Feeding Behaviour
This behaviour is related to obtaining and consuming food. It is a complex behaviour in the present day to day life that is regulated by many mechanisms like external factors such as food availability and quality, as well as by internal factors including sex, age, circadian rhythms and most importantly, the hormonal status related to energy homeostasis [1]. The understanding of the physiological basis of feeding behaviour regulation is particularly important, as in affluent societies, obesity has become a widespread problem [2]. However, the exact regulatory mechanisms are not well understood. Since hypothalamus is the centre for controlling feeding behaviour, a study has proved the role of hypothalamus in feeding behaviour and is mainly under the control of leptin and insulin [3-5]. Several hypothalamic neuropeptides such as Agouti-Related Protein (AgRP) and Neuropeptide Y (NPY) have been shown to be potent feeding stimulants, whereas Pre Opio-Melanocortins (POMC) and Cocaine- and Amphetamine-Regulated Transcript (CART) have been shown to suppress as done for the other food intake [6].
Physiology of Feeding
Feeding and satiety: Body weight depends on the balance between caloric intake and utilization of calories. Food intake is regulated not only on a meal to meal basis but also in a way that generally maintains weight at a given setpoint. If animals are made obese by force-feeding and then permitted to eat as they wish, their spontaneous food intake decreases until their weight falls to the control. If animals are starved and then permitted to eat freely, their spontaneous food intake increases until they regain the lost weight. It is common knowledge that the same thing happens in humans. Dieters can lose weight when caloric intake is reduced but when they discontinue their diets, 95% of them regain the weight they lost. Rebound weight gain is also noticed post recovery from illness that leads to weight loss.
Role of Hypothalamus
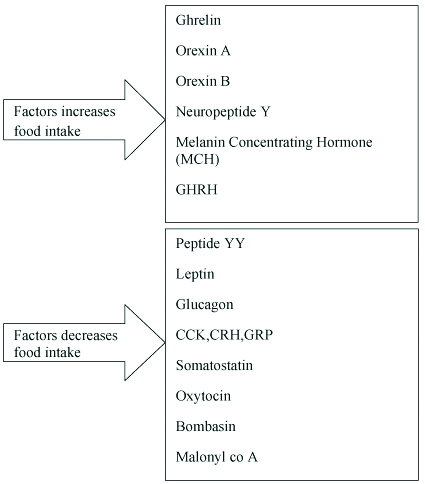
Hypothalamic regulation of the appetite for food depends primarily upon the interaction of two areas: a lateral feeding centre in the bed nucleus of the medial forebrain bundle at its junction with the pallido-hypothalamic fibres, and a medial satiety centre in the ventromedial nucleus. Stimulation of the ventromedial nucleus leads to inhibition of food intake, likewise, excessive eating termed as hyperphagia in the presence of increased food supply follows lesion in ventromedial nucleus resulting in hypothalamic obesity [Table/Fig-1] [7,8].
Showing the factors which increases and decreases food intake [7].
Theories of Feeding
There are four theories of feeding which includes: 1) Lipostatic theory; 2) Thermostatic theory; 3) Glucostatic theory; 4) Gut peptide theory.
Lipostatic Theory
Leptin is a hormone produced from fat cells, circulating protein containing 167 amino acids. Its name is derived from Greek word for thin. It acts on hypothalamus to decrease food intake and increase energy consumption. It appears to decrease the activity of neuropeptide Y neurons that increase appetite and to increase the activity of POMC secreting neurons. To reach its central site of action, circulating leptin must cross blood brain barrier. A short form of the leptin receptor is abundant in brain microvessels and probably is involved in transport of leptin into the brain. Leptin receptors are found in various tissues as well as in brain. In rodents, the decrease in plasma leptin produced by fasting is associated with inhibition of onset of puberty, depressed thyroid function and increased glucocorticoid secretion. It has been suggested that these are adaptive responses to the shortage of calories signalled by the decrease in leptin. Leptin receptors present in brown adipose tissue increases the activity of uncoupling proteins, thus producing a direct peripheral increase in energy expenditure [Table/Fig-2] [7,9].
Release of leptin from hypothalamus [7].

