A Case of Blistering Eruptions in Systemic Lupus Erythematosus
Sarojini Raman1, Abhimanyu Grover2, Prasant Padhan3, Urmila Senapati4
1 Associate Professor, Department of Pathology, KIMS, BBSR, Bhubaneswar, Odisha, India.
2 Postgraduate Resident, Department of Pathology, KIMS, BBSR, Bhubaneswar, Odisha, India.
3 Associate Professor, Department of Pathology, KIMS, PBMH, Bhubaneswar, Odisha, India.
4 Professor and Head, Department of Pathology, KIMS, BBSR, Bhubaneswar, Odisha, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sarojini Raman, Department of Pathology, KIMS, Campus-5, Kiit Campus, BBSR, Bhubaneswar-751024, Odisha, India.
E-mail: sraman10371@gmail.com
Cutaneous vesiculobullous lesions have a wide aetiological spectrum ranging from autoimmunity to medications and infections. Systemic Lupus Erythematosus (SLE) is one of most frequent autoimmune diseases with its cutaneous form being very uncommonly encountered. We report a case of Bullous Systemic Lupus Erythematosus (BSLE). Patient presented with fever, arthalgia and widespread blistering eruptions on face, neck and upper chest wall. Skin biopsy revealed subepidermal bulla and Direct Immunofluorescence (DIF) showed deposition of IgG, IgA, IgM, C3, C1q at the dermoepidermal junction. On treatment lesions healed rapidly. So proper clinical acumina is essential for diagnosis and management of such cases excluding the differentials.
Autoimmunity, Direct, Fluorescent antibody technique, Skin
Case Report
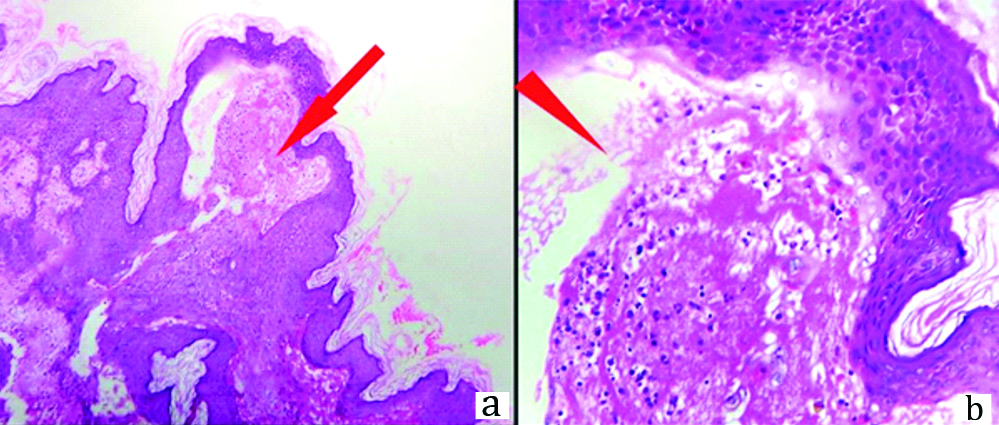
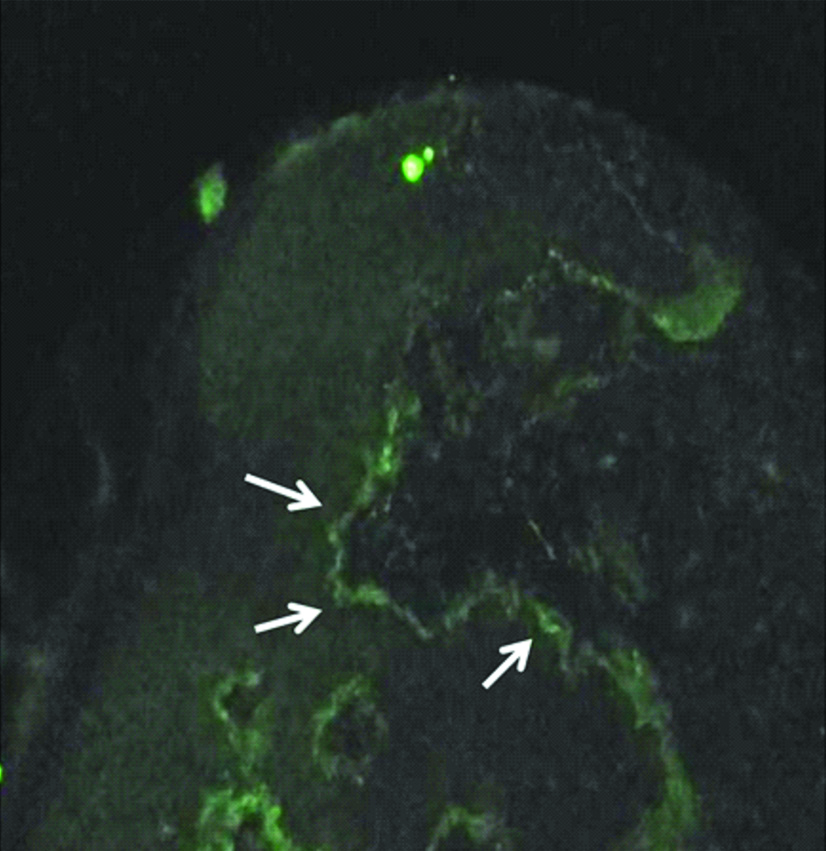
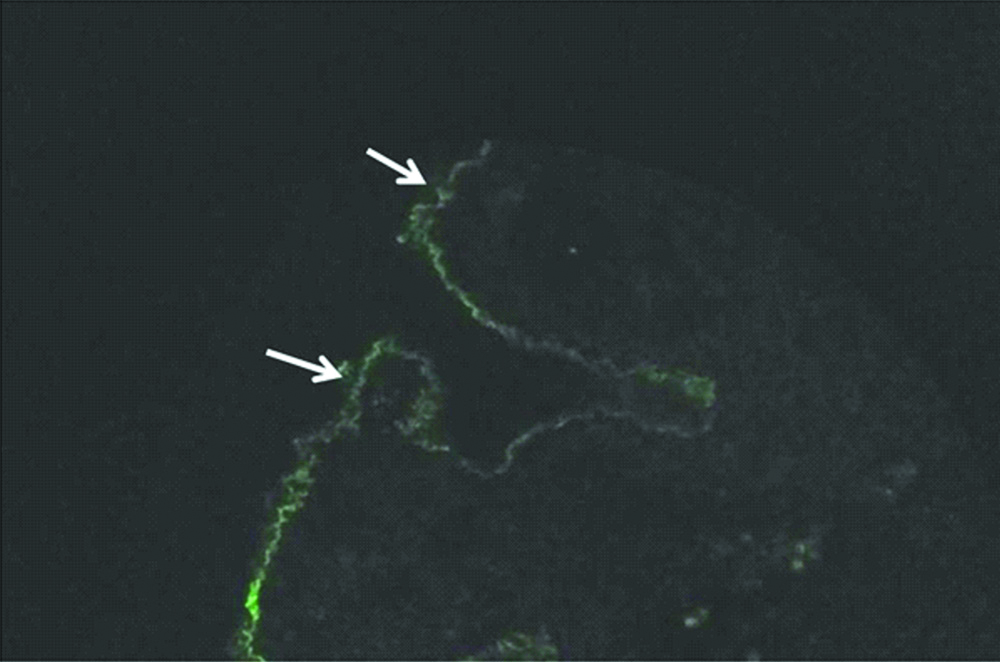
A 27-year-old female presented with intermittent fever, fatigue, arthralgia and myalgia since 2 months in rheumatology Out Patient Department. On examination she had tense progressive unilateral vesicullobullous lesions over face, neck & upper chest wall region in multiple crops, with rupture of vesicles causing draining of clear to turbid and occasionally bloody fluid [Table/Fig-1]. She also had oral ulcers. Nikolsky sign was negative. She had no relevant family/past/drug history. General physical examination revealed moderate pallor, bilateral pitting pedal oedema. Clinical provisional diagnosis was: 1) Bullous pemphigoid; 