Introduction
Role of epidural analgesia in laparoscopic surgery is questionable. There is paucity of data comparing local surgical site infiltration with epidural analgesia in laparoscopic colorectal resections.
Aim
To evaluate the efficacy and feasibility of local surgical site infiltration versus epidural analgesia in laparoscopic low anterior resection done for adenocarcinoma of the rectum.
Materials and Methods
This retrospective cohort study was done on 37 patients who had undergone laparoscopic low anterior resection at a single institution from January 2014 to March 2016. Patients were divided into two cohorts; Infiltration group (n=23) and Epidural group (n=14). Baseline characteristics and postoperative outcomes like number of patients requiring opioid rescue analgesia, incidence of urinary tract infection, postoperative hospital stay and overall morbidity were compared. Statistical analysis was done using SPSS software version 16.0. Mann-Whitney U test, Fischer’s-exact test and Pearson Chi-square test were used to test the significance wherever necessary.
Results
The number of patients requiring rescue opioid analgesia within the first 48 hours following surgery were 5 (35.7%) in the epidural group versus 4 (17.4%) in the infiltration group (p=0.255). The incidence of urinary tract infection at the index admission was 2 (14.3%) in the epidural group versus 2 (8.7%) in the infiltration group (p=0.625). Overall morbidity calculated using Clavien Dindo classification was 8 (57.14%) and 14 (60.8%) respectively in epidural and infiltration group (p=0.836). The median (interquartile range) postoperative hospital stay for the epidural group was nine days (5-13 days) and for the infiltration group was eight days (5-15 days).
Conclusion
Surgical site infiltration is a simple technique comparable to epidural analgesia for immediate postoperative pain control in terms of efficacy and feasibility in laparoscopic low anterior resections.
Analgesia methods, Laparoscopy, Pain, Postoperative, Rectal resection
Introduction
Surgery remains the main stay of treatment in the multimodal management of rectal cancer [1]. Rectal resections have been traditionally done by open method. In the last two decades, the role of laparoscopic surgery for rectal cancer is becoming more established as it has been shown to be on par with open surgery with respect to both short and long term oncological outcomes [2]. Laparoscopic approach to rectal resections has resulted in faster recovery and quicker initiation of adjuvant therapy [3].
Mechanism of postoperative pain in laparoscopic operations is different from that of open operations [4]. In addition to somatic component of pain due to penetrating trocar or abdominal wall suturing [5], there is a visceral mechanism postulated which is caused by traction of the peritoneum and adjacent nerves, irritation of the diaphragm due to surgical manipulation, carbon dioxide insufflation and due to retained gas after laparoscopy [6,7]. In addition, the tissue and nerve injury due to surgical trauma leads to increased levels of inflammatory cytokines and other chemicals which can induce central and peripheral nervous system sensitisation augmenting pain [8,9]. It has been observed that laparoscopic operations performed with pressures maintained under 10 mmHg have been less painful than higher pressures of pneumo–peritoneum [10,11].
Improper and inadequate pain management can result in various cardiovascular, respiratory, psychological and gastrointestinal complications including chronic post surgical pain [12-14].
There are various methods of postoperative pain control in laparoscopic rectal resections like Transversus Abdominis Plane (TAP) blocks, epidural analgesia, local wound infiltration, systemically administered opioids, non steroidal anti-inflammatory drugs and other multimodal adjuncts. Appropriate modality of pain control has to be chosen based on the type of rectal resection [15].
It was thought that in laparoscopic low anterior resection, since the specimen extraction site was small and usually less than 7 cm in length in addition to four other port insertion sites; adequate surgical site infiltration with local anaesthetic agent would suffice. Some centers also advocate patient controlled analgesia and TAP block for immediate postoperative pain management [16,17]. There is a paucity of literature comparing the efficacy of surgical site infiltration versus epidural analgesia in laparoscopic rectal resection.
The aim of our study was to compare the efficacy of local surgical site infiltration versus epidural analgesia in laparoscopic low anterior resection for adenocarcinoma rectum. Since laparoscopic low anterior resection was done routinely with a left lower abdominal transverse extraction incision along with a covering loop ileostomy in our center, it was proposed to compare the two modalities of postoperative analgesia in these specific group of patients for uniformity in the port insertion sites, specimen extraction site and the expertise of surgeons performing the operation.
