Specialists in the dental field often get habituated to having a partial or biased assessment of clinical findings or disorders by virtue of practicing a niche speciality over long periods of time. This can lead to a disadvantage to the patient in terms of prognosis unless a wider and all encompassing prespective is inculcated and maintained. Often in the field of endodontics, a patient presents with a finding which leads to a terminal conclusion of extraction. However, with an aim of preserving the tooth, if various principles of treatment modalities of other branches of dentistry are employed, the prognosis can take a 360° turn for successful preservation of the tooth in the arch in complete functional state.
We present one such case of an incomplete vertical fracture in the furcation area of a mandibular molar, destined for extraction, but conserved with concomitant orthodontic banding followed by intentional surgical bicuspidisation and full coverage restoration.
Endodontics, Intentional bicuspidisation, Orthodontic banding
Case Report
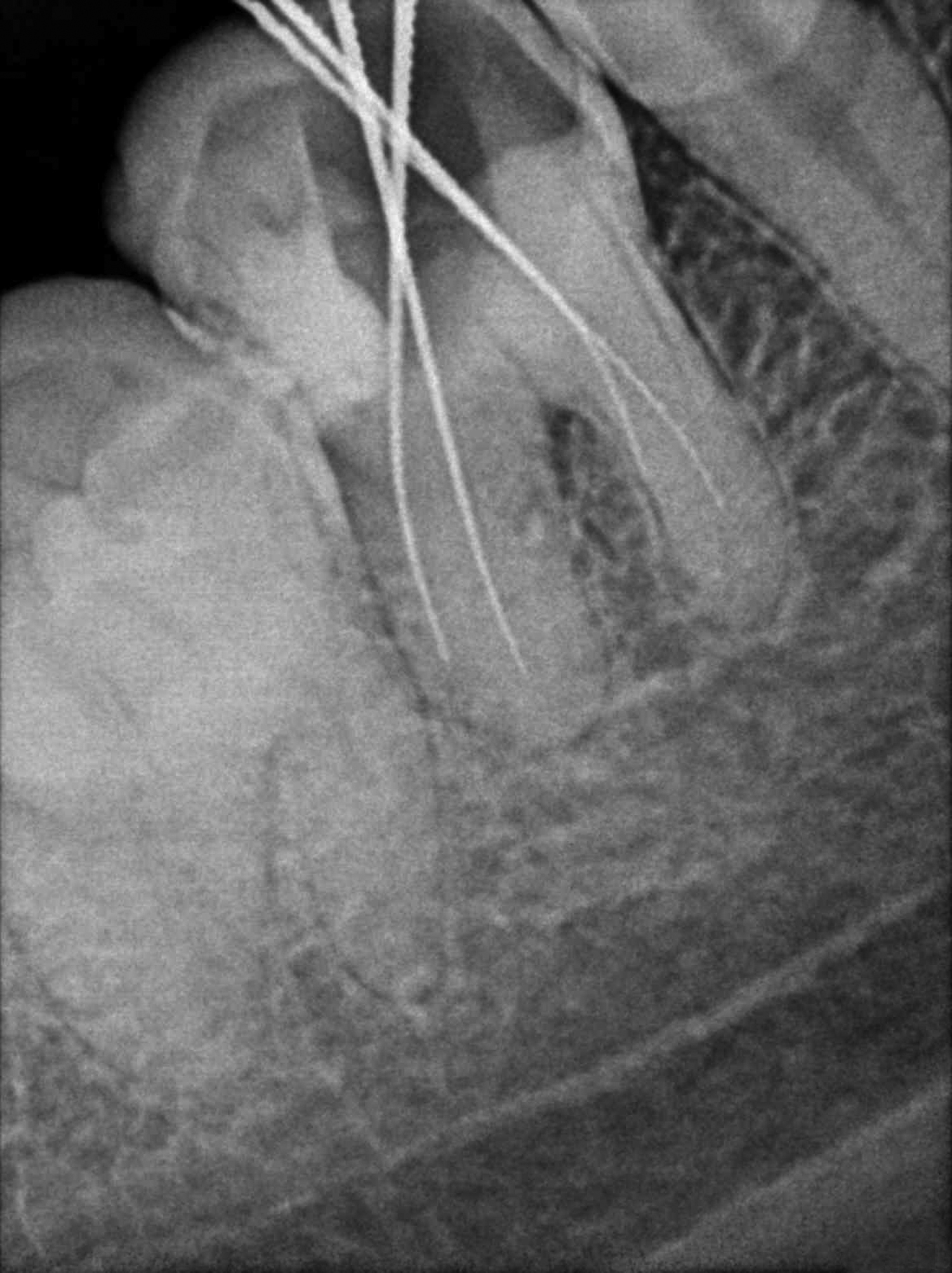
A 34-year-old male patient presented to the Department of Conservative Dentistry and Endodontics with a complaint of persistent low grade pain in right mandibular first molar since a fortnight. There was no contributory medical history or history of other dental treatment. Intraoral examination revealed caries with 45 and 46. No other teeth in the oral cavity were cariously involved, 46 showed deep mesio-occlusal caries involving the pulp and was sensitive to vertical percussion with no mobility or periodontal involvement. Vitality testing with the electric pulp tester gave a delayed response indicating irreversible pulpitis. Root canal treatment was initiated and