Gut Peptide Theory
Ghrelin is a hormone with 28 amino acid secreted from stomach. It operates like leptin as a peripherally generated regulator of appetite, but in the opposite fashion. It not only secretes growth hormone but also effects food intake and is increased during fasting. Central, peripheral and intraperitoneal administration of ghrelin increases food intake by stimulating arcuate nucleus, will be low in obese. Number of GI hormones have been reported to decrease food intake like peptide YY, PYY (secreted from small intestine and colon, levels are low in obese. It is due to idea that food entering the GIT triggers the release from the mucosa of substances which act on the brain to produce satiety. Ghrelin has to be acylated before it is released. An enzyme necessary for acylation of ghrelin is the Ghrelin O-acyltransferase, also expressed in the circulation of rodents [10].
Glucostatic Theory
The activity of the satiety centre in the ventromedial nuclei is probably governed in part by glucose utilisation of the neurons in it. Food intake is rapidly increased by intraventricular administration of compounds such as 2-deoxyglucose that decrease glucose utilisation in cells. Polyphagia is seen in diabetes mellitus, in which blood glucose is high but cellular utilisation is low because of the insulin deficiency [11].
Thermostatic Theory
Food intake is increased in cold weather and decreased in warm weather. However, there is little evidence that body temperature is a major regulator of food intake [7,12].
Schematic of the control of feeding in the hypothalamus: There are many factors that affect feeding behaviours such as Social facilitation, endocrine disorders, seasonal changes and stress. Among them, stress is the most common factor which affects the feeding behaviour in the life [Table/Fig-3] [13].
Control of feeding behaviour by hypothalamus [11].

Stress
Living beings are exposed to stress of varying degrees throughout their life. Stress is the disturbance of the normal body’s homeostasis or a condition of disharmony in response to a real or perceived threat or challenge. The threatening or challenge causing situation is referred to as a “stressor” [14]. It can also be described as a state characterised by a broad range of physiological and behavioural changes resulting from one or more stressors and biologically it is defined as “the non-specific response of the body to any demand” [3]. Today’s world man is exposed to large number of stress from a variety of sources.
Impact of Stress on Health
It is a significant individual and public health problem that is associated with numerous physical and mental health concerns. It is estimated that between 75% and 90% of primary care physician visits are caused by stress-related illnesses [15]. Cardiovascular disease, obesity, diabetes, depression, anxiety, immune system suppression, headaches, back and neck pain, and sleep problems are some of the health problems associated with stress. These conditions are most burdensome health problems in the United States based on health care costs, the number of people affected, and the impact on individual lives. Extreme levels of stress were reported by 22% of respondents from the 2011 Stress in America™ survey, and 39% reported that their level of stress had increased during the past year. More than 80% of the survey respondents at the world at work conference in 2012 reported that stress moderately or significantly contributed to their health care costs [14,16-18]. Stress can increase the risk for chronic diseases and other health problems, dealing with chronic conditions and poor health can increase the amount of stress one experiences. Stress also influences behaviours that affect health. Diet choices, sleep habits, and drug use are behaviours that are often negatively affected by stress. The APA’s 2011 survey showed that 39% of respondents reported overeating or eating unhealthy food because of stress, and 29% reported skipping a meal. In addition, 44% reported lying awake at night because of stress. On a positive note, 47% of respondents reported walking or exercise as a way of managing stress [19].
Types of Stress
It is very important to note that all stresses or stressors are not bad. Every individual experience a certain amount of stress on an almost daily basis, it cannot be eliminated completely. When it is experienced too much then it becomes a problem. Stress is of two kinds – Eustress-a positive form of good stress that motivates an individual to continue working and Distress – manifests when stress is no longer tolerable and/or manageable [20]. Stress may be eustress or distress can be determined by individual’s perception and coping resources for the stressor [21].
Based on Duration of Exposure
It can be chronic or acute. Chronic stress is a persistent, long lasting stressor, such as living with a terrible roommate, money, work, economy, death of loved ones, divorce, family and personal health problems. It is not easily resolved associated with negative health concerns. It results when there are constant multiple stressors or major life stressors present [22]. Acute stress, on the other hand, is a short lasting and one time stressor, such as failing an exam. Health is affected both physically and psychologically by exposure to repeated episodes of stress either due to excessive workload or constant worries. Stress coping skills will have to be learnt by such individuals exposed to episodic stress to avoid negative effects on health due to stress [13]. In addition, stress can be major or minor. A major stressor would be something like a death in the family, while a minor stressor may be as simple as getting stuck in traffic [23].
