Solitary Giant Osteoma of Mandible
Poonam Sagar1, Kirti Jain2, Shyama Jain3, Ramanuj Bansal4
1 Senior Resident, Department of Ear, Nose and Throat, Lok Nayak Hospital, New Delhi, India.
2 Consultant, Department of Ear, Nose and Throat, MGS Hospital, Punjabi Bagh, New Delhi, India.
3 Directorate Professor and Head, Department of Pathology, Lok Nayak Hospital, New Delhi, India.
4 Senior Specialist, Department of Ear, Nose and Throat, Lok Nayak Hospital, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Poonam Sagar, C-11A, Ram Dutt Enclave, Uttam Nagar-110059, New Delhi, India.
E-mail: poonamsgr.mamc@gmail.com
Osteomas are benign osteogenic tumours characterised by the proliferation of compact, cancellous or mixed bone. Mandible is an uncommon site for solitary osteoma. Osteomas usually occur as asymptomatic swelling but may cause significant concern due to their size, problem during mastication or even sleep disturbance. Osteomas can be a part of Gardener’s syndrome, which is characterised by the multiple colonic polyposis which have high incidence of malignant degeneration. We report a case of solitary giant osteoma of mandible in 30-year-old male who presented with large swelling of lower jaw since two years. In the present case, osteoma had both extraosseous and intraosseous component that involved lower border and body of the mandible. Excision was done using oscillating saw preserving the alveolar margin of the mandible. Mandibular reinforcement was done with titanium plates. In the present case, syndromic association was ruled out with colonoscopic examination.
Colonoscopy, Mastication, Titanium
Case Report
A 30-year-old male presented with history of swelling of left jaw for past two years. Swelling first appeared as hard nodule over the lower border of left jaw and progressed gradually. There was no history of trauma and any other such swelling in the body elsewhere. There was no history of pain, difficulty in mastication and reduced mouth opening. There was no history of abdominal complaints, co-morbid conditions and family history was insignificant.
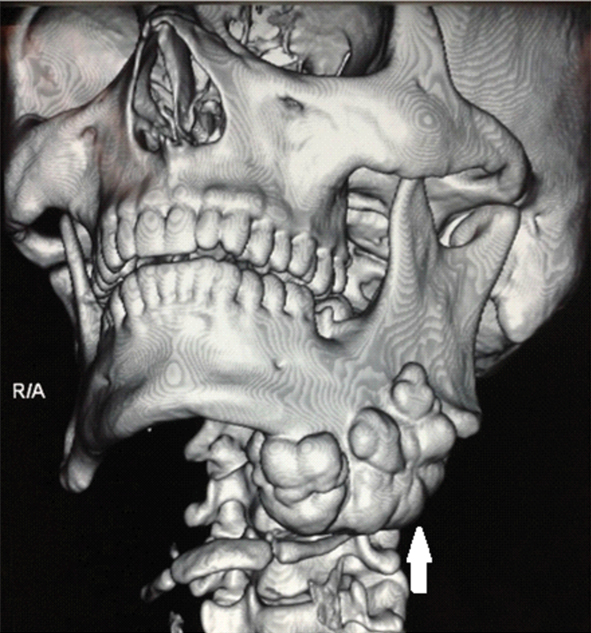
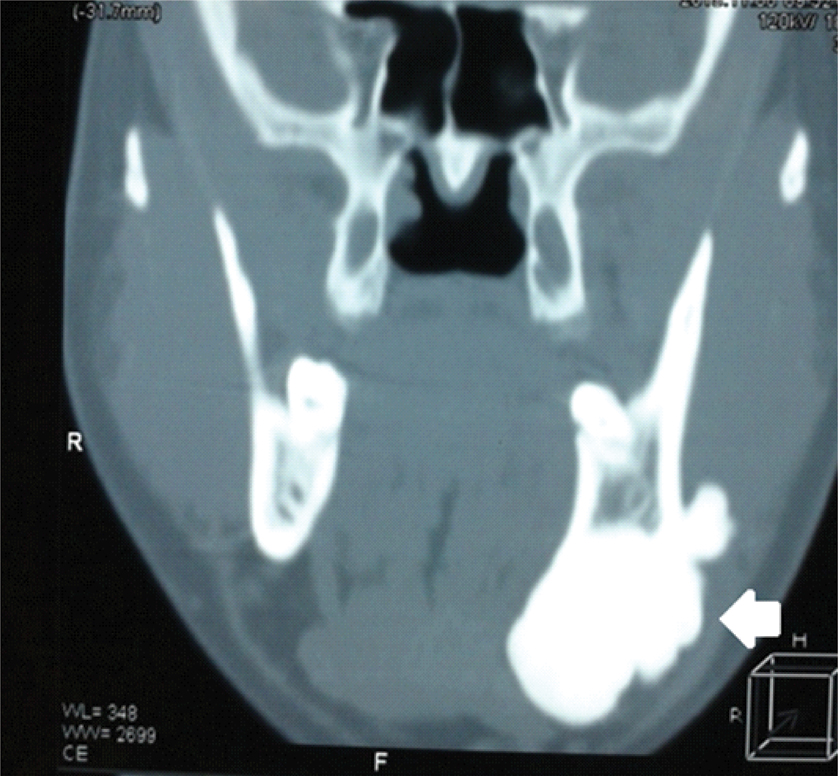
On inspection, single, oval, 7×5 cm swelling with normal overlying skin was seen along lower border of mandible on left side. On palpation, the swelling was bony hard, non-tender, well-defined, fixed to the mandible with bosselated surface. Oral cavity examination was normal with adequate mouth opening and normal dentition. Examination of nose, ear and neck did not reveal any abnormality. Computed Tomography (CT) scan showed dense sclerotic well-defined lobular lesion involving body of left mandible, measuring 67×40×49 mm in anteroposterior, transverse and vertical dimensions with no evidence of any unerupted tooth [Table/Fig-1,2]. These findings suggested non-odontogenic benign bony lesion possibly osteoma mandible or cemento-ossifying fibroma. With the probable diagnosis of osteoma mandible, patient was referred to gastroenterology department for colonoscopy to rule out colonic polyposis.