after pulp extirpation, a rough working length estimation X-ray was taken. On this radiographic examination, an incomplete vertical fracture line involving the furcation area was noted [Table/Fig-1]. The bone support of both roots was good and not periodontally compromised in any manner. There was no periodontal or furcation involvement seen in relation to 46. A disto-occlusal composite resin restoration was planned for 45. An assessment of all findings was made and a treatment protocol was developed to achieve functional preservation of the tooth in the arch.
Diagnostic radiograph of 46 showing incomplete vertical fracture in the furcation area.
Prior to any further treatment, an orthodontic band was placed around 46 to stabilise the tooth and prevent further propogation of the fracture line [Table/Fig-2]. Then root canal therapy was resumed. Access opening was refined, and four canal orifices were located, two mesial and two distal. The working length was determined [Table/Fig-3] and the canals were cleaned and shaped using crown-down technique with hand ProtaperTM instruments to size F1. A mastercone radiograph was taken [Table/Fig-4] and the canals were obturated with lateral condensation technique at the next sitting [Table/Fig-5].
Orthodontic band placed on 46.

Working length estimation radiograph for 46.
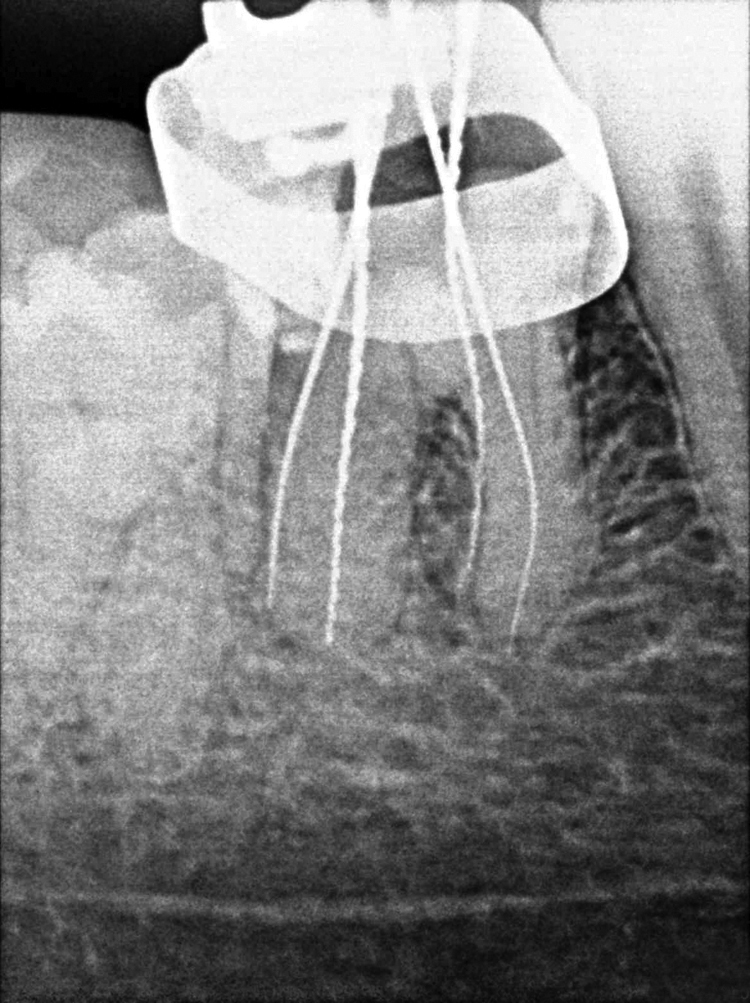
Mastercone radiograph in relation to 46.

Obturation radiograph of 46.

After two weeks, the post obturation restoration was done with composite resin (TPH, Dentsply) and then a surgical procedure was carried out for intentional bicuspidisation of the tooth. After removal of the orthodontic band, a full thickness Kirkland flap was raised with the cervicular incision extending from the distal