Pregnancy is a physiological state associated with varied biochemical and maternal adaptation in response to physical stimuli provided by foetus and placenta [1]. HDP affect 6-8% of all pregnancies [2] and along-with haemorrhage and infection, they form a complex triad, contributing immensely to maternal morbidity and mortality [1,3].
Hypertensive disorders of pregnancy, particularly pre-eclampsia, are responsible for 10% to 15% of maternal deaths [4]. In developing countries, incidence of pre-eclampsia and its morbidity is much higher as compared to high income countries. Over the years, maternal deaths due to pre-eclampsia have been significantly reduced by early diagnosis and management in developed countries; on the contrary it is still responsible for 19% of annual maternal deaths in developing countries including India [5].
Though exact aetio-pathogenesis of pre-eclampsia is unknown, multiple factors have been implicated to have a role in it; the factors being abnormal placental implantation, endothelial dysfunction, maternal immunological tolerance, cardiovascular, genetic, nutritional and environmental factors [6]. Amongst these, endothelial dysfunction is considered to be most important factor resulting in mild to moderate microangiopathy of target organs, leading to excessive leakage of LDH in serum [5-7]. Thus presence of LDH signifies tissue damage and haemolysis [8]. Elevated LDH levels in pre-eclampsia reflect severity as well occurrence of complications in pre-eclampsia [6,9,10].
It has been studied in recent times that pre-eclamptic patients with higher levels of LDH are susceptible to have poor maternal and foetal upshots [6,8,9,11,12]. Identification of such high risk patients with elevated LDH levels, along with close monitoring and prompt management may prevent these complications, with subsequent drop in feto-maternal morbidity and mortality. Most of the available data in literature till date, are smaller studies, spanning over smaller duration [6,8,9,11-18].
The present study was conducted to correlate LDH levels with blood pressure ranges and maternal and foetal outcome in women with gestational hypertension, pre-eclampsia.
Materials and Methods
A prospective case-control study was conducted, in Department of Obstetrics and Gynaecology in collaboration with Department of Pathology and Biochemistry, Vardhaman Mahavir Medical College and Safdarjang Hospital, New Delhi, India, over 18 months, from September 2014 to March 2016. One hundred fifty women, after 28 weeks of gestation, with HDP as cases, and another 150 normotensive pregnant women as controls, were enrolled in the study after taking their written informed consent. This study was approved by Institutional Ethical Committee. Women were selected consecutively on the basis of definitions given by National High Blood Pressure Education Program (NHBPEP 2000) [10] and ACOG criteria [3]. Following the ACOG criteria, cases were further divided into following subgroups-women with gestational hypertension, mild pre-eclampsia, severe pre-eclampsia and eclampsia [3]. All the women were then categorised according to serum LDH levels into mild (<600 IU/L), moderate (600-800 IU/L) and severe (>800 IU/L) categories.
Exclusion criteria were chronic hypertension, diabetes mellitus, chronic liver renal disease, epilepsy, thyroid disease, smoking, alcohol and drug intake, hyperuricaemia, symptomatic infectious diseases, multiple gestation, and unwillingness to participate.
On the first visit to the hospital, after comprehensive history and physical examination, the included women were subjected to routine investigations for HDP (haemoglobin, bleeding time, clotting time, blood sugar, liver and kidney function test). Then, about 2 mL of venous blood was drawn under aseptic conditions in a plain vial (before initiation of medical treatment) from the women in both the groups, serum was separated by centrifugation and estimation of serum LDH was done.
Concentration of serum LDH, was analysed by using analytical kits from HITACHI analyser 902 (hospital supply) in clinical biochemistry unit. This method is based on the reduction of pyruvate to lactate in the presence of NADH (nicotinamide adenine dinucleotide, reduced form) by the action of LDH enzyme. Pyruvate that remains unchanged reacts with 2,4-dinitrophenylhyrazone, which was then determined calorimetrically in an alkaline medium. The rate of fall of NADH is directly proportional to the activity of LDH. The rate of formed NAD+ is determined by the decrease in its absorbance.
