Hydrochlorothiazide Sensitised Acetazolamide induced Bilateral Angle Closure Glaucoma with Choroidal Detachment after Cataract Surgery
Chitaranjan Mishra1, T Sundar2, Srinivas Sanjeev3, Naresh Babu4, Ramasamy Kim5
1 Retina Fellow, Aravind Eye Hospital, Anna Nagar, Madurai, Tamil Nadu, India.
2 Medical Officer, Aravind Eye Hospital, Salem, Tamil Nadu, India.
3 Resident, Department of Ophthalmology, Aravind Eye Hospital, Salem, Tamil Nadu, India.
4 Senior Medical Officer, Aravind Eye Hospital, Anna Nagar, Madurai, Tamil Nadu, India.
5 Chief Medical Officer, Aravind Eye Hospital, Anna Nagar, Madurai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Chitaranjan Mishra, Aravind Eye Hospital, Anna Nagar, Madurai-625020, Tamil Nadu, India.
E-mail: drchitaranjan.gnec@gmail.com
Sulfonamide (Sulfa) derived medications causing bilateral secondary angle closure glaucoma with choroidal effusion is a known but rare clinical entity. Both acetazolamide and hydrochlorothiazide belong to sulfonamide group of drugs and have been separately reported in literature causing secondary angle closure glaucoma. However, administration of both these drugs causing this side effect in the same patient has not been reported previously. We report a case of 58-year-old male patient with hypertension and diabetes who developed bilateral angle closure glaucoma with choroidal detachment after administration of oral acetazolamide tablets during routine cataract surgery. The possible role of hydrochlorothiazide, a systemic antihypertensive, which the patient was on for three years, potentiating the adverse effect of acetazolamide is postulated since both these drugs are reported to cause this clinical entity. The patient was managed successfully with conservative antiglaucoma measures and cessation of the offending drugs. Hence, in all cases of secondary angle closure glaucoma, a thorough review of drugs of the patient is warranted. Identification of sulfa drugs and their discontinuation will result in prompt recovery of symptoms. Refraction, gonioscopy, fundoscopy and Ultrasonography (USG) B-scan will help in diagnosis and documentation of the clinical presentations.
Drug induced, Idiosyncratic response, Sulfonamide
Case Report
A 58-year-old male patient was diagnosed with left eye (OS) mature intumescent cataract and was posted for OS Manual Small Incision Cataract Surgery (MSICS). He was a known case of systemic hypertension on treatment with antihypertensive drugs including oral hydrochlorothiazide tablets for three years and a known diabetic on treatment for one month. His right eye (OD) was suggestive of Immature Senile Cataract with grade 2 Nuclear Sclerosis (IMSC, NS 2). Best Corrected Visual Acuity (BCVA) in OD was 6/6 and OS was Hand Movements (HM). All other anterior segment findings were Within Normal Limits (WNL) in both eyes (OU). Intraocular Pressures (IOP) in OU were 13 mmHg. OD fundus was WNL. USG B-scan in OS revealed anatomically normal posterior segment. Axial length in OD was 22.61 mm and in OS was 22.65 mm. He was prescribed tablet