Prognostic Factors on Survival of Rasoul-e-Akram Hospital Patients with Colorectal Cancer: A Survival Analysis
Shahram Agah1, Elham Vafaei2, Abolfazl Akbari3, Mansoureh Tavousi4, Mojtaba Soltani-Kermanshahi5
1 Colorectal Research Center, Rasoul-e-Akram Hospital, Iran University of Medical Sciences, Tehran, Iran.
2Rasoul-e-Akram Hospital, Iran University of Medical Sciences, Tehran, Iran.
3 Colorectal Research Center, Rasoul-e-Akram Hospital, Iran University of Medical Sciences, Tehran, Iran.
4 Colorectal Research Center, Rasoul-e-Akram Hospital, Iran University of Medical Sciences, Tehran, Iran.
5 Social Determinants of Health Research Center, School of Medicine, Semnan University of Medical Sciences, Semnan, Iran.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Mojtaba Soltani-Kermanshahi, Department of Epidemiology and Biostatistics, Semnan University of Medical Sciences, Semnan, Iran.
E-mail: msoltani@semums.ac.ir; msoltani@farabi.tums.ac.ir
Introduction
Colorectal Cancer (CRC) also called colon cancer or intestine cancer is characterised by cancerous growth of cells in the rectum, colon and appendix. CRC is the fourth most common form of cancer after skin, gastric, bladder and prostate cancers among Iranian population, since 6-8 people per 10,000 people suffer from this disease.
Aim
To evaluate the prognostic factors on survival of patients with CRC, in Rasool-e-Akram Hospital in Tehran, Iran.
Materials and Methods
The population under study included patients with CRC, admitted between 30 March 2010 to 29 March 2013, in Rasoul-e-Akram teaching hospital affiliated with Iran University of Medical Sciences, Tehran, Iran. The event was death from CRC and any other cause. Possible prognostic variables were selected from documents. A multivariate Cox regression model was performed to study the concurrent effect of parameters on survival after taking into account the parallel effect of residual factors.
Results
In this research 80 patients were studied. With respect to inclusion and exclusion criteria 68 patients were enrolled and data related to 68 patients were exposed to statistical analysis. Median and mean age of patients were equal to 55.5 and 55.0 years, respectively with standard deviation of 13.9 years. Only “Logarithm of White Blood Cell” showed a significant effect on survival of patients with CRC.
Conclusion
The results of our study showed the effect of WBC on survival of patients with CRC. Accordingly the increased one unit of log WBC increased the death hazard by 21.22 times in CRC patient.
Cox regression, Death, White blood cell
Introduction
Colorectal Cancer (CRC) also called colon cancer or intestine cancer is characterised by cancerous growth of cells in the rectum, colon and appendix [1]. CRC is considered as the third most prevalent malignancy and the fourth leading cause of cancer-related mortality worldwide [2]. In 2018, the total of new patient cases with cancer (incidents) were reported to be 18,078,957 cases; approximately 10.2% of the people diagnosed with cancer, had CRC and about 9.2% of cancer deaths were related to CRC [3].
The incidence rate of CRC varies greatly worldwide [4]. In 2012, the highest incidence rate of CRC was found in the Republic of Korea (AGR=45) and the lowest incidence rate of CRC was found in Singapore (AGR=33.7 per 100,000) [5,6]. CRC incidence has been steadily increasing in developing countries [7]. The highest increase was recorded in Western Asia (including Israel and Kuwait) and in Eastern Europe (including Czech Republic, Slovakia and Slovenia) [2].
CRC is the fourth most common form of cancer after skin, gastric, bladder and prostate cancers among Iranian population, since 6-8 people per 10,000 people suffer from this disease. Also, it is considered as the fifth most common form of cancer among men and the third most common among women in Iran. Furthermore, about one fifth of cases of CRC in Iran occurs in people aged below 40 years old [8,9].
Several research have been done for cancer related financial hardship such as, lost time from work and lost productivity followed by travel costs and medical costs not covered by the government health insurance [10,11]. According to the most recent Canadian researches on the burden of disease, out of $16.1 billion (b) related to the medical costs of cancer, the direct) and indirect burden of cancer were reported as $4.2b and $11.9b, respectively [12].