Stress affects the brain both physiologically and chemically. Depression and anxiety disorders are extremely common during stress. It is clear that these disorders are quite common in the general population, yet there is much to be learned about the causes of these disorders. Symptoms of depression include depressed mood, anhedonia, altered appetite, and nervousness, fatigue, lack of concentration, frequent colds, sleep disturbance and irritability. These psychopathologies develop by a complex interaction between genetic predisposition and an adverse environment [23].
Homeostasis that is challenged due to stressor in an organism may be regained by producing appropriate physiological responses to stress. Stress has long been considered as a critical risk factor in the development of addictive disorders and relapse to addictive behaviours [24,25]. The response to a stressor depends on how the individual assesses their environment and the stressor they experience. When the stressor exceeds a person’s ability to withstand or ability to respond appropriately to the stress, the homeostasis is disturbed [18]. One such homeostasis that is disrupted is in feeding behaviour [Table/Fig-4] [23].
Factors causing stress and its response from brain [23].

Stress does not affect each individual the same way. A stimulus that may be stressful to one individual may not be stressful to another. Environment, life events, and genetics play a role in an individual’s tolerance for stress. When an individual perceives a stimulus as stressful, a physiological and behavioural response will be displayed to regain equilibrium lost by the stressor [23].
Stress response due to endocrine and autonomic nervous system actions by epinephrine release prepares the body to overcome threat or challenge that is perceived as stress [26]. These physiological changes including increase in heart rate, respiratory rate, blood pressure, sweating and heightened acuity of senses associated with endorphin release characterise the fight or flight response which is manifestations of stress coping measures. There may be surplus energy production due to enhanced cortisol production which might suppress immune function [10]. A stressful situation induces the organism to mobilise not only the adrenal system and endocrine system but also the central nervous system and the pituitary [27]. One of the main mechanism by which stress affects the brain is by oxidative stress causing oxidative damage. During stressful conditions, oxidative stress reflects a mismatch between reactive oxygen species’ effect on the biological systems in the body and the detoxifying ability of these systems to repair the damage due to reactive intermediates. Disturbances in the normal state of cells can cause toxic effects through the production of peroxides and free radicals that damage all components of the cell. It can cause disruptions in normal mechanisms of cellular signalling and is associated with increased production of oxidising species or significant decrease in the effectiveness of antioxidants such as glutathione [28].
Effect of Acute and Chronic Stress on Hypothalamic Pituitary Adrenal Axis
It is well known that the Hypothalamic-Pituitary-Adrenal (HPA) axis helps in maintaining basal and stress related homeostasis of the nervous system as well as cardiovascular, immune and metabolic functions. The main regulation of circadian and stress-related activity of the HPA axis occurs at the level of parvicellular subdivision of the hypothalamic Paraventricular Nuclei (PVN). The majority of these neurons secrete CRH and Vasopressin (VP), which synergistically stimulate ACTH secretion by the pituitary corticotrophic cells. ACTH in turn leads to formation of Corticosterone (CORT) from Cholesterol (CHOL) which when released by the adrenal cortex can serve as inhibitory feedback control in the HPA system [Table/Fig-5] [29].
Showing the Release of glucocorticoids from hypothalamus [23].

It has been postulated that stress of any kind, acute and mild, or chronic and severe affects eating habits [30].
During acute stress Corticotropin-Releasing Hormone (CRH) is released from the medial parvocellular (mp) paraventricular nucleus of the hypothalamus (PVN), ACTH is released from pituitary and the cascade of reactions takes place for the release of glucocorticoids. CRH is also released from arcuate nucleus to inhibit neuropeptide Y and Agouti-Related Peptide (AGRP) (these are the hormones that increases food intake and suppresses energy expenditure). Urocortins are the molecules, belongs to CRH family, also released at this time which is also responsible for suppressing appetite by inhibiting the ghrelin activity. Thus, during acute stress, CRH is responsible for inhibiting the appetite [30,31]. Thus, CRH injected directly into the dorsal anterior Bed Nucleus of the Stria Terminalis (BNST) the ventral part or other brain regions such as the central amygdala or locus coeruleus) significantly reduces food intake in already food-deprived rats [32].