All women were followed through their antenatal period till 72 hours post-delivery (along-with their newborns) and subsequently till 12 weeks postpartum.
Outcomes measured were demographic and maternal characteristics, serum LDH values, its correlation with blood pressure and feto-maternal outcome and correlation of blood pressure with other biochemical markers (liver and kidney function tests).
Statistical Analysis
Sample size calculation and data analysis: To detect a significant difference from 90-95%, correlation among cases and controls, with a power of 80%, and incidence of pre-eclampsia being 5-8%, two tailed α of 5% required a minimum of 150 women in each group, thus achieving a sample size of 300 as deduced through epi info software. All data were entered on predesigned case proforma and deciphered at the end of the study using SPSS 21.0 version. Quantitative variables were compared using unpaired t-test/mann-Whitney test between two groups, and ANOVA/Kruskal Wallis test between more than two groups. Qualitative variables were correlated using chi-square/Fisher exact test. ROC curve was used to assess the predictability of various factors for diagnosing severity of hypertension. Pearson/Spearsman correlation coefficient was used to assess correlation between various quantitative parameters. The level of significance was set at <0.05 for all variables.
Results
Amongst 300 women included in the study, 123 women had LDH levels <600 IU/L, 59 had LDH levels 600-800 IU/L and 118 women had >800 IU/L. Out of the total 150 cases, 47 had gestational hypertension, 65 had mild pre-eclampsia and 38 had severe pre-eclampsia. The mean age of women in hypertensive group was 25.06±4.13 years, while that in normotensive group was 24.38±3.8 years. Thus, both were comparable statistically (p-value=0.153). Most of the patients belonged to lower and lower middle class, hailing from rural (37.33%) and slum (47.67%) areas [Table/Fig-1].
Comparison of demographic and maternal characteristics of the study population.
| S. NO. | Characteristics | Hypertensive Group (%) | Normotensive group (%) | Total (%) | p-value |
|---|
| 1. | Age (years) |
| 20 | 18 (12.00%) | 22 (14.67%) | 40 (13.33%) | 0.451 |
| 21-30 | 119 (79.33%) | 120 (80.0%) | 239 (79.67%) |
| >30 | 13 (8.67%) | 8 (5.33%) | 21 (7.00%) |
| 2. | Parity |
| Multigravida | 72 (48.00%) | 78 (52.00%) | 150 (50.00%) | 0.23 |
| Primigravida | 78 (52.00%) | 72 (48.00%) | 150 (50.00%) |
| 3. | Residence |
| Urban | 21 (14.00%) | 26 (17.33%) | 47 (15.67%) | 0.729 |
| Slum | 73 (48.67%) | 70 (46.67%) | 143 (47.67%) |
| Rural | 56 (37.33%) | 54 (36.00%) | 110 (36.67%) |
| 4. | Socioeconomic status (modified Kuppuswami Upper Scale) |
| Upper | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | 0.192 |
| Upper middle | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) |
| Middle | 37 (24.67%) | 29 (19.00%) | 66 (22.00%) |
| Lower middle | 92 (61.33%) | 89 (59.33%) | 181 (60.33%) |
| Lower | 21 (14.00%) | 32 (21.33%) | 53 (17.67%) |
The mean serum LDH levels in hypertensive group was 1011.81±539.31 IU/L, while it was 555.24±237.69 IU/L in the normotensive group (p-value<0.0005). Analysing the cases with respect to serum LDH values, the mean LDH value was much lower in women with gestational hypertension and mild pre-eclampsia (n=112; 958.52±501.75 IU/L), when compared to women with severe pre-eclampsia (n=38; 1168.9±618.13 IU/L) This difference was statistically significant (p-value=0.017) [Table/Fig-2].