Three dimensional reconstruction image showing dense sclerotic well-defined lobular lesion involving body of left mandible, measuring 67×40×49 mm in anteroposterior, transverse and vertical dimension (white arrow).
Coronal CT scan showing large sclerotic lesion involving lower margin of body of mandible (white arrow).
As patient was concerned about such large swelling over his face, plan of excision was made on the basis of cosmetic grounds. Patient was planned for excision with transcervical approach under general anaesthesia. A curvilinear incision was made from the chin midline, extending over the swelling, well below to preserve the marginal mandibular nerve and reaching till the mastoid tip. Subplatysmal flaps were elevated. A lobulated bony lesion was seen over the lower border of left mandible involving the buccal aspect extending medially to involve lingual aspect also [Table/Fig-3]. This bony tumour was cut from the mandible taking wide margin using oscillating saw with preservation of inferior alveolar nerve, alveolar rim and dentition. The mandible was reinforced using titanium plates [Table/Fig-4]. Histopathological examination showed mature lamellar bone consistent with compact osteoma [Table/Fig-5]. Patient did well in post-operative period.
Intraoperative image showing lobulated hard bony tumour involving lower border, both lingual and buccal surface, extending up to the angle of mandible (white arrow- mandible, black arrow- osteoma).

Showing mandibular reconstruction using titanium plates preserving the alveolar margin.

Histopathology showing mature lamellar bony fragment. (H&E stain, 400X, black arrows).

Discussion
Osteomas are benign slow growing bone forming tumours. Osteomas can be classified as peripheral, central or extraskeletal. Peripheral osteoma arises from the periosteum and grows as exophytic masses. Central osteoma arises from the endosteum and grows centripetally while uncommonly extraskeletal osteomasarise from soft tissues. Osteomas are commonly found in craniofacial bones, paranasal sinuses (frontal sinus) being the most common site [1]. Osteomas are found in 1% of subjects undergoing plain sinus radiographs and in 3% of those undergoing CT scan for sinus symptoms [2]. Giant solitary osteoma of mandible is a rare entity. In a study in elderly population in India, the prevalence of osteoma was around 3% (1/29 cases) [3]. Most common sites in mandible are body, angle, condyle, coronoid process, and sigmoid notch in that order [4]. Osteomas can occur during second decade to sixth decade of life. Larrea-Oyarbide N et al., in a retrospective study of 106 cases found mean age to be 50 years [4]. Osteomas are more commonly found in male than females (1.7:1).
Osteomas may be solitary or multiple. Multiple osteomas may be associated with Gardener’s syndrome. Gardener’s syndrome is an autosomal dominant disorder, variant of familial adenomatosis coli characterised by multiple osteomas, soft tissue tumours (desmoid tumours, fibromas, epidermoid, sebaceous cyst) and colorectal polyposis. It is caused by mutation in Adenomatous Polyposis Coli (APC) gene on chromosome 5q. Colonic polyps in this syndrome are associated with high incidence of malignant degeneration reaching up to 100%. Early diagnosis is crucial, prophylactic colectomy may be required [5].
Exact aetiology of osteomas is unknown. Various theories proposed are developmental, traumatic, infectious and reactive [6-8]. In our case, no specific aetiology was found. Osteoma of mandible can present with various symptoms such as swelling, malocclusion, difficulty in mastication and even obstructive sleep apnoea depending on location of tumour [9]. Pain is not a feature of osteoma.
Osteomas are histologically divided into three categories. First is ivory or eburnated osteoma which is characterised by compact, dense bone with minimal fibrous tissue lacking Haversian system. Second is, mature osteoma also known as osteoma spongiosum composed of spongy mature bone in which bony trabeculae are divided by the conspicuous amount of fibrous tissue, containing fibroblast in different stages of maturation. Connective tissue may contain distended thin walled vessels. Third type is mixed osteoma with features typical of both ivory and mature osteoma.