During chronic stress, glucocorticoids released from HPA in the bloodstream are elevated. Peripherally, glucocorticoids enhance the activity of lipoprotein lipase in adipose tissue, leading to an increase in fat storage [33]. Thus, in humans, a peripheral injection of CRH leads to increased food intake one hour later but the amount of food consumed is directly correlated with the magnitude of the cortisol response to the injection [34]. Glucocorticoids stimulate food intake by interacting with several appetite-regulating targets. They increase AMP-activated protein kinase signalling in the ARC to up-regulate NPY and AGRP expression in this region and stimulate the actions of these orexigenic peptides (increases food intake) [30]. It has been observed that rats prefer foods rich in fat and sucrose among other food items when exposed to stress indicating the need for more rewarding foods and preference for comfort foods due to stress induced glucocorticoid release [35].
Types of Stressors in Laboratory Animals
Physiological includes restraint stress, forced swimming stress, noise stress, electric foot shock stress, food deprivation. Restraint stress or immobilization is commonly used because it is less severe, but is still capable of activating the stress response by stimulating the hypothalamic pituitary adrenal axis. In this type of stressor, movement is limited by placement of rodent in a plexiglass chamber or immobilization bag. After every use of restraint, instruments should be washed to prevent any transmission disorders [36]. High intensity noise exposure (50-90 db) is also used as a physical stressor. This protocol can be used as a type of environmental stressor to mimic stress in everyday life. This stress is given for a period of 30 minutes continuously and animal is allowed to take rest for 10 minutes, remaining 30 minutes procedure is continued. It can able to stimulate the hypothalamo-pituitary adrenal axis and generate brain activity by causing anxiogenic effect on behaviour. If examiner is also staying in same room it’s better to use ear protectors [37].
Forced swimming stress: Animal made to swim in the water forcibly for five minutes then grasp the animal gently by the tail or trunk lift from the water, place it to dry. Container used for this should be 45 cm in length and 30 cm in breadth water has to be filled up to 30 cm. In each container two or three rats are permissible. After stress procedure animal is grabbed by tail and placed in a dry cloth. Like this procedure can be done by repeated intervals for 1 hour/day making sure that animal should not drown [38,39].
Electric foot shock stress: It is more severe stressor and can be applied using a metallic grid to shock the foot or to the tail. In this the suggested shock duration to be very short and the shock levels should be very low. For this type of stressor, animal should be trained in learning tasks for a period of some days but this is known to cause degeneration of structure. After completion of procedure for each rat that metallic grid floor should clean with ethanol or spirit to remove the odour, faeces and urine [39].
Food deprivation stress: It is the restriction of ad libitum amount of food for a certain period of time, giving feed at a fixed time for a period of four hours [40].
Psychological stress includes Maternal separation, Overcrowding, Social isolation, Sleep deprivation, Resident/intruder.
Maternal separation stress: It is an excellent prenatal stressor leads to activation of hypathalam-pituitary adrenal axis due to separation and handling. This stressor involves removal of pup from the care of its mother for certain period of time [38].
Overcrowding stress: permissible limit of animals in a cage is 2-3 but in this study, it involved the animals more than 4-5 [23].
Social isolation: It is a common type of psychological stressor in which subject is placed in a long term solitary housing at least about two to four weeks without any companion. Placing each animal in one cage and permitting the animals to listen and smell of other rats in the same colony [23,38].
Sleep deprivation: This type of stress is controversial because it is quite severe, in this animal is not allowed to sleep certain period of time by keeping the animal in a revolving drum, sleep deprivation drum or inverted flower pot technique [41].
Resident/intruder stress: It is social conflict stress involving threat from an aggressive male [23].