Correlation of Serum LDH and Blood Pressure.
| LDH Levels In Study Population | p-valuea | p-valueb |
|---|
| Mean LDH value |
|---|
| Hypertensive group (n=150) | | 0.017 | <0.0005 |
| Gestational hypertension and mild pre-eclampsia | 958.52±501.75 IU/L |
| Severe pre-eclampsia | 1168.9±618.13 IU/L |
| Normotensive Group (n=150) | 555.24±237.69 IU/L | |
p-valuea=level of significance for severity of hypertension
p-valueb= level of significance for mean LDH values among cases and controls
It was noted that in women with LDH levels above 800 IU/L (118/300) 28 women had systolic BP>160 and above (23.7%) and 40 women had diastolic BP 110 and above (11.01%). Studying the association of LDH with increase in blood pressure, the rise in LDH was found to be weakly correlated with SBP (correlation coefficient=0.24), but strongly correlated with DBP (correlation coefficient=-0.12) [Table/Fig-3].
Distribution of study population according to serum LDH levels and blood pressure.
| Blood pressure | <600IU/L | 600-799 IU/L | ≥ 800 IU/L | Correlation coefficient |
|---|
| Systolic blood pressure |
| <140 mmHg | 103 | 27 | 20 | 0.24 |
| 140-159 mmHg | 13 | 30 | 70 |
| >160 mmHg | 7 | 2 | 28 |
| Diastolic blood pressure |
| < 90 mmHg | 106 | 31 | 13 | -0.12 |
| 90-109 mmHg | 13 | 24 | 65 |
| >110 mmHg | 4 | 4 | 40 |
Analysing the maternal complications in the hypertensive group, 8 (8.08%) women developed eclampsia, 3 (2.00%) had placental abruption and 1 (0.67%) had HELLP syndrome. Noteworthy was the fact, that all these women had LDH values >800 IU/L. However, none of these complications were seen in the normotensive group. Also, as the levels of LDH increased in both the groups, the percentage of women delivering by LSCS increased (p-value=0.001) [Table/Fig-4].
Correlation of Serum LDH with maternal complications and mode of delivery.
| S.No | | Normotensive group | Hypertensive Group | p-value |
|---|
| 1. | Complications | <600 IU/L | 600-800 IU/L | >800 IU/L | <600 IU/L | 600-800 IU/L | >800 IU/L |
|---|
| Eclampsia | 0 | 0 | 0 | 0 | 0 | 8 | 0.113 |
| Placental Abruption | 0 | 0 | 0 | 0 | 0 | 3 | 0.455 |
| HELLP syndrome | 0 | 0 | 0 | 0 | 0 | 1 | 0.772 |
| 2. | Mode of delivery |
| NVD | 103 (100%) | 25 (92.6%) | 18 (90%) | 20 (100%) | 29 (90%) | 86 (87.8%) | 0.001 |
| LSCS | 0 (0%) | 2 (7.4%) | 2 (10%) | 0 (0%) | 3 (10%) | 12 (12.3%) |
The gestational age at delivery of women in hypertensive group (37.34±2.55 weeks) was significantly lesser than that of women in normotensive group (38.41±1.74 weeks) (p-value<0.0005).
