(12):WD01-WD02. [Google Scholar]
[14]. Handog EB, Gabriel TG, Pineda RT, Management of cutaneous tuberculosisDermatol Ther 2008 21(3):154-61. [Google Scholar]