Distant metastasis is the major cause of death in patients with CRC [13]. The development of overwhelming majority of CRC cases was found to be associated with environmental factors rather than heritable genetic mutations [12]. CRC has been known to have different biologic characteristics, treatment modalities, recurrence patterns and survival rates from those cancers occurring in the colon [14-18].
The survival in patients with CRC is an important point and, it is influenced by many factors such as: WBC (White Blood Cell), coffee consumption, use of antibiotics, sex, child-Pugh class, Carcino embryonic Antigen (CEA), KRAS gene status and red meat consumption [1,19-23]. Since separate analysis of CRC may provide more specific information on the prognosis, there is a need for further studies to find the prognostic factors and survival of patients with CRC. Therefore, the present research was aimed to determine the prognostic factors on survival of patients with CRC in Rasoul-e-Akram hospital in Tehran, Iran.
Materials and Methods
Patients and Data Source
Rasoul-e-Akram hospital is a referral hospital located in the capital of Iran. The present study was a cross-sectional study which included patients with CRC admitted between 30 March 2010 to 29 March 2013 in Rasoul-e-Akram teaching hospital affiliated with Iran University of Medical Sciences, Tehran, Iran. Patients with rectum cancer were excluded from the study and only the patients with complete data were included in the study. The event was death from CRC and other causes were censored in the analysis. The survival time was calculated based on the sum of days starting from admission date until death from CRC or any other cause or end of the study (29 March 2013).
Sample Size
Considering the age as the principal variable and death rate of patients with CRC and also “coefficient of determination” or “R-squared value” of age on other variables, 70 patients were estimated as the sample size by the PASS software. About 10% of attrition rate was assumed and then the final sample size increased to 80 patients. In our calculation type I error and power were reported by 5% and 80%, respectively.
Prognostic Variable
Possible prognostic variables were selected from patient’s medical records including WBC (White Blood Cell), RBC (Red Blood Cell), Hb (Hemoglobin), BG (Blood Group), SC (Stage of Cancer), DM (Diabetes Mellitus), as well as age at first visit and gender.
Statistical Analysis
Descriptive statistics were done by measuring median, mean and standard deviation for quantitative variables and percentages/counts for discrete parameters. Cox-model is frequently used in the case of studying the effect of variables on censored time-to-event outcome [24]. A multivariate Cox proportional hazards model was performed to study the concurrent effect of parameters on survival after taking into account the parallel effect of residual factors. Selection of best model was done based on manual and self-acted backward methods. Results of the analysis were shown in the form of regression estimates tables. Hazard ratios of outcomes under study were calculated for each parameter estimate as well as reporting the 95% of confidence intervals. Categorical covariates were compared with a pre-specified reference category. All analysis were made at a significance level of α=0.05 using SPSS software version 18.
Results
In this study 80 patients were perused, off which 68 patients were enrolled with respect to inclusion and exclusion criteria and data related to 68 patients were used for statistical analysis.
Patients
Median and mean age of patients were 55.5 and 55.0 years, respectively with standard deviation of 13.9 years. The mean and standard deviation of WBC, RBC and Hb were equal to 7.9±3.2109/L, 4.0±0.51012/L and 11.1±1.5 mmol/L, respectively. Males constituted 58.8% of the patients and 67.6% of them aged more than 50 years [Table/Fig-1]. More than half of the patients had at least stage III of CRC.
Demographic, clinical and laboratory variables in the study population (n=68).
| Factor | n | % |
|---|
| Gender |
| Male | 40 | 58.8 |
| Female | 28 | 41.2 |
| Age | | |
| <50 years | 22 | 32.4 |
| ≥50 | 46 | 67.6 |
| Cancer Stage |
| 0 and I | 12 | 17.6 |
| II | 14 | 20.6 |
| III | 9 | 13.3 |
| IV | 33 | 48.5 |
| Diabetes | | |
| Yes | 19 | 27.9 |
| No | 49 | 72.1 |
| Death | 14 | 20.6 |
In this study, other factors such as RBC, HB, diabetes, age, log WBC and stage were not different and there was no statistically significant difference between males and females (p-value >0.1), of the 68 study patients, death occurred in 14 (20.6%) patients by CRC (p-value=0.46).