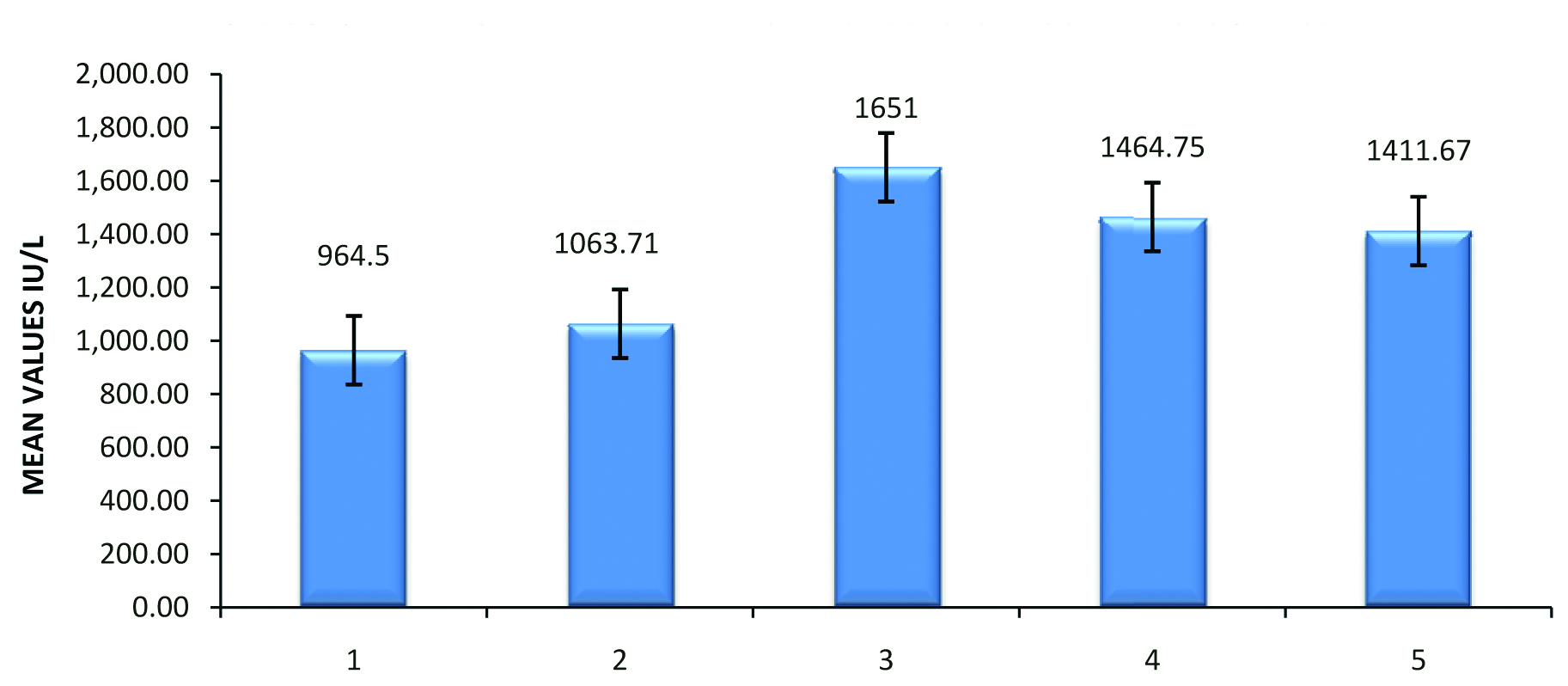
The women with LBW neonates had higher levels of LDH (1058.88±575.19 IU/L) than women with average birth weight (975.82±510.71 IU/L) [Table/Fig-5]. Also, it was seen that as the levels of serum LDH increased, the prognosis of foetus worsened and chances of NICU admission, IUD and neonatal death increased [Table/Fig-6].
Correlation of serum LDH with foetal outcome.
| FoetalOutcome | LDH value (IU/L) | p-valuea | p-valueb |
|---|
| Normotensive Group (%) | Hypertensive Group (%) |
|---|
| <600 | 600-800 | >800 | <600 | 600-800 | >800 |
|---|
| POG | | |
| Preterm | 1 (0.97%) | 1 (3.8%) | 4 (20%) | 7 (40.9%) | 13 (34.5%) | 27 (27.3%) | 0.402 | <0.0005 |
| Term | 103 (99%) | 25 (96.2%) | 16 (80%) | 13 (59.1%) | 19 (65.5%) | 71 (72.7%) |
| Birth weight | | |
| LBW | 0 (0%) | 0 (0%) | 2 (10%) | 12 (54.6%) | 9 (28.1%) | 44 (44.4%) | 0.227 | <0.0005 |
| Average | 103 (100%) | 27 (100%) | 18 (90%) | 8 (45.5%) | 23 (71.9%) | 54 (55.6%) |
| Still birth | 0 | 0 | 0 | 0 | 0 | 6 (4%) | 0.076 | <0.0005 |
| Neonatal death | 0 | 0 | 0 | 0 | 0 | 3 (2%) |
| NICU admission | 0 | 0 | 0 | 0 | 0 | 24 (16%) |
| Alive+well | 103 (100%) | 27 (100%) | 20 (100%) | 0 | 0 | 117 (78%) |
p-valuea=level of significance among cases
p-valueb=level of significance among cases and controls
Association of LDH with foetal outcome.
