Characteristics of Sharp Injuries in Anaesthesia Providers in New York State: A Cross-sectional Study
Shamantha Reddy1, Vilma Joseph2, Zhen Liu3, Tracey Straker4
1 MD, Department of Anesthesiology, Montefiore Medical Center/Albert Einstein College of Medicine, New York City, New York, USA.
2 MD, Department of Anesthesiology, Montefiore Medical Center/Albert Einstein College of Medicine, New York City, New York, USA.
3 MD, PhD, Department of Emergency General surgery, The affiliated hospital of Qingdao University, Qingdao, Shandong, China.
4 MD, Department of Anesthesiology, Montefiore Medical Center/Albert Einstein College of Medicine, New York City, New York, USA.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Zhen Liu, No. 16, Jiangsu Rd, Qingdao, Shandong, China.
E-mail: drwatson@yeah.net
Introduction
Sharp instrument injury, defined as cuts, punches, scratches, nicks, or other injuries that break the skin and thus permit the entry of bacteria and viruses into the body, is the most common hazard faced by health care workers. Anaesthesiologists work in a rapid-paced environment, and are at high risk of injury from sterile sharps while preparing medication or dirty sharps that have been in contact with patients.
Aim
This field study aimed to determine the incidence and distribution of sharp injuries among anaesthesia providers in New York State.
Materials and Methods
The study was performed during year 2014 among the members of New York State Society of Anaesthesiologists (NYSSA). A total of 282 anaesthesia providers including anaesthesiology attendings, residents, fellow and interns participated in an anonymous online survey (Survey Monkey) of 18 questions.
Results
Of 2965 NYSSA members polled, 282 anaesthesia providers responded (9.51% response rate). A total of 248 (95.04%) respondents responded a prior needlestick injury. A total of 165 (59.14%) experienced dirty sharp injury (DSI) in the course of their practice, and the most common cause was hollow bore needles. The most common cause of DSI occurred while the provider was holding the sharp himself. A total of 117 (42.4%) respondents had injury even though safety mechanism was available and used.
Conclusion
Sharp injuries were a common risk to anaesthesia providers in New York State. Future research should investigate strategies to reduce injury and improve reporting among anaesthesia providers.
Clinical hazard, Needlestick injury, Occupational health
Introduction
Sharp instrument injury is the most common hazard faced by health care workers. “Sharps” have been defined as any object in the health care setting that can puncture the skin and thus permit the entry of bacteria and viruses into the body. A “sharps injury” includes cuts, punches, scratches, nicks, or other injuries that break the skin [1]. These injuries occur during activities such as preparing medications, blood sampling, needle disposal, waste collections, transfusions, intravenous catheter placement, skin incision, cutting, suturing and other invasive procedures. These injuries predispose to more than 20 types of infections including Human Immunodeficiency Virus (HIV), hepatitis B (HBV) and hepatitis C (HCV) [2]. The number of infections with HCV, HBV, and HIV in health care workers, attributable to exposure to percutaneous injuries reaches 39%, 37%, and 4.4% respectively [3]. Although needlestick injuries among health care workers such as nurses or medical students have been well studied, its incidence and characteristics in anaesthesiology providers remains underreported [4]. Anaesthesiology providers work in a rapid-paced environment, and are at high risk of injury from sterile sharps while preparing medication or dirty sharps that have been in contact with patients (needlestick injuries in anaesthetists). A sterile sharp injury has been defined as an injury from a sharp that has had no contact with a patient. A dirty sharp is defined as one that has been in contact with a patient, either directly such as in a vein or artery, or indirectly, such as in an intravenous line that is connected to a patient, or one used after a patient’s blood entered a multi-dose vial or piggyback drip. Even if the sharp was connected to an IV line at a distance from a patient, it was still considered a dirty sharp [5].