acetazolamide 250 mg for 30 minutes before OS surgery to counter any intraoperative positive vitreous pressure. He underwent an uneventful MSICS under sub-Tenon’s anaesthesia with Posterior Chamber Intraocular Lens (PCIOL) implantation in OS. After six hours of surgery the slit lamp examination revealed in the bag PCIOL with minimal postoperative inflammation. Rest of the anterior segment findings and fundus findings were WNL in OU. On the first postoperative day at 8 AM his visual acuity in OS was 6/12. Corneal epithelial oedema (2+), shallow peripheral anterior chamber and raised IOP (26 mmHg) was noted in OS. Anterior segment of OD was unchanged and IOP of OD was 16 mmHg. Fundus was WNL in OU. In view of raised IOP, he was prescribed tablet acetazolamide 250 mg stat and topical brimonidine and timolol combination twice a day in addition to regular postoperative steroid-antibiotic eye drops in OS. At 8 pm on postoperative day one his BCVA in OD was 6/6 and OS was 6/12. Anterior segment examination revealed conjunctival chemosis and circumcorneal congestion in OU. Corneal epithelial oedema increased in OS though OD cornea was clear. Anterior chamber of both the eyes were shallow with doubtful pupillary block [Table/Fig-1]. IOP of OD was 18 mmHg and OS was 28 mmHg. To combat the probable mechanism of pupillary block, both eyes Yttrium Aluminium Garnet (YAG) peripheral iridotomy was done. On postoperative day two, in spite of patent peripheral iridotomies, both eyes revealed very shallow angle of anterior chambers. Fundoscopy of OD revealed normal appearing posterior pole and OS revealed choroidal detachment [Table/Fig-2a,b]. However, USG B-scan of OU revealed peripheral choroidal detachments [Table/Fig-2c]. In addition, the thickness of retino-choroidal-scleral complex was increased (OD 2.3 mm, OS 2.8 mm). At this time, a drug induced phenomena causing secondary pupillary block was strongly suspected and his drugs were reviewed. Systemic antihypertensive hydrochlorthiazide and antiglaucoma drug acetazolamide were suspected to be causing idiosyncratic reactions resulting in choroidal effusion and ocular findings. Hence, these drugs were discontinued. In addition to steroid-antibiotic drops and topical antiglaucoma medications, he was started on systemic prednisolone 30 mg once a day. The next day (postoperative day three) his anterior segment findings improved minimally, though posterior segments were unchanged. During the review check up, on postoperative day 10, his angle of anterior chambers was normal depth OU [Table/Fig-3a]. Intraocular pressure was 14 mmHg OU. Fundoscopy revealed OU completely resolved choroidal detachments which were confirmed on USG B-scan [Table/Fig-3b].
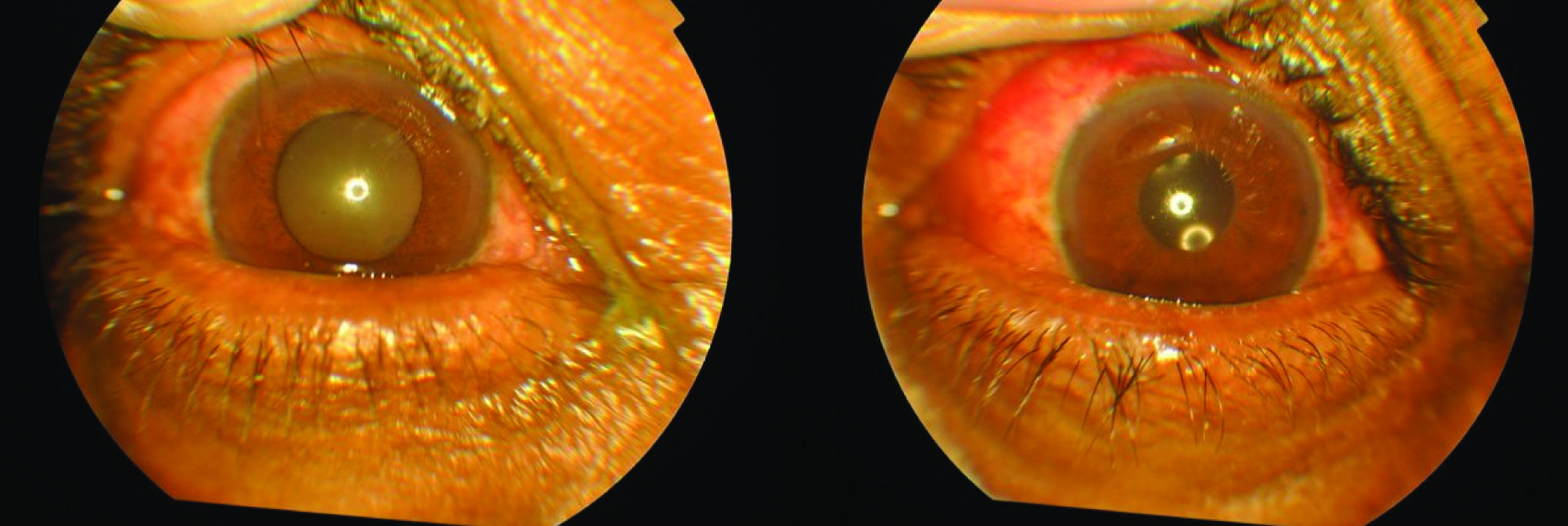
Postoperative day one: anterior segment examination of both eyes. Right eye is showing immatutre cataract. In left eye, posterior chamber intraocular lens can be seen. Both eyes angle of anterior chamber is shallow. Note the minimal subconjunctival haemorrhage from cataract surgery in the left eye.