Some of the Review of Works on Stress Related to Feeding Behaviour Stress is known to alter feeding responses in a bidirectional pattern, with both increased and decreased intake of food [42]. It is an important factor in the development of addiction and in addiction relapse and may contribute to an increased risk for obesity and other metabolic diseases [43]. Uncontrollable, stress changes eating patterns and the salience and consumption of hyper palatable foods that induce metabolic changes that would promote weight and body fat mass [4]. Famitafreshi H et al., have demonstrated that food consumption was increased in addicted isolated rats when compared to addicted socialised rats and concluded that feeding behaviour was regulated by adult hippocampal neurogenesis in addiction period and socialisation improves it [44]. Stress also causes elevated glucocorticoid levels leading to stimulation of feeding behaviour and excessive weight gain [45]. Carr JA et al., demonstrated that stress inhibits feeding behaviour in all vertebrates [46]. Restraint stresses have shown to reduce body weight due to decreased intake of food [47]. Cristina R et al., demonstrated that acute stress causes weight loss and chronic stressors promote the activation of the pro-obesogenic mechanisms that favour the accumulation of central/visceral fat [48]. However, Favreau-Peigne et al., demonstrated that chronic stress altered animal welfare but also decreased body weight [49].
Although acute stress has shown to have facilitating effects on memory, chronic stress causes development of psychiatric disorders (depression and anxiety) which lead to altered appetite [32]. Stress was associated with significant elevation in the markers of oxidative stress in the cerebral cortex. Hacioglu G et al., demonstrated that exposure to stress causes increased production of ROS. Brain Derived Neurotrophic Factor (BDNF) has a crucial role in the survival and supports the neuronal cells, neuronal integrity and connectivity. It has role in neuronal process and its interaction with ROS might be crucial for neurodegenerative and neuropsychiatric abnormalities and the decreased expression of BDNF is implicated in the sensitivity to stress and stress enhanced responses. Also, BDNF deficient mice were observed to be more susceptible to stress induced oxidative damage, which suggests that there is direct interplay between oxidative stress indicators and BDNF levels in the brain [32].
Medina HV et al., stated that stress causes neuronal damage leads to significantly higher concentration of lipid peroxides by products like MDA and neuronal damage marker NSE [50]. It was proved that during oxidative stress the concentration of Glutathione (GSH), activity of Superoxide Dismutase (SOD) and Glutathione Peroxidase (GPX) was decreased while Malondialdehyde (MDA) were seen to be increased in different brain regions of experimental rats (hippocampus, cerebellum respectively) in comparison to the control group. It was obvious that MDA, the indicated marker for Lipid Peroxidation (LPO), showed a significant elevation in the exposed group compared to control [51]. Under normal condition, the over ROS production was neutralised by the antioxidant defence mechanisms. Glutathione (GSH) is an important non-enzymatic antioxidant that plays a crucial role in the detoxification of ROS. SOD and GPX enzymes are the first line of cellular defence against oxidative injury [52].
Conclusion
Stress is known to cause many factors leading to various disorders. It is known to cause oxidative stress by causing oxidative damage. Uncontrollable stress causes changes in feeding behaviour and is known to alter feeding responses in a bidirectional pattern, with both increased and decreased intake of food.