We conducted an electronic survey on the occurrence of sharp injuries in anaesthesia providers, as well as circumstances surrounding the injury, mechanism of injury and measures taken afterwards. We hope that our study will make the readers aware of the sharp injuries and shed some light on the importance of the safety mechanism use and the proper procedure and management after the sharp injury has occurred.
Materials and Methods
This study was performed during 2014 (September-December) in New York State. We sent an electronic survey to all the members of NYSSA. Responders were included in this study, others with no or incomplete responses were excluded. A total of 282 anaesthesia providers including anaesthesiology attendings, residents, fellow and interns participated in an anonymous online survey of 18 questions. After receiving an exemption from the Institutional Review Board of Albert Einstein College of Medicine, we sent an electronic survey to all the members of NYSSA in August 2014. A unique login was issued to each email address to prevent multiple responses. The survey was created by the Survey Monkey website (Survey Monkey, Inc. {US}) A validated questionnaire containing 18 questions targets sharp object injuries associated with anaesthesia-related activities.
Correlations with gender, academic and private practice, years of experience, emergent and non-emergent situations, as well as the type of the procedures involved with sharp injuries were addressed [Appendix 1]. The survey was created by the Survey Monkey website (Survey Monkey, Inc. [US]) and sent to the NYSSA members electronically. A repeat survey was sent to non-responders three weeks later.
Statistical Analysis
Data was collected and analysed using the statistical tools available on the Survey Monkey webpage. Data was expressed as means±SEM. A probability of p<0.05 was considered as statistically significant.
Results
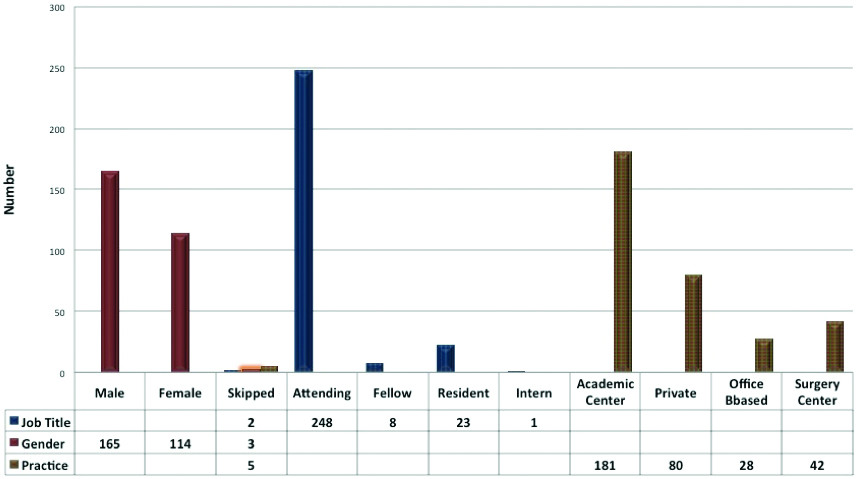
Of the 2965 NYSSA members polled, we received responses from 282 members-a 9.51% response rate [Table/Fig-1,2 and 3]. A total of 248 responses were anaesthesiology attendings, which constituted 87.94% of all responses. The remainder of the responses were from anaesthesiology residents 23 (8.16%), fellows 8 (2.84%), interns 1 (0.35%), 2 responders did not disclose their position. Of the responders, 114 (40.42%) were female, 165 (58.51%) were male, 3 responders did not disclose their gender. The majority of the survey respondents (53.87%) were in academic practice.