Postoperative day two: a) Fundus examination of right eye revealed normal appearing posterior pole. Left eye revealed choroidal detachment; b) Fundus of left eye showing peripheral choroidal detachment; c) USG B-scan of both eyes suggestive of peripheral choroidal detachments.

Postoperative day 10: a) Anterior segment of both eyes suggestive of normal depth of anterior chamber; b) USG B-scan of both eyes suggestive of anatomically normal posterior segment (resolved choroidal detachments).

Discussion
Sulfonamide derivatives include antibiotics, anticonvulsants, diuretics (antihypertensives and for treatment of congestive heart failure) and various Carbonic Anhydrase Inhibitors (CAI) e.g., topiramate, acetazolamide and dorzolamide. These groups of drugs have been reported to cause transient myopia, ciliary body oedema, shallow anterior chamber, choroidal effusion and detachment and rarely anterior uveitis and optic disc oedema [1-3]. Most of these drugs including topiramate, acetazolamide and hydrochlorothiazide were found to have probable Naranjo scores of 5-8 and likely bilateral Angle Closure Glaucoma (ACG) score (more than or equal to 4) [4]. Topiramate is most often reported in literature to cause the above mentioned side effects [1,4,5]. The number of reports of hydrochlorothiazide or acetazolamide causing these side effects is limited in the literature [1,3,5-12]. However, we could not find any report of these above mentioned side effects in a patient who is administered both hydrochlorothiazide and acetazolamide. This case is the first report of acute bilateral angle closure with choroidal effusion and detachment in a patient on both hydrochlorothiazide and acetazolamide. There are previous reports of bilateral angle closure glaucoma with choroidal effusion in the setting of cataract surgery, which indicates that this type of intervention may play a part in the reactions, unlike the other clinical settings in which acetazolamide is used [3,5,11,12].
The exact mechanism of development of these ocular complications towards sulfa drugs remains unknown. The proposed theory is an idiosyncratic reaction resulting in eicosanoid metabolism causing ciliary body oedema resulting in choroidal effusion, forward rotation of lens and zonular relaxation [1,4,12]. The later is the reason for transient myopia and the former two are reasons for angle closure glaucoma. Reports on combination of sulfa group of drugs causing these ocular side effects are rare. Lee GC et al., have reported a case in their series of three cases and they ascribed the mechanism to be prior sensitisation of the patient to hydrochlorothiazide and have emphasised to stop all the sulfa drugs if the patient develops similar complications [1]. We propose a similar theory of prior sensitisation of the patient to hydrochlorothiazide and the acute idiosyncratic reaction of acetazolamide resulted in these complications.
While treating these patients, a thorough review of the drugs should be made and the offending drug(s) must be stopped. Supportive treatment includes topical antiglaucoma medications and systemic mannitol if the IOP remains very high. Regular postoperative steroid-antibiotic drops to be continued in cataract operated cases. Role of systemic steroids remains debatable however some cases have reported positive outcomes with additional steroid treatment [5]. In this case also we got a prompt recovery due to addition of oral prednisolone.