1. Alive and well; 2. NICU admission; 3. Fresh still birth; 4. Macerated still birth; 5. Neonatal death
Drawing contrast for the other biochemical parameters within cases and controls, it was noted that there was a significant difference in serum bilirubin, SGOT, SGPT, blood urea and serum creatinine between the two groups (p-value<0.0005) [Table/Fig-7].
Correlation of blood pressure and other parameters.
| Biochemical tests | HypertensiveGroup | NormotensiveGroup | p-value |
|---|
| Serum Bilirubin | 0.56±0.32 | 0.37±0.14 | <0.0005 |
| Mild pre-eclampsia | 0.53/0.33 | | |
| Severe pre-eclampsia | 0.62/0.29 | | 0.02 |
| SGOT | 56.37±40.82 | 40.25±20.84 | <0.0005 |
| Mild pre-eclampsia | 56.57/40.27 | | |
| Severe pre-eclampsia | 55.79/42.96 | | 0.702 |
| SGPT | 54.65±35.5 | 44.91±23.12 | <0.0005 |
| Mild pre-eclampsia | 59.39/35.91 | | |
| Severe pre-eclampsia | 40.66/30.61 | | 0.002 |
| Blood urea | 30.83±18.71 | 21.09±7.77 | <0.0005 |
| Mild pre-eclampsia | 31.21/20.67 | | |
| Severe pre-eclampsia | 29.71/11.19 | | 0.804 |
| Serum Creatinine | 0.6±0.43 | 0.45±0.13 | <0.0005 |
| Mild pre-eclampsia | 0.6/0.49 | | |
| Severe pre-eclampsia | 0.59/0.19 | | 0.207 |
Discussion
Several studies have been done for correlating to serum LDH with feto-maternal outcome [7,10,11,13,14,17-26]; all these had different results because of varied sample size, study duration and parameter observed [Table/Fig-8].
Comparative evaluation of LDH in different studies.
| Author (year) | Type of Study | Sample Size | Observation | Conclusion |
|---|
| 1. Kant RH et al., [7] | Observational | 200 | LDH, LFT and KFT | Pre-eclampsia-Significant correlation with levels |
| 2. Dey PS et al., [10] | Case-control | 101 | LDH and GGT | Pre-eclampsia-significant correlation with levels |
| 3. Lavanya YR and Shobharani B [11] | Case-control | 60 | LDH | Pre-eclampsia-significant correlation with levels |
| 4. Bakhshandeh N et al., [13] | Case-control | 100 | LDH | Pre-eclampsia-Not significant |
| 5. Sreelatha S et al., [14] | Prospective | 80 | LDH and UA | Pre-eclampsia and LBW significant correlation with levels |
| 6. Hak J et al., [17] | Case-control | 200 | LDH | Pre-eclampsia and Foetal outcome- significant correlation with levels |
| 7. Bera S et al., [18] | Case-control | 124 | LDH, ALT and AST | BP and LBW- significant correlation with levels |
| 8. Gandhi M et al., [20] | Case-control | 50 | LDH and UA | Pre-eclampsia and SGA-significant correlation with levels |
| 9. Sabiullah M et al., [21] | Case-control | 50 | LDH | Pre-eclampsia-significant correlation with levels |
| 10. Sharma C et al., [22] | Case-control | 60 | LDH, AST andLipid profile | Raised in hypertensive group |
| 11. Umastyari Y et al., [23] | Prospective | 150 | LDH | Pre-eclampsia and SGA - significant correlation with levels |
| 12. Munde SM et al., [24] | Prospective | 80 | LDH | Pre-eclampsia foetal weight-significant correlation with levels |
| 13. Andrews L et al., [25] | Prospective | 2237/328 | LDH,ALT,AST UA, PT and APTT | Pre-eclampsia, Placental abruption, HELLP and DIC- significant correlation with levels |
| 14. Sonagra AD et al., [26] | Cross-sectional | 120 | LDH, ALP and UA | Pre-eclampsia- significant correlation with levels |
| 15. Present study | Case-control | 300 | LDH, LFT and KFT | Pre-eclampsia and Feto-maternal outcome- significant correlation with levels |
In consonance with previous researchers, serum LDH is correlated significantly with severity of blood pressure [6,8]. Detection of serum LDH in pregnant female would help the clinicians, even at Primary Health Centres (PHCs) to diagnose pre-eclampsia early and timely refer them to higher centres for better antepartum surveillance and manage in order to avert the complications associated with it. So it is proposed that efforts should be made to make this simple and cheap testing modality to be available at all PHCs for all antenatal hypertensive women.