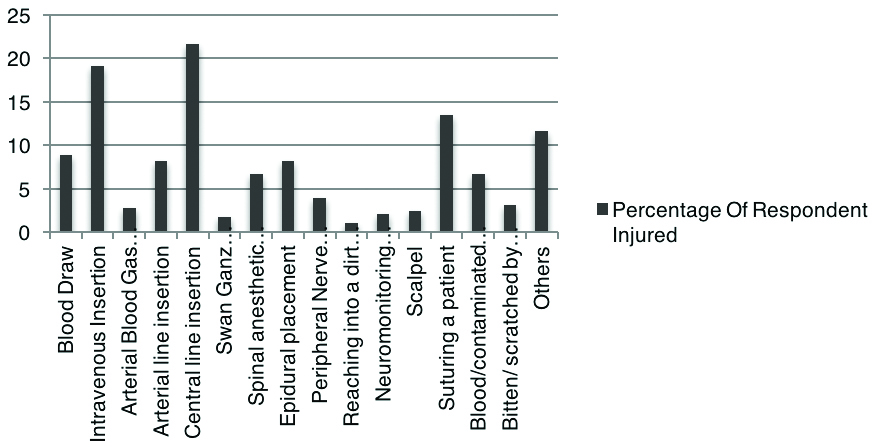
Common mechanisms of dirty sharp injury.
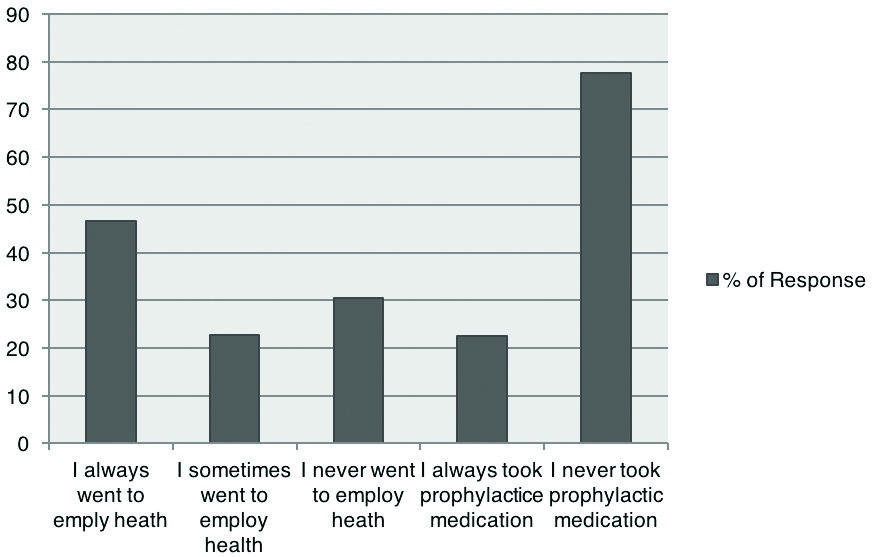
Prophylaxis and employee health visit after DSI.
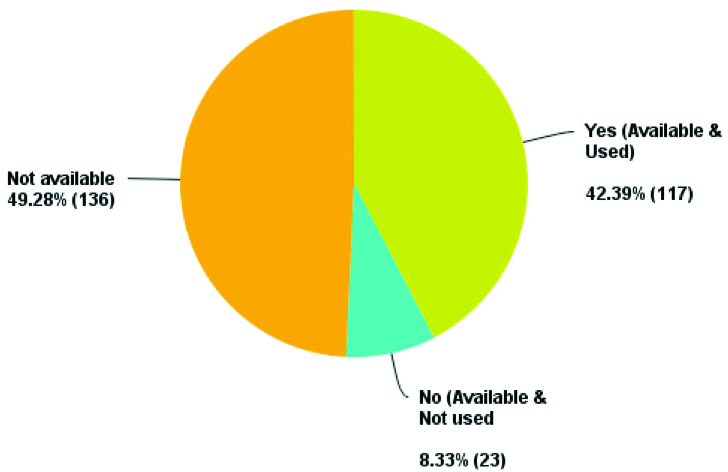
59.41% respondents experienced Dirty Sharp Injury (DSI) during their practice; see [Table/Fig-4]. One hundred seventeen (42.4%) respondents had injury even though safety mechanism was available and used [Table/Fig-5]. A 49.3% had injury with sharps where safety mechanisms were not available. Safety mechanisms were available but not used by 8.33% of the members at the time of the stick. A 95.04% anaesthesiology providers responded that they experienced sterile sharp injury in their practices [Table/Fig-6]. A 84.44% of respondents reported sterile injury with glass, while 95.51% anaesthesiology providers had sterile injury with needles [Table/Fig-7]. A total of 250 out of 282 responded for sterile glass injury and all responded for sterile needle injury [Table/Fig-8]. One hundred seven out of 207 respondents 52.7 (%) reported DSI due to hollow bore needles. Other frequent causes were angiocaths of different gauges 39.2 (%), suture needle 36.2 (%), solid needle 15.5 (%), scalpel 9.6 (%) and glass vial 9 (%) [Table/Fig-9].