Materials and Methods
This was a retrospective cohort study done in the colorectal surgical unit at the Christian Medical College Vellore, which is a tertiary care center in India. All patients who had undergone laparoscopic low anterior resection for rectal cancer between January 2014 and March 2016 were included in this study. Patients requiring additional procedures other than the above mentioned procedure or patients in whom colorectal anastomosis was deferred due to various preoperative and intraoperative factors were excluded. After approval from the Institutional Review Board (CMC VELLORE IRB No. 10154), data on the relevant outcome parameters were extracted and analysed.
All the patients had either received thoracic epidural analgesia or local surgical site subcutaneous infiltration.
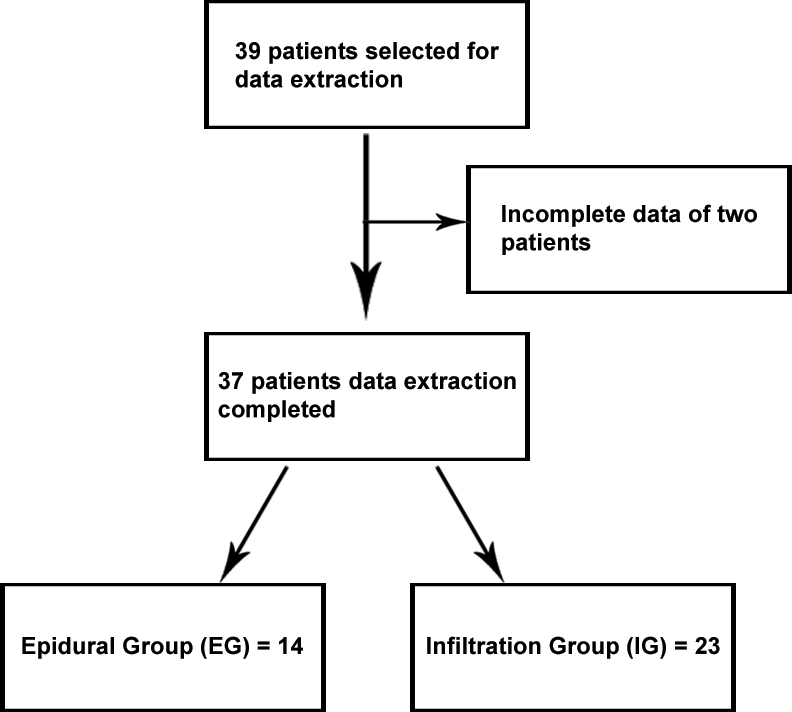
Data was extracted from online inpatient charts and clinical workstation. There were a total of 39 laparoscopic low anterior resections done during this period, of which complete online data was available for thirty-seven patients [Table/Fig-1]. The following outcome parameters were compared between the Epidural Group (EG) and the Infiltration Group (IG):
Patient selection process.
Number of patients requiring opioid rescue doses within 48 hours after surgery;
Incidence of urinary tract infection within the index admission period;
Morbidity based on Clavien-Dindo score (1 to 5, 5 being the worst) [18]; and
Duration of postoperative hospital stay in days.
Procedure
Appropriate Venous Thromboembolism (VTE) and antibiotic prophylaxis was given. Anaesthesia with regard to induction, maintenance and extubation followed a standard protocol as per department policy. Patients in the Epidural Group had an epidural catheter inserted prior to anaesthesia and epidural infusion with 0.25% bupivacaine, at 4 to 5 ml per hour, was started immediately after induction till skin closure. This was later replaced with 0.1% bupivacaine along with fentanyl 2 mg per ml maintained at 4 to 5 ml per hour postoperatively. Patients in the Infiltration Group had all the port sites, specimen extraction site and ileostomy site infiltrated with 0.25% bupivacaine at a dosage not exceeding beyond 2 mg per kilogram body weight prior to skin closure.
Senior colorectal surgeons performed all laparoscopic low anterior resections who had at least three years of experience in advanced laparoscopy. Port sites and specimen extraction sites were standard for the procedure. There were two 10 mm ports inserted in the right lumbar and right iliac fossa region and two 5 mm ports inserted in the epigastric and left lumbar regions. The specimen extraction site was made in the left lumbar region less than 7 cm in length in a transverse or oblique fashion and this specimen was extracted after applying Alexis wound protector (Applied Medical Resources Corporation, California). Once the colorectal anastomosis was performed with circular stapler, a covering loop ileostomy was fashioned in the premarked site in right iliac fossa. Rectus in the specimen extraction site was closed with no.1 Polydioxanone (PDS) in a continuous fashion and skin was closed with skin staplers.