[1]. Schwartz MW, Woods SC, Porte D, Seeley RJ, Baskin DG, Central nervous system control of food intakeNature 2000 404:661-71.10.1038/3500753410766253 [Google Scholar] [CrossRef] [PubMed]
[2]. Berthoud HR, Neural control of appetite: cross-talk between homeostatic and non-homeostatic systemsAppetite 2004 43:315-17.10.1016/j.appet.2004.04.00915527935 [Google Scholar] [CrossRef] [PubMed]
[3]. Dhir A, Padi SS, Naidu PS, Kulkarni SK, Protective effect of naproxen (non-selective COX-inhibitor) or rofecoxip (selective COX-2 inhibitor) on immobilization stress induced behavioural and biochemical alterations in miceEur J Pharmacol 2006 535(1-3):192-98.10.1016/j.ejphar.2006.01.06416522321 [Google Scholar] [CrossRef] [PubMed]
[4]. Yvonne H, Yau C, Potenza MN, Stress and eating behavioursMinerva Endocrinol 2013 38(3):255-67. [Google Scholar]
[5]. Hillebrand JJ, de Wied D, Adan RA, Neuropeptides, food intake and body weight regulation: a hypothalamic focusPeptides 2002 23:2283-306.10.1016/S0196-9781(02)00269-3 [Google Scholar] [CrossRef]
[6]. Stanley S, Wynne K, McGowan B, Bloom S, Hormonal regulation of food intakePhysiol Rev 2005 85:1131-58.10.1152/physrev.00015.200416183909 [Google Scholar] [CrossRef] [PubMed]
[7]. Ganong. Review of medical physiology. 21st edition.128-30 [Google Scholar]
[8]. Atalayer D, Rowland NE, Structure of motivation using food demand in micePhysiol Behav 2011 104(1):15-19.10.1016/j.physbeh.2011.04.04221549728 [Google Scholar] [CrossRef] [PubMed]
[9]. Mayer J, Regulation of energy intake and the body weight: the glucostatic theory and the lipostatic hypothesisAnnals of the New York Academy of sciences 1955 63(1):15-43.10.1111/j.1749-6632.1955.tb36543.x13249313 [Google Scholar] [CrossRef] [PubMed]
[10]. Prinz P, Stengel A, Control of food intake by gastrointestinal peptides: mechanisms of action and possible modulation in the treatment of obesityJ NeurogastroenterolMotil 2017 23(2):180-96.10.5056/jnm1619428096522 [Google Scholar] [CrossRef] [PubMed]
[11]. Fukushima A, Hagiwara H, Fujioka H, Kimura F, Akema T, Funabashi T, Sex differences in feeding behaviour in rats: the relationship with neuronal activation in the hypothalamusFrontiers in Neuroscience 2015 9:8810.3389/fnins.2015.0008825870535 [Google Scholar] [CrossRef] [PubMed]
[12]. Yates AA, Food intake, appetite, and work in hot environments 1993 Chapter: 15. 298 [Google Scholar]
[13]. Gregus A, Wintink AJ, Davis AC, Kalynchuk LE, Effect of repeated corticosterone injections and restraint stress on anxiety and depression-like behaviour in male ratsBehav Brain Res 2005 156(1):105-14.10.1016/j.bbr.2004.05.01315474655 [Google Scholar] [CrossRef] [PubMed]
[14]. Chrousos GP, Gold PW, The concepts of stress and stress systems disordersJAMA 1992 267(9):1244-52.10.1001/jama.267.9.12441538563 [Google Scholar] [CrossRef] [PubMed]
[15]. American Institute of Stress Web site [Internet]. Yonkers (NY): The American Institute of Stress; [cited 2012 July 2]. Available from: http://www.stress.org [Google Scholar]
[16]. American Psychological Association. Stress in America: Our Health at Risk. Washington (D.C.): The American Psychological Association; 2011. Pp.78. Available from: www.stressinamerica.org [Google Scholar]
[17]. American Psychological Association Website [Internet]. Washington (D.C.): American Psychological Association; [cited 2012 June 27]. Available from: http://www.apa.org [Google Scholar]
[18]. CCH Business Law Daily Web site [Internet]. Riverwoods (IL): CCH Business Law Daily; [cited 2012 June 27]. Available from: http://www.employmentlawdaily.com [Google Scholar]
[19]. American Psychological Association. Stress in America: Our Health at Risk. Washington (D.C.): The American Psychological Association; 2011. 78 Pp. Available from: www.stressinamerica.org [Google Scholar]