surface of the mandibular second premolar to the midfacial surface of the mandibular second molar [Table/Fig-6]. After flap elevation, the tooth was dissected with the help of a long shank tapered fissure carbide bur to make vertical cuts towards the bifurcation area. All faces of the mesial and distal roots were rounded up and the spurs were smoothened. After irrigation with saline solution, the flap was repositioned and sutured with 3/0 silk sutures [Table/Fig-7].
Kirkland flap raised in relation to 46.
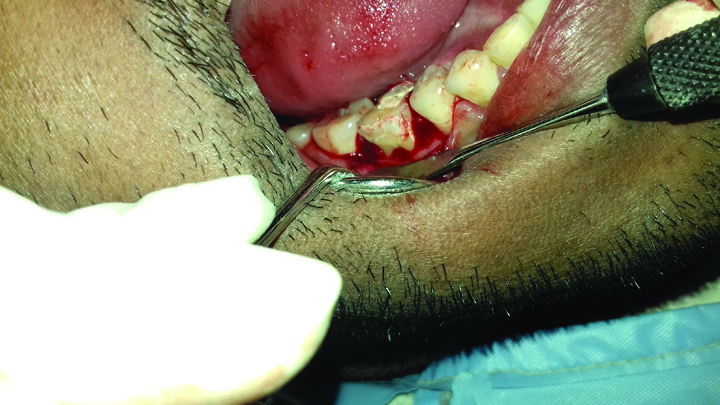
Bicuspidisation carried out and flap sutured with 46.

Six weeks after surgery, the two newly created bicuspids were prepared for receiving full stainless steel crowns [Table/Fig-8], 45 received a composite restoration for disto-occlusal caries which was restricted to enamel only. Each new bicuspid of 46 was crowned as a separate premolar tooth [Table/Fig-9,10]. After six month follow up, the patient was completely asymptomatic with no findings of periodontal involvement.
Crown cutting completed with the newly created bicuspids.

Crowns cemented on the newly created premolars of 46.

IoPAR showing cemented crowns with 46.

Discussion
From a functional and developmental point of view, the first permanent molars are the most important teeth, with a key role in occlusion. The role of first permanent molars is established in balanced occlusion [1]. Loss of first permanent molars, because of dental caries, negatively affects both arches and has adverse effects on occlusion. It is reported that early extraction of these teeth results in tilting of neighbouring teeth into the hollow spaces, super eruption of the teeth in the opposite arch, unilateral chewing, shift in midline and dental malocclusion [2].