Statistical Analysis
Data was entered in to Microsoft excel sheet and Statistical analysis was done using SPSS software version 16.0. Mann-Whitney U test, Fischer’s-exact test and Pearson Chi-square test were used to test the significance wherever necessary. Data were presented as medians and interquartile ranges. A p-value of less than or equal to 0.05 was considered significant.
Results
Among the 37 patients, fourteen were from the EG and 23 were from the IG. There were 11 males and three females in the EG and 16 males and seven females in the IG. The mean age of patients in the EG was 51.35 years and the IG was 49.69 years [Table/Fig-2].
Baseline characteristics of patients undergoing laparoscopic low anterior resection.
| Patient characteristics | Epidural Group (EG)(n=14) | Infiltration Group (IG)(n=23) |
|---|
| Average Age (in years) | 51.35 | 49.69 |
| Males | 11 | 16 |
| Females | 3 | 7 |
| ASA physical status |
| I | 6 | 11 |
| II | 8 | 12 |
| III | 0 | 0 |
a) Opioid rescue numbers: In the EG, 5 (35.7%) of 14 patients required rescue pain relief with parenteral morphine (0.1 mg/Kg body wt/dose) within 48 hours following the operation. About four of them required a single dose of opioid rescue, whereas one patient required three doses. In the IG 4 (17.4%) of 23 patients required rescue parenteral morphine for pain relief. All four of them received a single rescue dose of parenteral opioid within the first 48 hours following surgery. The difference between both the groups was not found statistically significant (p=0.255) [Table/Fig-3].
Outcomes of Epidural Group (EG) versus surgical site Infiltration Group (IG) after laparoscopic low anterior resection.
| Epidural group (EG)(n=14) | Infiltration group (IG)(n=23) | p-value |
|---|
| Opioid rescue numbers* | 5 (35.7%) | 4 (17.4%) | 0.255 |
| Incidence of Urinary tract infection* | 2 (14.3%) | 2 (8.7%) | 0.625 |
| Overall Morbidity ** | 8 (57.14%) | 14 (60.8%) | 0.836 |
| Duration of Postoperative hospital stay, median days ***(interquartile range) | 9 (5-13) | 8 (5-15) | 0.863 |
* Fisher’s-exact test
** Pearson Chi-square test
*** Mann-Whitney U test
b) Incidence of Urinary Tract Infection (UTI): In the EG, 2 (14.3%) of 14 patients were diagnosed to have culture positive urinary tract infection within the same admission and 2 (8.7%) of 23 patients in the IG had UTI. The difference between both the groups was not found statistically significant (p=0.625) [Table/Fig-3].
c) Postoperative hospital stay: The median (interquartile range) postoperative hospital stay for the EG was nine days (5-13 days) and for the IG was eight days (5-15 days). This difference was not statistically significant (p=0.863) [Table/Fig-3].
d) Postoperative morbidity: The overall complication rate in the EG was 8 (57.14%) out of 14 patients and in the IG it was 14 (60.8%) out of 23 patients. The difference between both the groups was not found statistically significant (p-value =0.836) [Table/Fig-4].
Postoperative morbidity rate based on Clavien-Dindo classification.
| Epidural group (EG) (n=14) | Infiltration group (IG) (n=23) |
|---|
| Overall complication rate | 8 (57.14%) | 14 (60.8%) |
| Complication (Clavien-Dindo classification) | | |
| I | 3 | 4 |
| II | 3 | 4 |
| III | 1 | 5 |
| IV | 1 | 1 |
| V | 0 | 0 |
Discussion
Literature regarding optimal postoperative pain control in laparoscopic rectal resection is lacking. With the advent of enhanced recovery protocol, thoracic epidural analgesia has been proposed for better pain control and faster recovery in open rectal resections and the same has been extrapolated to laparoscopic rectal resections as well [19]. However in laparoscopic rectal resections, the need for epidural analgesia is questionable [20]. Moreover the specimen extraction site is usually 5 to 7 cm in length and many surgeons believe local wound infiltration to be equivalent to or even better than epidural analgesia for this immediate postoperative pain relief [21,22].