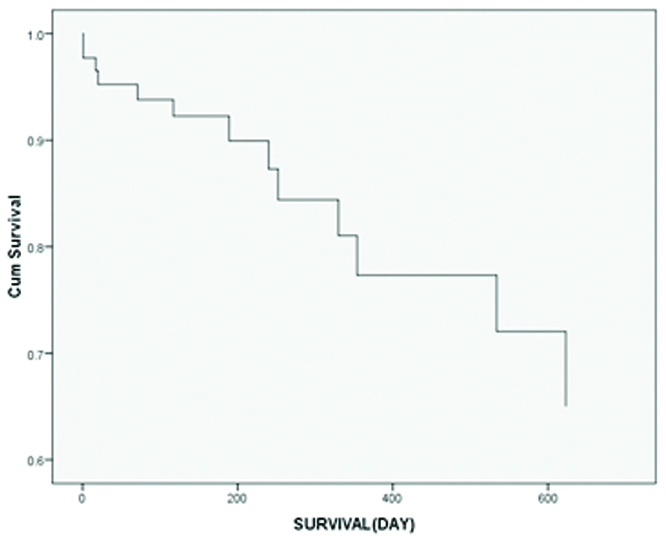
[Table/Fig-2] shows the initial model for the evaluation of patients with CRC. In the backward method, all factors were included in the model and then only the significant variables remained. Log WBC was only found to have a significant effect on survival of patients with CRC. [Table/Fig-3] presents the results of backward selection. Hazard of death increased with the increase in log WBC, about 21 times for every unit. [Table/Fig-4] shows the cumulative survival of patients with CRC at mean of log WBC (1.98).
Initial Cox proportional odds regression model for patients with CRC.
| Variable | β | SE | Hazard ratio | p-value |
|---|
| Log WBC | 5.95 | 2.27 | 383.47 | 0.009 |
| RBC | -4.11 | 1.88 | 0.02 | 0.029 |
| HG | 1.33 | 0.64 | 3.77 | 0.037 |
| Blood group (A) | 0.91 | 1.26 | 2.47 | 0.472 |
| Blood group (B) | -0.14 | 1.31 | 0.87 | 0.914 |
| Blood group (AB) | -1.20 | 2.27 | 0.30 | 0.596 |
| Blood group (O) | Reference |
| Stage 1 | 2.74 | 2.07 | 15.54 | 0.185 |
| Stage 2 | -3.76 | 2.06 | 0.02 | 0.067 |
| Stage 3 | -0.04 | 1.12 | 0.96 | 0.971 |
| Stage 4 | Reference |
| Diabetes | 4.27 | 1.55 | 71.26 | 0.006 |
| Sex | 1.88 | 0.95 | 6.54 | 0.048 |
Final Cox proportional odds regression model for patients with CRC.
| Variable | β | SE | p-value | Hazard ratio | 95% of CI for hazard ratio |
|---|
| Log WBC | 3.06 | 1.02 | 0.003 | 21.22 | 2.871 | 156.772 |
Log: Logarithm; CI: Confidence interval
Cumulative survival of patients with CRC at mean of LOG-WBC.
Discussion
In this study, WBC, RBC, HG, BG, SC, DM, as well as age at first visit and gender were considered as prognostic factors on survival of patients with CRC. More than 50% of patients had at least stage III cancer, indicating the insouciance to refer the doctor.
For decades, the pivotal role of WBCs in wound healing and tissue repair has been recognised. Depending on the environment, WBC function is adaptive. For example, WBCs can be inflammatory, such that it hinders tissue repair under certain conditions such as active infection [25-27].
Lee YJ et al., at a cohort study conducted in Korea showed the association between WBC and the mortality risk of all cancers but, they failed to show this association with the rough subgroup analyses of colon, prostate or breast cancers [18].
The results of the present study showed the significant effect of WBC on survival of patients with CRC. Accordingly, 1 unit increase in the log WBC caused 21.22 time increase in the death hazard in patients with CRC. The graph is also consistent with this result.
Alberts SR and Wagman LD ported the longer survival in patients with CRC who had liver metastasis when they used the new chemotherapy methods [13]. In 2014, a prospective cohort study was carried out to evaluate the effect of coffee consumption on CRC and the results showed the reduction of overall occurrence of colorectal tumors as a result of coffee consumption [1].