[20]. Arria AM, O Grady KE, Caldeira KM, Vincent KB, Wilcox HC, Wish ED, Suicide ideation among college students: A multivariate analysisArch Suicide Res 2009 13:230-46.10.1080/1381111090304435119590997 [Google Scholar] [CrossRef] [PubMed]
[21]. Erica MJ, Stress relief: the role of exercise in stress managementACSM’s Health and Fitness Journal 2013 17(3):14-19.10.1249/FIT.0b013e31828cb1c9 [Google Scholar] [CrossRef]
[22]. American Psychological Association. Stress in America: Our Health at Risk. Washington (D.C.): The American Psychological Association; 2011. 78 Pp. Available from: www.stressinamerica.org [Google Scholar]
[23]. Atchley D, The time-course of the effects of stress on behaviour in rodentsEukaryon 2011 :17 [Google Scholar]
[24]. Kreek MJ, Nielsen DA, Butelman ER, LaForge KS, Genetic influences on impulsivity, risk taking, stress responsivity and vulnerability to drug abuse and addictionNat Neurosci 2005 8(11):1450-57.10.1038/nn158316251987 [Google Scholar] [CrossRef] [PubMed]
[25]. Koob GF, A Role for brain stress systems in addictionNeuron 2008 59(1):11-34.10.1016/j.neuron.2008.06.01218614026 [Google Scholar] [CrossRef] [PubMed]
[26]. Kayalvizhi , Vijaya L, Nilesh NK, Chandrasekhar M, A study on the role of antioxidant vitamin e supplementation on behavioural changes induced by immobilization stress in miceIndian J Sci 2012 2(1):27-30. [Google Scholar]
[27]. de Diego OY, Romero ZY, Decara J, Alphotochopherol protects against oxidative stress in the fragile knock out mouse; an experimental therapeutic approach for the Fmr1 deficiencyNeuropsychopharma 2009 34(4):1011-26.10.1038/npp.2008.15218843266 [Google Scholar] [CrossRef] [PubMed]
[28]. Djordjevic J, Cvijic G, Davidovic V, Different activation of ACTH and corticosterone release in response to various stressors in ratsPhysiol Res 2003 52:67-72. [Google Scholar]
[29]. Sominsky L, Spencer SJ, Eating behaviour and stress: a pathway to obesityFront Psychol 2014 5:43410.3389/fpsyg.2014.0043424860541 [Google Scholar] [CrossRef] [PubMed]
[30]. Currie P, Integration of hypothalamic feeding and metabolic signals: focus on neuropeptide YAppetite 2003 41:335-37.10.1016/j.appet.2003.08.01114637334 [Google Scholar] [CrossRef] [PubMed]
[31]. Richard D, Lin Q, T feeva E, The corticotropin-releasing factor family of peptides and CRF receptors: their roles in the regulation of energy balanceEur J Pharmacol 2002 440:189-97.10.1016/S0014-2999(02)01428-0 [Google Scholar] [CrossRef]
[32]. Ciccocioppo R, Fedeli A, Economidou D, Policani F, Weiss F, Massi M, The bed nucleus is a neuro anatomical substrate for the anorectic effect of corticotropin-releasing factor and forits reversal by nociceptin/orphaninJNeurosci 2003 23:9445-51.10.1523/JNEUROSCI.23-28-09445.2003 [Google Scholar] [CrossRef]
[33]. Jorntorp P, Do stress reactions cause abdominal obesity and comorbiditiesObesRev 2001 2:73-86.10.1046/j.1467-789x.2001.00027.x12119665 [Google Scholar] [CrossRef] [PubMed]
[34]. George SA, Khan S, Briggs H, Abelson JL, CRH-stimulated cortisol release and food intake in healthy, non-obese adultsPsychoneuroendocrinology 2010 35:607-12.10.1016/j.psyneuen.2009.09.01719828258 [Google Scholar] [CrossRef] [PubMed]
[35]. Shimizu H, Arima H, Watanabe M, Goto M, Banno R, Sato I, Glucocorticoids increase neuropeptideY and agouti-related peptide gene expression via adenosine mono phosphate activated protein kinase signaling in the arcuate nucleus of ratsEndocrinology 2008 149:4544-53.10.1210/en.2008-022918535107 [Google Scholar] [CrossRef] [PubMed]