Mandibular osteoma needs to be differentiated from exostoses or tori which are the bony outgrowths that continue to grow throughout the life. These are thought to be developmental or reactive in origin and are not true neoplasms. Mandibular tori found to involve lingual surface of anterior mandible, primarily in premolar region. Tori are typically pedunculated or multilobulated, broad based smooth masses. Patient with tori are usually asymptomatic unless it interferes with fitting of dentures. The other differential diagnoses are osteoid osteoma, odontoma, osteoblastoma, ossifying cementoma or osteosarcoma.
Osteomas appear as well-defined homogenous radiodense masses on CT. Three dimensional reconstruction is useful in planning excision and repair. Symptomatic osteoma requires excision. Recurrences are rare and malignant transformation has not been reported [4].
Sadeghi HM et al., reviewed literature of giant osteoma mandible and found seven cases. Their study concluded that osteoma mandible can present with symptoms such as swelling, dyspnea and dysphagia [10]. Ata ali J et al., reported large osteoma of mandible over left lateral aspect of mandible mimicking parotid swelling [11]. De souza PD et al., reported giant osteoma mandible arising from inner aspect of left ramus of mandible presenting as cervical swelling [12].
Osteomas of size >30 mm or weight >110 gm are considered as giant lesions [13]. Giant osteoma of mandible becomes important as it may interfere with mastication, cosmesis or can cause symptoms such as obstructive sleep apnea. Excision of large lesion requires consideration of post-operative function. In the present case report, osteoma involved lower border, both lingual and buccal surface of mandible, reaching till the angle of mandible and sparing the alveolar margin. Complete excision was done using oscillating saw, preserving the alveolar margin and dentition. Mandible was reinforced using titanium plates. The smaller and pedunculated lesion can be removed intraorally while the larger lesion requires transcervical approach. Mandibular reconstruction, if required can be done with titanium plating or bone graft [14].
Conclusion
Giant osteoma of mandible is a rare entity. Giant osteoma needs to be differentiated from osteoid osteoma, osteoblastoma, cementifying fibroma and malignant bone forming tumours. Complete excision is the treatment of choice if symptomatic with due consideration to the functional outcome.
[1]. Earwaker J, Paranasal sinus osteomas: a review of 46 casesSkeletal radiol 1993 22(6):417-23. [Google Scholar]
[2]. Erdogan N, Demir U, Songu M, Ozenler NK, Uluç E, Dirim B, A prospective study of paranasal sinus osteomas in 1889 cases: changing patterns of localizationLaryngoscope 2009 119(12):2355-359. [Google Scholar]
[3]. Bajpai M, Parde N, Chandolia B, Arora M, Prevalence of jaw tumors in elderly Indian population: A retrospective pathological analysis of 29 casesOral Maxillofacial Pathology J 2107 8(1):16-18. [Google Scholar]
[4]. Larrea-Oyarbide N, Valmaseda-Castellon E, Berini-Aytes L, Gay-Escoda C, Osteomas of the craniofacial region. Review of 106 casesJ Oral Pathol Med 2008 37(1):38-42. [Google Scholar]
[5]. Alexander AA, Patel AA, Odland R, Paranasal sinus osteomas and Gardner’s syndromeAnn Otol Rhinol Laryngol 2007 116(9):658-62. [Google Scholar]
[6]. Eller R, Sillers M, Common fibro-osseous lesions of paranasal sinusesOtolaryngol Clin North Am 2006 39(3):585-600. [Google Scholar]
[7]. Moretti A, Croc A, Leone O, Osteoma of maxillary sinus: case reportActa Otorhinolaryngol Ital 2004 24(4):219-22. [Google Scholar]
[8]. Kaplan I, Calderon S, Buchner A, D Agostino L, Peripheral osteoma of the mandible: a study of 10 new cases and analysis of the literatureJ Oral Maxillofa Surg 1994 52(5):467-70. [Google Scholar]
[9]. Tarsitano A, Marchetti C, Unusual presentation of obstructive sleep apnea due to a giant mandible osteoma: case report and literature reviewActaotorhinol Ital 2013 33(1):63-66. [Google Scholar]
[10]. Sadeghi HM, Shamloo N, Taghvi N, Safi Y, Aghdashi F, Ismaeilnejad M, Giant osteoma mandible causing dyspnea: A rare case presentation and review of the literatureJ Maxillofac Oral Surg 2015 14(3):836-40. [Google Scholar]
[11]. Ata-Ali J, Ata-Ali F, Giant peripheral osteoma of the mandible simulating a parotid gland tumorBraz J Otorhinolaryngol 2016 35(2):01-03. [Google Scholar]
[12]. De souza PD, Leonhardt FD, Ahumada NG, Abrahao M, Cervantes O, Giant osteoma of the mandibleBraz J Otorhinolaryngol 2015 81(1):107-808. [Google Scholar]
[13]. Cheng KJ, Wang SQ, Lin L, Giant osteomas of the ethmoid and frontal sinuses. Clinical characteristics and review of the literatureOncology letters 2013 5(5):1724-30. [Google Scholar]
[14]. Soni S, Bhargava A, Revisiting peripheral osteoma of the mandible with case series and review of the literatureIndian J Otolaryngol Head Neck Surg 2014 66(2):212-18. [Google Scholar]