Epidural analgesia requires an epidural catheter to be placed prior to anaesthesia and being an invasive procedure, it is not devoid of problems. In addition to the time consumed for insertion of epidural catheter, complications like hypotension requiring frequent use of vasopressor agents; lower limb sensory and motor blockade and nausea along with vomiting are often seen [23]. Serious complications like dural puncture, epidural hematoma and epidural abscess though rare have been reported [24].
Due to the problems mentioned above, other modalities of postoperative pain control have been investigated in various studies. Ventham NT et al., found in their systematic review and meta-analysis that in a heterogenous group of patients, local anaesthetic wound infiltration was associated with comparable pain scores to that obtained by epidural analgesia in abdominal surgeries [25]. TAP block, local wound infiltration, wound infusion, fentanyl based Patient Controlled Analgesia (PCA), intravenous lignocaine and multimodal analgesia have been compared in various abdominal surgeries and it has been found that no single mode of analgesia is by far superior than the rest [26]. Various types of TAP block has been compared with epidural analgesia by several authors like Kadam VR and Moran JL, Niraj G et al., and Ganapathy S et al., in laparotomy and have concluded TAP to be non inferior to epidural analgesia [27-29]. In a meta-analysis of RCT’s by Borzellino G et al., role of epidural analgesia within ERAS programme after laparoscopic colorectal surgery did not seem to offer any additional clinical benefits to patients when compared to TAP block, PCA, continuous wound infusion and IV lignocaine [19]. Similarly Pedrazzani C et al., have shown that TAP block along with local infiltration provides reduced opioid requirement and good pain control in the setting of laparoscopic colorectal surgery [30].
Various forms of analgesia are practiced based on available modality and preference at various centres. Local surgical site infiltration [22,31] is done for all port sites, extraction site and stoma creation site prior to skin closure, in the subcutaneous plane using bupivacaine 0.25% not exceeding 2 mg per kilogram of body weight. Surgical site infiltration is simple to perform and can be done by a surgeon with any level of expertise. Its importance in laparoscopic operations is even more due to the relatively small incisions involved as compared to open operations. Therefore, this retrospective cohort study was conducted to evaluate the efficacy and feasibility of epidural analgesia with local wound infiltration specifically in laparoscopic low anterior resection.
Analysis of pain score using visual analogue score would have been a better tool to compare both the groups. Since in our institution, student nurses assessed visual analogue score inconsistently, their value and reliability was doubtful. Hence the next best option was to calculate the number of patients and doses of parenteral rescue opioid analgesia for breakthrough pain relief within the first 48 hours following the operation. In the EG, 35.7% of patients received parenteral rescue analgesia with opioids whereas only 17.4% of patients received it in the IG which is nearly half the number of patients than that of in the epidural group showing a trend towards better postoperative pain control in the IG although the difference was not statistically significant (p=0.255).
There was no statistically significant difference between both the groups in terms of incidence of culture positive UTI’s or median postoperative hospital stay. The overall morbidity in the EG was 57.14% as compared to 60.8% in the IG. There were no complications recorded due to epidural catheter placement in this group of patients, which is expected due to the small group of patients studied. Nevertheless epidural analgesia is known to cause several complications, which should be weighed against the intended benefits especially in laparoscopic surgery.
In the context of fastrack surgery, it is advisable to study and compare various factors affecting outcomes one at a time keeping the other variables constant. It should also be understood that various types of surgical approaches (open versus laparoscopy) might require tailored protocols depending on the complexity and requirement for analgesia. We feel that epidural analgesia may be unnecessary in laparoscopic low anterior resections and that local surgical site infiltration will provide comparable postoperative analgesia at the same time avoiding complications associated with epidural analgesia. Role of local surgical site infiltration as part and package of pre-emptive analgesia and it’s role in preventing chronic post surgical pain mechanisms are recipes for future well formulated studies [7,9,14].
Limitation
Retrospective cohorts study in itself is limited by the nature of selection bias and information bias. Further well designed randomized controlled studies are required to assess cost-effectiveness; role in pre-emptive analgesia and chronic post surgical pain in both these forms of postoperative analgesia especially in laparoscopic low anterior resections in the context of fastrack protocols.