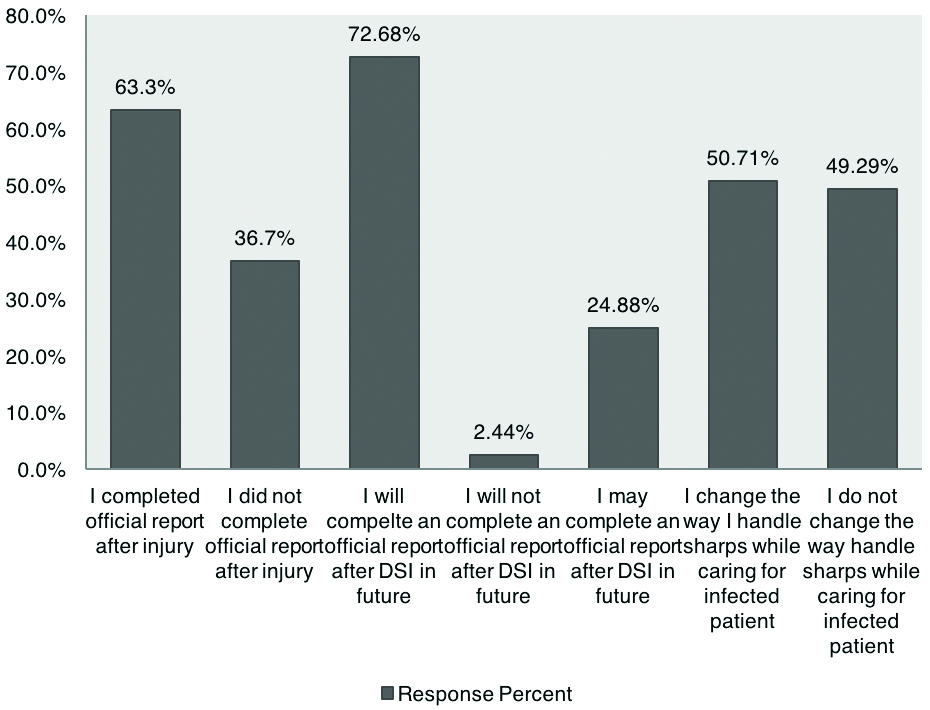
Report after experiencing sharp injury.
If there was a safety mechanism available for the sharp, did you use it.
Number of sharp injuries during anaesthesiology practice.
| Number of sharps injury | Response Percentage | Response Count |
|---|
| 1 | 13.83% | 39 |
| 2 | 17.73% | 50 |
| 3 | 16.96% | 45 |
| 4 | 8.87% | 25 |
| 5 | 9.22% | 26 |
| 6 | 5.67% | 16 |
| 7 | 2.84% | 8 |
| 8 | 1.06% | 3 |
| 9 | 1.06% | 3 |
| 10 and above | 15.96% | 45 |
| Not Applicable | 7.80% | 22 |
| Total | 100 | 282 |
Sterile sharp injuries among anaesthesia providers.
| Answer Options | Response Percentage | Response Count |
|---|
| Yes | 95.04% | 268 |
| No | 3.90% | 11 |
| Not applicable | 1.06% | 3 |
| Total | 100% | 282 |
Incidence of sterile injury and type of injury.