In a nested case-control study conducted Dik VK et al., showed the association between increasing use of antibiotics and increasing risk of CRC [22]. Previous studies showed that the global incidence of CRC is higher in men [8,23].
In a study conducted between 2007-2014, Lahti SJ et al., showed that child- Pugh class, CEA and KRAS gene status are the independent prognostic factors of overall survival in patients with unresectable CRC liver metastases [9].
Limitation
The missing information from patients such as CEA, or adjuvant chemotherapy was considered as a limitation of the present study, resulting in the lack of evaluation for other factors related to the survival of patients.
Conclusion
The results of the current study confirmed the effect of WBC on survival of patients with CRC. Accordingly, 1 unit increase in log of WBC caused the 21.22 time increase in death hazard in patients with CRC.
[1]. Samanian S, Mahjoubi B, Mahjoubi F, Mirzaee R, Azizi R, Investigation of the genes MDR1/MRP1 and their relationship with clinical and para-clinical characteristics of colorectal cancerZahedan Journal of Research in Medical Sciences 2013 15(7):31-34. [Google Scholar]
[2]. Gandomani HS, Aghajani M, Mohammadian-Hafshejani A, Tarazoj AA, Pouyesh V, Salehiniya H, Colorectal cancer in the world: incidence, mortality and risk factorsBiomedical Research and Therapy 2017 4(10):1656-75.10.15419/bmrat.v4i10.372 [Google Scholar] [CrossRef]
[3]. Global Cancer Observatory. Colorectal cancer 2018. Available at: https://gco.iarc.fr/today/data/factsheets/cancers/10_8_9-Colorectum-fact-sheet.pdf/. Accessed March 25, 2019 [Google Scholar]
[4]. Arnold M, Sierra MS, Laversanne M, Soerjomataram I, Jemal A, Bray F, Global patterns and trends in colorectal cancer incidence and mortalityGut 2017 66(4):683-91.10.1136/gutjnl-2015-31091226818619 [Google Scholar] [CrossRef] [PubMed]
[5]. Jung KW, Won YJ, Kong HJ, Oh CM, Cho H, Lee DH, Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2012Cancer res treat 2015 47(2):12710.4143/crt.2015.06025761484 [Google Scholar] [CrossRef] [PubMed]
[6]. Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012Int J Cancer 2015 136(5):E359-86.10.1002/ijc.2921025220842 [Google Scholar] [CrossRef] [PubMed]
[7]. Jemal A, Center MM, DeSantis C, Ward EM, Global patterns of cancer incidence and mortality rates and trendsCancer Epidemiol Biomarkers Prev 2010 19(8):1893-07.10.1158/1055-9965.EPI-10-043720647400 [Google Scholar] [CrossRef] [PubMed]
[8]. Höffken N, Leichsenring J, Reinacher-Schick A, Clinically relevant, gender-specific differences in colorectal carcinoma (CRC)Zeitschrift fur Gastroenterologie 2015 53(8):782-88.10.1055/s-0035-155347626284326 [Google Scholar] [CrossRef] [PubMed]
[9]. Lahti SJ, Xing M, Kim HS, KRAS status as an independent prognostic factor of survival for unresectable colorectal cancer after Yttrium-90 radioembolization therapyJ Vas Interv Radiol 2015 26(8):1102-11.10.1016/j.jvir.2015.05.03226210240 [Google Scholar] [CrossRef] [PubMed]
[10]. Azzani M, Roslani AC, Su TT, The perceived cancer-related financial hardship among patients and their families: A systematic reviewSupportive Care Cancer 2015 23(3):889-98.10.1007/s00520-014-2474-y25337681 [Google Scholar] [CrossRef] [PubMed]
[11]. Longo CJ, Fitch M, Grignon M, McAndrew A, Understanding the full breadth of cancer-related patient costs in Ontario: A qualitative explorationSupportive Care Cancer 2016 24(11):4541-48.10.1007/s00520-016-3293-027271866 [Google Scholar] [CrossRef] [PubMed]