Conclusion
Studies comparing surgical site local infiltration and epidural analgesia in laparoscopic rectal resections are limited. This study has shown that local surgical site infiltration and epidural analgesia did not differ in rescue analgesic consumption or in overall complication rates. Our retrospective analysis suggests that local surgical site infiltration is a simple and reasonable alternative to epidural analgesia for immediate postoperative pain control in laparoscopic low anterior resections.
* Fisher’s-exact test
** Pearson Chi-square test
*** Mann-Whitney U test
[1]. Dayal S, Battersby N, Cecil T, Evolution of Surgical Treatment for Rectal Cancer: A ReviewJ Gastrointest Surg 2017 21(7):1166-73. [Google Scholar]
[2]. Lelong B, Bege T, Esterni B, Guiramand J, Turrini O, Moutardier V, Short-term outcome after laparoscopic or open restorative mesorectal excision for rectal cancer: A comparative cohort studyDis Colon Rectum 2007 50(2):176-83. [Google Scholar]
[3]. Biondi A, Grosso G, Mistretta A, Marventano S, Toscano C, Drago F, Laparoscopic vs. open approach for colorectal cancer: Evolution over time of minimal invasive surgeryBMC Surg 2013 13(2):S12 [Google Scholar]
[4]. El-Sherbiny W, Saber W, Askalany AN, El-Daly A, Sleem AAA, Effect of intra-abdominal instillation of lidocaine during minor laparoscopic proceduresInt J Gynaecol Obstet Off Organ Int Fed Gynaecol Obstet 2009 106(3):213-15. [Google Scholar]
[5]. Gough AE, Chang S, Reddy S, Ferrigno L, Zerey M, Grotts J, Periprosthetic anaesthetic for postoperative pain after laparoscopic ventral hernia repair: A randomized clinical trialJAMA Surg 2015 150(9):835-40. [Google Scholar]
[6]. Kaba A, Laurent SR, Detroz BJ, Sessler DI, Durieux ME, Lamy ML, Intravenous lidocaine infusion facilitates acute rehabilitation after laparoscopic colectomyAnaesthesiology 2007 106(1):11-18. [Google Scholar]
[7]. Chou YJ, Ou YC, Lan KC, Jawan B, Chang SY, Kung FT, Preemptive analgesia installation during gynecologic laparoscopy: A randomized trialJ Minim Invasive Gynecol 2005 12(4):330-35. [Google Scholar]
[8]. Beilin B, Bessler H, Mayburd E, Smirnov G, Dekel A, Yardeni I, Effects of preemptive analgesia on pain and cytokine production in the postoperative periodAnaesthesiology 2003 98(1):151-55. [Google Scholar]
[9]. Kelly DJ, Ahmad M, Brull SJ, Preemptive analgesia I: Physiological pathways and pharmacological modalitiesCan J Anaesth 2001 48(10):1000-10. [Google Scholar]
[10]. Ekstein P, Szold A, Sagie B, Werbin N, Klausner JM, Weinbroum AA, Laparoscopic Surgery May Be Associated With Severe Pain and High Analgesia Requirements in the Immediate Postoperative PeriodAnn Surg 2006 243(1):41-46. [Google Scholar]
[11]. Vecchio R, Murabito P, Panascia E, Di Martino M, Rinzivillo C, Cunsolo V, Postoperative pain in laparoscopic surgeryIl G Chir 2002 23(1-2):13-17. [Google Scholar]
[12]. Golzari SEJ, Nader ND, Mahmoodpoor A, Underlying mechanisms of postoperative pain after laparoscopic surgeryJAMA Surg 2016 151(3):295-96. [Google Scholar]
[13]. Rahman HM, Beattie J, “Managing post-operative pain,”The Pharmaceutical Journal 2005 275:145URI:10030893. Available from: http://www.scirp.org/(S(i43dyn45teexjx455qlt3d2q))/reference/ReferencesPapers.aspx?ReferenceID=199966 [Google Scholar]
[14]. Neil MJ, Macrae WA, Post surgical pain- the transition from acute to chronic painRev Pain 2009 3(2):06-09. [Google Scholar]
[15]. Ayad S, Babazade R, Elsharkawy H, Nadar V, Lokhande C, Makarova N, Comparison of Transversus Abdominis Plane Infiltration with Liposomal Bupivacaine versus Continuous Epidural Analgesia versus Intravenous Opioid AnalgesiaPLoS ONE [Internet] 2016 11(4):e0153675 [Google Scholar]