Hence, it is imperative that all possible modalities of treatment be explored in order to retain a permanent first molar.
In the treated case, the fracture line, observed in the initial radiograph [Table/Fig-1], extended from the furcation area towards the point of bifurcation at the floor of the pulp chamber. During access cavity preparation, it was observed that the fracture line did not extend into the pulp chamber; thus, confirming the diagnosis of incomplete vertical furcation fracture. Vertical furcation fracture is a vertical crack that extends vertically from the floor of the pulp chamber in a mandibular molar towards the furcation area of the roots. The pulp is mostly involved in a vertical furcation crack and the tooth is vaguely symptomatic until the fracture line propagates and mobility sets in. The tooth rarely separates into two pieces because the tooth is held in position by the surrounding bone. The prognosis for this type of crack is fair but it depends on how deep the crack extends into the internal aspect of the tooth. The options are to treat the tooth with a root canal followed by a build up, post and crown or to extract the tooth [3]. Several classifications have been proposed to better explain vertical tooth fractures [4,5] (by Leubke and others), but there is scant mention in literature of vertical fractures restricted to the furcation area with incomplete progression of the fracture line.
Placement of an orthodontic band was done to achieve stabilisation and to prevent further progression of the fracture line. It enabled greater convenience to the operator during root canal treatment. It is a modality that is both practical and convenient to the clinical presentation of an incomplete fracture line in a molar requiring root canal therapy.
Bicuspidisation of molars is a less commonly used technique of endodontic surgery. The increased awareness and desire of patients to maintain their dentition has prompted clinicians to attempt conservation and preservation of teeth which are usually destined to be extracted. Periodontally compromised teeth with severe bone loss at the furcation area are often retained with the bicuspidisation procedure so that, there is conservation of the alveolar ridge.
Farshchian F and Kaiser DA have reported success of molar bicuspidisation [6]. They state that the success of bicuspidisation depends on three factors:
Stability, adequate bone support and, the individual tooth section;
Absence of severe root fluting of the distal aspect of the mesial root or mesial aspect of the distal root;
Adequate separation of the mesial and distal roots, to enable the creation of an acceptable embrasure for effective oral hygiene.
Indications for bicuspidisation include root fracture, severe bone loss affecting one or more roots, Class II or III furcation invasions or involvements, inability to successfully treat and fill a canal, severe root proximity inadequate for a proper embrasure space and root trunk fracture or decay with invasion of the biological width.
However, bicuspidisation should be avoided when there is poor oral hygiene, the furcation is deep and the roots are fused together or if the retained roots are endodontically untreatable.
A 10 year retrospective study by Park SY et al., studied the factors affecting the prognosis of resected molars [7]. They found the failure rate to be 29.8% in the 402 cases observed at one year follow up. The principle factor contributing to failure was identified as greater than 50% bone loss secondary to periodontal disease. It has been proposed that, it is a good guideline for teeth to have greater than 50% bone support when root resection is the considered treatment choice.
According to Newell DH, the advantage of the bisection is the retention of some or the entire tooth [8]. However, the disadvantage is that the remaining root or roots must undergo endodontic therapy and the crown must undergo restorative and prosthodontic management.
In the case reported, various aspects of occlusal function such as location and size of contacts and the steepness of cuspal inclines may have played a significant role in causing the fracture. During treatment, occlusal contacts were reduced in size and repositioned more favourably. Success of root resection and separation procedures depends to a large extent on proper case selection. In this case, the roots of the involved tooth were adequate in length and periapically healthy with no furcation involvement, and hence, bicuspidisation technique was preferred. Use of full metal crown restoration was preferred as it increases the stress bearing capacity. It is a complete protective and functional solution, making it successful in a wide range of clinical situations when tooth form or alignment is not ideal.