[12]. Mirolla M, The cost of chronic disease in CanadaGPI Atlantic 2004 Jan 61:67Available at: http://www.gpiatlantic.org/pdf/health/chroniccanada.pdf [Google Scholar]
[13]. Alberts SR, Wagman LD, Chemotherapy for colorectal cancer liver metastasesOncologist 2008 13(10):1063-73.10.1634/theoncologist.2008-014218838438 [Google Scholar] [CrossRef] [PubMed]
[14]. Park YJ, Park KJ, Park JG, Lee KU, Choe KJ, Kim JP, Prognostic factors in 2230 Korean colorectal cancer patients: Analysis of consecutively operated casesWorld J Surg 1999 23(7):721-26.10.1007/PL0001237610390594 [Google Scholar] [CrossRef] [PubMed]
[15]. Roncucci L, Fante R, Losi L, Di Gregorio C, Micheli A, Benatti P, Survival for colon and rectal cancer in a population-based cancer registryEur J Cancer 1996 32(2):295-302.10.1016/0959-8049(95)00532-3 [Google Scholar] [CrossRef]
[16]. Wolmark N, Wieand HS, Rockette HE, Fisher B, Glass A, Lawrence W, The prognostic significance of tumor location and bowel obstruction in Dukes B and C colorectal cancer. Findings from the NSABP clinical trialsAnn Surg 1983 198(6):743-52.10.1097/00000658-198312000-000136357118 [Google Scholar] [CrossRef] [PubMed]
[17]. Halvorsen TB, Seim E, Tumour site: A prognostic factor in colorectal cancer?: A multivariate analysisScandinavian Journal of Gastroenterology 1987 22(1):124-28.10.3109/003655287089918683563405 [Google Scholar] [CrossRef] [PubMed]
[18]. Lee YJ, Lee HR, Nam CM, Hwang UK, Jee SH, White blood cell count and the risk of colon cancerYonsei Med J 2006 47(5):646-56.10.3349/ymj.2006.47.5.64617066508 [Google Scholar] [CrossRef] [PubMed]
[19]. Demeyer D, Mertens B, De Smet S, Ulens M, Mechanisms linking colorectal cancer to the consumption of (processed) red meat: a reviewCrit Rev Food Sci Nutr 2016 56(16):2747-66.10.1080/10408398.2013.87388625975275 [Google Scholar] [CrossRef] [PubMed]
[20]. Radmard AR, Five common cancers in IranArch Iran Med 2010 13(2):143-46. [Google Scholar]
[21]. Nakamura T, Ishikawa H, Mutoh M, Wakabayashi K, Kawano A, Sakai T, Coffee prevents proximal colorectal adenomas in Japanese men: a prospective cohort studyEur J of Cancer Prev 2016 25(5):388-94.10.1097/CEJ.000000000000020326291025 [Google Scholar] [CrossRef] [PubMed]
[22]. Dik VK, van Oijen MG, Smeets HM, Siersema PD, Frequent use of antibiotics is associated with colorectal cancer risk: Results of a nested case-control studyDig Dis Sci 2016 61(1):255-64.10.1007/s10620-015-3828-026289256 [Google Scholar] [CrossRef] [PubMed]
[23]. McSorley ST, Black DH, Horgan PG, McMillan DC, The relationship between tumour stage, systemic inflammation, body composition and survival in patients with colorectal cancerClin Nutr 2018 37(4):1279-85.10.1016/j.clnu.2017.05.01728566220 [Google Scholar] [CrossRef] [PubMed]
[24]. Cox DR, Regression models and life-tablesInBreakthroughs in statistics 1992 New York, NYSpringer:527-541.10.1007/978-1-4612-4380-9_37 [Google Scholar] [CrossRef]
[25]. Borysenko M, Beringer T, Functional Histology 1984 BostonLittle Brown [Google Scholar]
[26]. Claes L, Recknagel S, Ignatius A, Fracture healing under healthy and inflammatory conditionsNat Rev Rheumatol 2012 8(3):13310.1038/nrrheum.2012.122293759 [Google Scholar] [CrossRef] [PubMed]
[27]. King W, Toler K, Woodell-May J, Role of white blood cells in blood-and bone marrow-based autologous therapiesBioMed Research International 2018 2018:651084210.1155/2018/651084230112414 [Google Scholar] [CrossRef] [PubMed]