[16]. Wu Y, Liu F, Tang H, Wang Q, Chen L, Wu H, The analgesic efficacy of subcostal transversus abdominis plane block compared with thoracic epidural analgesia and intravenous opioid analgesia after radical gastrectomyAnaesth Analg 2013 117(2):507-13. [Google Scholar]
[17]. Revie EJ, McKeown DW, Wilson JA, Garden OJ, Wigmore SJ, Randomized clinical trial of local infiltration plus patient-controlled opiate analgesia vs. epidural analgesia following liver resection surgeryHPB 2012 14(9):611-18. [Google Scholar]
[18]. Dindo D, Demartines N, Clavien PA, Classification of Surgical ComplicationsAnn Surg 2004 240(2):205-13. [Google Scholar]
[19]. Borzellino G, Francis NK, Chapuis O, Krastinova E, Dyevre Vrie, Role of epidural analgesia within an eras program after laparoscopic colorectal surgery: A review and meta-analysis of randomised controlled studiesSurg Res Pract 2016 2016:e7543684 [Google Scholar]
[20]. Halabi WJ, Kang CY, Nguyen VQ, Carmichael JC, Mills S, Stamos MJ, Epidural analgesia in laparoscopic colorectal surgery: A nationwide analysis of use and outcomesJAMA Surg 2014 149(2):130-36. [Google Scholar]
[21]. Whiteman A, Bajaj S, Hasan M, Novel techniques of local anaesthetic infiltrationContin Educ Anaesth Crit Care Pain 2011 11(5):167-71. [Google Scholar]
[22]. Ahn SR, Kang DB, Lee C, Park WC, Lee JK, Postoperative pain relief using wound infiltration with 0.5% bupivacaine in single-incision laparoscopic surgery for an appendectomyAnn Coloproctology 2013 29(6):238-42. [Google Scholar]
[23]. Shafiq F, Hamid M, Samad K, Complications and interventions associated with epidural analgesia for postoperative pain relief in a tertiary care hospitalMiddle East J Anaesthesiol 2010 20(6):827-32. [Google Scholar]
[24]. Chan YC, Dasey N, Iatrogenic spinal epidural abscessActa Chir Belg 2007 107(2):109-18. [Google Scholar]
[25]. Ventham NT, Hughes M, O’Neill S, Johns N, Brady RR, Wigmore SJ, Systematic review and meta-analysis of continuous local anaesthetic wound infiltration versus epidural analgesia for postoperative pain following abdominal surgeryBr J Surg 2013 100(10):1280-89. [Google Scholar]
[26]. Garimella V, Cellini C, Postoperative Pain ControlClin Colon Rectal Surg 2013 26(3):191-96. [Google Scholar]
[27]. Kadam VR, Moran JL, Epidural infusions versus Transversus Abdominis Plane (TAP) block infusions: retrospective studyJ Anaesth 2011 25(5):786-87. [Google Scholar]
[28]. Niraj G, Kelkar A, Jeyapalan I, Graff-Baker P, Williams O, Darbar A, Comparison of analgesic efficacy of subcostal transversus abdominis plane blocks with epidural analgesia following upper abdominal surgeryAnaesthesia 2011 66(6):465-71. [Google Scholar]
[29]. Ganapathy S, Sondekoppam RV, Terlecki M, Brookes J, Das AS, Subramanian L, Comparison of efficacy and safety of lateral-to-medial continuous transversus abdominis plane block with thoracic epidural analgesia in patients undergoing abdominal surgery: A randomised, open-label feasibility studyEur J Anaesthesiol 2015 32(11):797-804. [Google Scholar]
[30]. Pedrazzani C, Menestrina N, Moro M, Brazzo G, Mantovani G, Polati E, Local wound infiltration plus transversus abdominis plane (TAP) block versus local wound infiltration in laparoscopic colorectal surgery and ERAS programSurg Endosc [Internet] 2016 30(11):5117-25. [Google Scholar]
[31]. Loizides S, Gurusamy KS, Nagendran M, Rossi M, Guerrini GP, Davidson BR, Wound infiltration with local anaesthetic agents for laparoscopic cholecystectomyCochrane Database Syst Rev 2014 (3):CD007049 [Google Scholar]