| Number | None | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 and more | Total |
|---|
| Type |
|---|
| Glass | 15.66% (39) | 26.91% (67) | 20.88% (52) | 8.84% (22) | 4.02% (10) | 8.84% (22) | 2.41% (6) | 1.20% (3) | 1.20% (3) | 0.00% (0) | 10.44% (26) | 250 |
| Needle | 4.49% (12) | 21.72% (58) | 24.72% (66) | 13.48% (36) | 5.24% (14) | 10.11% (27) | 4.12% (11) | 1.50% (4) | 1.50% (4) | 1.12% (3) | 12.73% (34) | 268 |
Incidences of dirty sharp injury.
| Number of injuries | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 and above | N/A | Total |
|---|
| Gauge needle | 22.04% 41 | 9.68% 18 | 2.69% 5 | 1.61% 3 | 0.54% 1 | 0.54% 1 | 0.54% 1 | 0.54% 1 | 0% 0 | 1.61% 3 | 60.22% 112 | 186 |
| Hollow bore needle | 28.99% 60 | 12.56% 26 | 4.35% 9 | 3.38% 7 | 0.00% 0 | 0.48% 1 | 0.97% 2 | 0.48% 1 | 0% 0 | 1.45% 3 | 47.34% 98 | 207 |
| Solid needle | 8.78% 13 | 4.05% 6 | 1.35% 2 | 0.68% 1 | 0.0% 0 | 0.0% 0 | 0.0% 0 | 0.0% 0 | 0% 0 | 0.68% 1 | 84.46% 125 | 148 |
| Suture needle | 20.90% 37 | 9.60% 17 | 1.69% 3 | 1.13% 2 | 1.69% 3 | 0.56% 1 | 0.0% 0 | 0.0% 0 | 0% 0 | 0.56% 1 | 63.84% 113 | 177 |
| Glass vial | 6.25% 9 | 1.39% 2 | 0.0% 0 | 0.0% 0 | 0.69% 1 | 0.0% 0 | 0.0% 0 | 0.0% 0 | 0% 0 | 0.69% 1 | 90.97% 131 | 144 |
| Scalpel | 7.53% 11 | 0.68% 1 | 0.0% 0 | 1.37% 2 | 0.0% 0 | 0.0% 0 | 0.0% 0 | 0.0% 0 | 0% 0 | 0.0% 0 | 90.41% 132 | 146 |
A 59.2% injuries occurred while the provider was holding the sharp himself. Injury occurred while someone else was holding the sharp in 26.25% members and while sharp lying on a surface in 31.66% members. When asked if the situation when injury occurred was emergent or not, majority (64.6%) of respondents said they received sharp injuries during a non-critical situation. Majority of the members answered that they had DSI while doing central venous catheterisation (21.63%), intravenous insertion (19.15%) and placement of sutures (13.47%) [Table/Fig-10].
Circumstances of dirty injury.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 and more | N/A | Total |
|---|
| Holding dirty sharp yourself | 26.61% 58 | 16.97% 37 | 5.50% 12 | 5.05% 11 | 1.38% 3 | 0.92% 2 | 0.46% 1 | 0.46% 1 | 0.46% 1 | 1.38% 3 | 40.83% 89 | 218 |
| Someone else holding dirty sharp | 18.13% 29 | 3.75% 6 | 1.88% 3 | 1.88% 3 | 0.00% 0 | 0.00% 0 | 0.00% 0 | 0.63% 1 | 0.00% 0 | 0.00% 0 | 73.75% 118 | 160 |
| Sharp lying on flat surface/tray | 20.00% 34 | 7.65% 13 | 1.76% 3 | 1.76% 3 | 0.59% 1 | 0.00% 0 | 0.00% 0 | 0.00% 0 | 0.00% 0 | 0.00% 0 | 68.24% 116 | 170 |
| Emergent situation | 20.63% 33 | 3.13% 5 | 3.13% 5 | 3.13% 5 | 0.00% 0 | 0.00% 0 | 0.00% 0 | 0.00% 0 | 0.00% 0 | 1.88% 3 | 68.13% 109 | 160 |
| Non-critical situation | 26.36% 63 | 20.50% 49 | 7.11% 17 | 4.18% 10 | 2.09% 5 | 0.84% 2 | 0.84% 2 | 0.00% 0 | 0.42% 1 | 1.26% 3 | 36.40% 87 | 23 |
As described in [Table/Fig-3], 46% of responders always went to employ health after needle stick injury, while 31% never did that. A 78% of respondents never took prophylactic medication after DSI. 63.30% respondents completed an incident report after sharp injury [Table/Fig-4]. A total of 72.68% respondents were willing to fill up an incident report after DSI. A total of 50.71% members will change their way of handling sharps when caring for patients known to have an infectious disease, such as hepatitis or AIDS. An 82.27% agreed that in case of a hospital worker getting a DSI, should a form that requests patient permission to perform HIV and/or hepatitis testing be added to paperwork at the time of admission [Table/Fig-6].