Langer B et al., reported a 38% failure rate for the resected molars over a 10 year period [9]; 26% of failures were due to periodontal problems. Buhler H reported that 32.1% of resected molars failed, and 44% of failures were related to periodontal problems [10]. According to the standardised reports on root resection of Buhler H, 89% of root-resected teeth survived over a seven year period. In this study, the failure rate of all molars over a 10 year period was 29.8%. Blomlof L et al., showed similar results, in that 32% of molars failed over a 10 year period; 80% of the failed molars were lost because of periodontal or endodontic periodontal lesions [11]. They revealed that the patient sample was prone to periodontitis, which resulted in a large number of periodontal failures. However, Carnevale G et al., reported a 6.9% failure rate over a 10 year period, which was lower than this study [12]. This difference might be because the inclusion criteria and maintenance program in Carnevale G et al., study was strict [12].
Conclusion
While every dental speciality is a niche field unto itself, its redeeming quality is without a doubt the extent of its contribution towards a consolidated healthy oral cavity. The prognosis of any speciality treatment plan can greatly benefit from the application of principles of other specialities and the authors hope that this has been aptly demonstrated by the multidisciplinary approach in the preservation of the molar with incomplete vertical fracture.
[1]. Cağlaroğlu M, Kilic N, Erdem A, Effects of early unilateral first molar extraction on skeletal asymmetryAm J Orthod Dentofacial Orthop 2008 134(2):270-75.10.1016/j.ajodo.2006.07.03618675209 [Google Scholar] [CrossRef] [PubMed]
[2]. Rebellato J, Asymmetric extractions used in the treatment of patients with asymmetriesSemin Orthod 1998 4(3):180-88.10.1016/S1073-8746(98)80019-4 [Google Scholar] [CrossRef]
[3]. Cohen S, Blanco L, Beeman L, Vertical root fractures-clinical and radiographic diagnosisJ Am Dent Assoc 2003 134(4):43410.14219/jada.archive.2003.019212733776 [Google Scholar] [CrossRef] [PubMed]
[4]. Remya C, Indiresha HN, George JV, Dinesh K, Vertical root fractures: A reviewInt J Contemp Dent Med Rev 2015 2015:220115 [Google Scholar]
[5]. Principles and practice of endodontics 2008 4th edM Torabinejad and RE Walton editors [Google Scholar]
[6]. Farshchian F, Kaiser DA, Restoration of the split molar: bicuspidizationAm J Dent 1988 1(1):21-22. [Google Scholar]
[7]. Park SY, Shin SY, Yang SM, Kye SB, Factors influencing the outcome of root-resection therapy in molars: a 10-year retrospective studyJ Periodontol 2009 80(1):32-40.10.1902/jop.2009.08031619228087z [Google Scholar] [CrossRef] [PubMed]
[8]. Newell DH, Diagnosing molar furcation invasionsJ Indiana Dent Assoc 1999 78(1):21-25.:27 [Google Scholar]
[9]. Langer B, Stein SD, Wagenberg B, An evaluation of root resections. A ten-year studyJ Periodontol 1981 52(12):719-22.10.1902/jop.1981.52.12.7196948102 [Google Scholar] [CrossRef] [PubMed]
[10]. Buhler H, Evaluation of root-resected teeth. Results after 10 yearsJ Periodontol 1988 59(12):805-10.10.1902/jop.1988.59.12.8053066890 [Google Scholar] [CrossRef] [PubMed]
[11]. Blomlof L, Jansson L, Appelgren R, Ehnevid H, Lindskog S, Prognosis and mortality of root-resected molarsInt J Periodontics Restorative Dent 1997 17(2):190-201. [Google Scholar]
[12]. Carnevale G, Di Febo G, Tonelli MP, Marin C, Fuzzi M, A retrospective analysis of the periodontal-prosthetic treatment of molars with interradicular lesionsInt J Periodontics Restorative Dent 1991 11(3):189-205. [Google Scholar]