Conclusion
The ocular events in this case were most probably due to the idiosyncratic reactions of combination of hydrochlorothiazide and acetazolamide. In all cases of secondary angle closure glaucoma, the physician should do a thorough review of drugs of the patient. Identification of sulfa drugs and their discontinuation will result in prompt recovery of symptoms. Refraction, gonioscopy, fundoscopy and USG B-scan will help in diagnosis and documentation of the clinical presentations.
[1]. Lee GC, Tam CP, Danesh-Meyer HV, Myers JS, Katz LJ, Bilateral angle closure glaucoma induced by sulphonamide-derived medicationsClin Exp Ophthalmol 2007 35(1):55-58.10.1111/j.1442-9071.2006.01365.x17300572 [Google Scholar] [CrossRef] [PubMed]
[2]. Acharya N, Nithyanandam S, Kamat S, Topiramate-associated bilateral anterior uveitis and angle closure glaucomaIndian J Ophthalmol 2010 58(6):557-59.10.4103/0301-4738.7170020952855 [Google Scholar] [CrossRef] [PubMed]
[3]. Malagola R, Arrico L, Giannotti R, Pattavina L, Acetazolamide-induced cilio-choroidal effusion after cataract surgery: unusual posterior involvementDrug Des Devel Ther 2013 7:33-36.10.2147/DDDT.S3832423378740 [Google Scholar] [CrossRef] [PubMed]
[4]. Murphy RM, Bakir B, O’Brien C, Wiggs JL, Pasquale LR, Drug-induced bilateral secondary angle-closure glaucoma: a literature synthesisJ Glaucoma 2016 25(2):e99-105.10.1097/IJG.000000000000027025943730 [Google Scholar] [CrossRef] [PubMed]
[5]. Mancino R, Varesi C, Cerulli A, Aiello F, Nucci C, Acute bilateral angle closure glaucoma and choroidal effusion associated with acetazolamide administration after cataract surgeryJ Cataract Refract Surg 2011 37(2):415-17.10.1016/j.jcrs.2010.12.03221241929 [Google Scholar] [CrossRef] [PubMed]
[6]. Geanon JD, Perkins TW, Bilateral acute angle-closure glaucoma associated with drug sensitivity to hydrochlorothiazideArch Ophthalmol 1995 113(10):1231-32.10.1001/archopht.1995.011001000190127575249 [Google Scholar] [CrossRef] [PubMed]
[7]. Roh YR, Woo SJ, Park KH, Acute-onset bilateral myopia and ciliochoroidal effusion induced by hydrochlorothiazideKorean J Ophthalmol 2011 25(3):214-17.10.3341/kjo.2011.25.3.21421655050 [Google Scholar] [CrossRef] [PubMed]
[8]. Chen SH, Karanjia R, Chevrier RL, Marshall DH, Bilateral acute angle closure glaucoma associated with hydrochlorothiazide-induced hyponatraemiaBMJ Case Rep 2014 pii:bcr201420669010.1136/bcr-2014-20669025477363 [Google Scholar] [CrossRef] [PubMed]
[9]. Kronning E, Transient myopia following the use of acetazolamideActa Ophthalmol (Copenh) 1957 35(5):478-84.10.1111/j.1755-3768.1957.tb02240.x13497648 [Google Scholar] [CrossRef] [PubMed]
[10]. Fan JT, Johnson DH, Burk RR, Transient myopia, angle closure glaucoma, and choroidal detachment after oral acetazolamideAm J Ophthalmol 1993 115(6):813-14.10.1016/S0002-9394(14)73654-2 [Google Scholar] [CrossRef]
[11]. Parthasarathi S, Myint K, Singh G, Mon S, Sadasivam P, Dhillon B, Bilateral acetazolamide-induced choroidal effusion following cataract surgeryEye 2007 21:870-72.10.1038/sj.eye.670274117293785 [Google Scholar] [CrossRef] [PubMed]
[12]. Senthil S, Garudadri C, Rao HB, Maheshwari R, Bilateral simultaneous acute angle closure caused by sulphonamide derivatives: a case seriesIndian J Ophthalmol 2010 58(3):248-52.10.4103/0301-4738.6265720413935 [Google Scholar] [CrossRef] [PubMed]