Discussion
Our survey study was started with an intention to look at the various ways a health care provider could accidentally get a sharp injury while handling the sharps. A 95.04% anaesthesiology providers responded a prior needlestick injury, which is much higher than the study conducted by Motavaf M et al., with an incidence of 56.8% [6]. One possible reason for this may due to demographics. According to a study conducted by Rosenberg AD et al., the incidence of sharp injury among anaesthesiologists was 88% in the 1990s, which is similar to our current study [7]. Compared to other healthcare workers, our study shows that anaesthesiology providers have a similar incidence of sharp injury. More than 90% of surgeons in training have experienced sharp injury [8]. Deipolyi AR et al., reported that 91% of interventional radiologist experienced sharp injury in the past [9]. However, Balouchi A et al., study shows that 64% of nurses experienced at least one sharp injury during the past year [10]. The reason for high incidence of sharp injury among anaesthesiology providers may due to the rapid-paced work environment.
The report rate after sharp injury is 63.3%, which is much higher than Motavaf M et al., (32.2%) and Tait AR’s et al., (31%) study [6,11]. However, additional measures to improve report rate such as increasing the awareness of outcomes or further education should be strengthened, since anaesthesiology providers are more prone to high-risk exposure in contrast with other healthcare staff [12].
Although safety mechanisms are important for preventing sharp injury [13], according to a study conducted by Wicker S et al., 59.3% of sharp injuries among anaesthesiology providers can be prevented by safety devices [14]. We suggest that educational programs for reducing sharp injuries should not be neglected and awareness of the risk of needle sticks might be helpful.
Our study reveals that the majority of respondents experienced sharp injuries during non-emergent situation. This phenomenon indicates that the providers should be careful during daily cases and not just in emergencies. But each provider most probably deals with less number of emergency cases compared to regular daily elective cases. So, the conclusion cannot be made that non-emergency situations have less incidence of sharp injuries.
Limitation
There are some limitations with our study such as small sample size, limited population. The information given was from the past experience and hence may decrease the accuracy due to recall bias.
This is a small study and is used as a needs assessment for a larger study. Ongoing studies of larger population need to be done to get more conclusive data.
Conclusion
Sharp injuries were a common risk to anaesthesia providers in New York State. Future research should try to increase the sample size, response rate, and investigate strategies to reduce injury and improve reporting among anaesthesia providers.