[36]. Warne JP, Horneman HF, Wick EC, Bhargava A, Pecoraro NC, Ginsberg AB, Comparison of superior mesenteric versus jugular venous infusions of insulin in streptozotocin-diabetic rats on the choice of caloric intake, body weight, and fat storesEndocrinology 2006 147:5443-451.10.1210/en.2006-070216873535 [Google Scholar] [CrossRef] [PubMed]
[37]. Gulay H, Assessment of oxidative stress parameters of brain derived neurotrophic factor heterozygous mice in acute stress modelIran J Basic Med Sci 2016 19(4):388-93. [Google Scholar]
[38]. Heinrichs SC, Koob GF, Application of experimental stressors in laboratory rodentsCurrent Protocols in Neuroscience 2006 82:123-24. [Google Scholar]
[39]. Yahav RY, Franko M, Huly A, Doron R, The forced swim test as a model of depressive-like behaviourJ Vis Exp 2015 97:52587 [Google Scholar]
[40]. Dietze S, Katarina R, Fink H, Brosda J, Voigt JP, Food deprivation, body weight loss and anxiety-related behaviour in ratsAnimals (Basel) 2016 6(1):410.3390/ani601000426751481 [Google Scholar] [CrossRef] [PubMed]
[41]. Shinomiya K, Shigemoto Y, Okuma C, Mio M, Kamei C, Effects of short acting hypnotics on sleep latency in rats placed on grid suspended over waterEur J Pharmacol 2003 460:13910.1016/S0014-2999(02)02915-1 [Google Scholar] [CrossRef]
[42]. Jayanthi M, Margaret JM, The link between stress and feeding behaviourNeuropharmacology 2012 63(1):97-110.10.1016/j.neuropharm.2012.04.01722710442 [Google Scholar] [CrossRef] [PubMed]
[43]. Pagadala P, Manaschakravarthy K, Nerella S, Shankarappa V, Babu MR, Heart rate variability and electrocardiographic changes during acute mental stress in first MBBS students: An Analytical studyNatl J Physiol Pharm Pharmacol 2019 9(Online First)10.5455/njppp.2019.9.1135108122018 [Google Scholar] [CrossRef]
[44]. Hamidreza F, Morteza K, Fatemeh A, Assessment of improvement in feeding behaviour and co morbid psychiatric disorders in morphine addiction period in socialized male ratsINDJ 2016 8(1):01-16.10.9734/INDJ/2016/27633 [Google Scholar] [CrossRef]
[45]. Luba S, Spencer J, Eating behaviour and stress: a pathway to obesityStress Regulation of Appetite 2014 5:43410.3389/fpsyg.2014.0043424860541 [Google Scholar] [CrossRef] [PubMed]
[46]. Carr JA, Stress, neuropeptides, and feeding behaviour: a comparative perspectiveIntegr Comp Biol 2002 42(3):582-90.10.1093/icb/42.3.58221708754 [Google Scholar] [CrossRef] [PubMed]
[47]. Jooyeon J, Dong HL, Sang S, Effect of chronic restraint stress on body weight, food intake and hypothalamic gene expressions in miceEndocrinolMetab 2013 28:288-196.10.3803/EnM.2013.28.4.28824396694 [Google Scholar] [CrossRef] [PubMed]
[48]. Cristina R, Suzanne L, Impact of stress on metabolism and energy balanceCurrent Opinion in Behavioural Science 2016 9:71-77.10.1016/j.cobeha.2016.01.011 [Google Scholar] [CrossRef]
[49]. Favreau-Peigne A, Calandreau L, Constantin P, Gaultier B, Bertin A, Emotionality modulates the effect of chronic stress on feeding behaviour in birdsPLoS ONE 2014 9(2):8724910.1371/journal.pone.008724924498302 [Google Scholar] [CrossRef] [PubMed]
[50]. Medina HV, Ramos LJ, Luquin S, Sanchez LF, Garcia EJ, Navarro RA, Increased lipid peroxidation and neuronal specific enolase in treatment refractory schizophrenicsJ Psychiatr Res 2007 41(8):652-58.10.1016/j.jpsychires.2006.02.01016600300 [Google Scholar] [CrossRef] [PubMed]
[51]. Husseina S, Abdel-Aleem ES, Galalb MK, Biochemical and histological studies on adverse effects of mobile phone radiation on rat’s brainJournal of Chemical Neuroanatomy 2016 78:10-19.10.1016/j.jchemneu.2016.07.00927474378 [Google Scholar] [CrossRef] [PubMed]
[52]. Kurutas EB, The importance of antioxidants which play the role in cellular response against oxidative/nitrosative stress: current stateNutr J 2016 15:7110.1186/s12937-016-0186-527456681 [Google Scholar] [CrossRef] [PubMed]