Present study showed significantly elevated levels of LDH to be associated with presence of complications in hypertensive group as compared to normotensive group. This was analogous to conclusions from previous investigators [9,13]. This again emphasises the fact that morbidity due to HDP can be decreased only with stringent management of such women, after picking up the clinical entity well within time. For this purpose LDH is quite beneficial. Also higher number of LSCS in women with increased levels of serum LDH proved the fact that clinical suspicion and adequate facilities to diagnose pre-eclampsia in time must be endorsed even at the PHCs; so that such women can be timely transferred to first referral units for operative deliveries and for achieving optimum feto-maternal outcome. However, very few researchers did not find any significant difference in LDH level between normotensive and pre-eclamptic patients, which could be attributed to small sample size of their study [14].
Scrutinising the foetal outcome in the study in females with HDP, high levels of LDH were able to predict worst foetal prognosis in terms of prematurity, birth weight, NICU admission and foetal demise. This was similar to findings of past pollsters who reported that the mean gestational age decreased with increased LDH levels, which could be due to induction of labour at an earlier gestational age [6,12,13,15-19].
Higher number of preterm, LBW babies, intrauterine deaths, neonatal deaths and high NICU admissions, in hypertensive group could be due to early settings of placental insufficiency, followed by foetal growth restriction and hence recourse to early induction in those women after weighing the clinical scenario.
In order to establish predictive value of LDH as a marker for HDP, the present author’s correlated blood pressure with other available biochemical tests viz., serum bilirubin, SGOT, SGPT, blood urea and serum creatinine. Analogous to previous investigators, a positive correlation with the same in the present study highlighted the long-term significance of LDH in predicting development of HDP in antenatal women (at risk) [15,18,26]. Altered levels of LFT and KFT in severe pre-eclampsia provides us with a gamut of minimum laboratory parameters that must be performed in each women of HDP; adding to predictive value of LDH.
Ample knowledge of the above in all young gynaecologists and the grass-root multipurpose health workers and mid wives, along-with timely intervention would strengthen maternal surveillance and curtail the rate limiting step in pathogenesis of severe pre-eclampsia, averting its dreaded complications.
Limitation
Having drawn from a smaller populace over a period of 18 months, the results cannot be applied to the national population. For the latter, larger and more powered studies are advocated.
Conclusion
Elevated levels of LDH in HDP are indicative of cellular damage and dysfunction; thus LDH can be used as a biochemical marker, reflecting the severity of the disease. Detection of high-risk pregnancies with increased levels of LDH, besides careful monitoring in antenatal period and proper management would be the key to decrease both maternal and foetal morbidity and mortality. Thus all PHCs and sub-centers should be equipped with detection of LDH testing kits.
p-valuea=level of significance for severity of hypertension
p-valueb= level of significance for mean LDH values among cases and controls
p-valuea=level of significance among cases
p-valueb=level of significance among cases and controls