[1]. Thomas WJ, Murray JR, The incidence and reporting rates of needle-stick injury amongst UK surgeonsAnn R Coll Surg Engl 2009 91(1):12-17.10.1308/003588409X35921318990263 [Google Scholar] [CrossRef] [PubMed]
[2]. Elmiyeh B, Whitaker IS, James MJ, Chahal CA, Galea A, Alshafi K, Needle-stick injuries in the National Health Service: a culture of silenceJ R Soc Med 2004 97(7):326-27.10.1177/01410768040970070515229257 [Google Scholar] [CrossRef] [PubMed]
[3]. Pruss-Ustun A, Rapiti E, Hutin Y, Estimation of the global burden of disease attributable to contaminated sharps injuries among health-care workersAm J Ind Med 2005 48:482-90.10.1002/ajim.2023016299710 [Google Scholar] [CrossRef] [PubMed]
[4]. Cho E, Lee H, Choi M, Park SH, Yoo IY, Aiken LH, Factors associated with needlestick and sharp injuries among hospital nurses: a cross-sectional questionnaire surveyInt J Nurs Stud 2013 50:1025-32.10.1016/j.ijnurstu.2012.07.00922854116 [Google Scholar] [CrossRef] [PubMed]
[5]. Berry AJ, Greene ES, The risk of needlestick injuries and needlestick-transmitted diseases in the practice of anaesthesiologyAnaesthesiology 1992 77(5):1007-21.10.1097/00000542-199211000-000251306064 [Google Scholar] [CrossRef] [PubMed]
[6]. Motavaf M, Mohaghegh Dolatabadi MR, Ghodraty MR, Siamdoust SA, Safari S, Mohseni M, Anaesthesia personnel’s knowledge of, attitudes toward, and practice to prevent needlestick injuriesWorkplace Health Saf 2014 62(6):250-55.10.3928/21650799-20140514-0524971820 [Google Scholar] [CrossRef] [PubMed]
[7]. Rosenberg AD, Bernstein DB, Bernstein RL, Skovron ML, Ramanathan S, Turndorf H, Accidental needlesticks: do anaesthesiologists practice proper infection control precautions?Am J Anaesthesiol 1995 22(3):125-32. [Google Scholar]
[8]. Makary MA, Al-Attar A, Holzmueller CG, Sexton JB, Syin D, Gilson MM, Needlestick injuries among surgeons in trainingN Engl J Med 2007 356(26):2693-99.10.1056/NEJMoa07037817596603 [Google Scholar] [CrossRef] [PubMed]
[9]. Deipolyi AR, Prabhakar AM, Naidu S, Oklu R, Needlestick Injuries in Interventional Radiology Are Common and UnderreportedRadiology 2017 2017:17010310.1148/radiol.201717010328631962 [Google Scholar] [CrossRef] [PubMed]
[10]. Balouchi A, Shahdadi H, Ahmadidarrehsima S, Rafiemanesh H, The frequency, causes and prevention of needlestick injuries in nurses of kerman: a cross-sectional studyJ Clin Diagn Res 2015 9(12):DC13-15.10.7860/JCDR/2015/16729.696526816889 [Google Scholar] [CrossRef] [PubMed]
[11]. Tait AR, Tuttle DB, Prevention of occupational transmission of human immunodeficiency virus and hepatitis B virus among anaesthesiologists: a survey of anaesthesiology practiceAnaesth Analg 1994 79(4):623-28.10.1213/00000539-199410000-000027646614 [Google Scholar] [CrossRef] [PubMed]
[12]. Askarian M, Yadollahi M, Kuochak F, Danaei M, Vakili V, Momeni M, Precautions for health care workers to avoid hepatitis B and C virus infectionInt J Occup Environ Med 2011 2(4):191-98. [Google Scholar]
[13]. Dulon M, Lisiak B, Wendeler D, Nienhaus A, Workers’ Compensation Claims for Needlestick Injuries Among Healthcare Personnel in Hospitals, Doctors’ Surgeries and Nursing InstitutionsGesundheitswesen 2018 80(2):176-82.10.1055/s-0043-11400328753705 [Google Scholar] [CrossRef] [PubMed]
[14]. Wicker S, Jung J, Allwinn R, Gottschalk R, Rabenau HF, Prevalence and prevention of needlestick injuries among health care workers in a German university hospitalInt Arch Occup Environ Health 2008 81(3):347-54.10.1007/s00420-007-0219-717619897 [Google Scholar] [CrossRef] [PubMed]