2) Dermatitis herpetiformis; 3) Bullous SLE. Haematological & biochemical investigations revealed the following: Hb-6.1 g/dL, TRBC-2.84 millions/cmm, MCV-65.1 fL, MCH-21.5 pg/dL, MCHC-33 gm/dL, RDW-CV-19.3, TLC-6810/cmm, Differential Count: N67, L28, M03, E02, B00, TPC-2.89 lac/cmm, Urine protein/creatinine ratio: 5.8 (N<0.2), Serum Urea-55 mg/dL, Serum creatinine-1.2 mg/dL, Urine RE/ME:Alb 3+, RBCs-10-13/hpf, granular cast: 9-10/hpf, Urine protein-193.1 mg/dL, Spot urine creatinine-33.0 mg/dL, Serum C3-27 mg/dL, C4-6 mg/dL, ANA (IIF): homogenous ++ in 1:80 dilutions, Anti ds DNA-214.6 IU/mL. Histopathological & immunofluorescence study was advised in skin biopsy. Grossly, shave biopsy skin tissue measured 0.3×0.2×0.1 cm. Histosection showed an intact neutrophil-rich subepidermal vesicle with neutrophils infiltrating the dermal papillae and lined up along the Dermal-epidermal junction (DEJ) [Table/Fig-2]. There was mild chronic inflammatory cell infiltration surrounding vessels in dermis. Histological diagnosis was Bullous SLE with dermatitis herpetiformis and linear IgA dermatosis as the differentials. DIF revealed 2+ IgG & C1q granular staining at the DEJ, trace IgA, IgM & C3 staining at the DEJ [Table/Fig-3,4]. So based on clinical, serological, histology and immunofluorescence findings final diagnosis was Bullous Systemic Lupus Erythematosus excluding the differentials. The patient was treated with intravenous methylprednisolone 1 mg/day for 3 days followed by 1 mg/kg/day, Hydroxychloroquine 200 mg/day, IV cyclophosphamide 15 mg/kg/month. After 2 weeks all the bullous lesions had healed completely.
Tense vesicles in face and neck (arrow marked).

a) Subepidermal vesicle, H&E stain,100x (arrow marked). b) Neutrophils, karyorrhectic debris in oedematous vesicle, H&E stain, 400x (arrow head marked).
IgG along DEJ, 100x (arrow marked).
C1q along DEJ, 100x (arrow marked).
Discussion
Lupus Erythematosus (LE) is a systemic progressive autoimmune disease characterised by multi organ involvement with a worldwide prevalence of 17-48/100,000 population [1]. Up to 76% of patients show skin involvement. Variable forms of skin involvements have been reported like Subacute Cutaneous LE (SCLE), Chronic Discoid LE (DLE), Bullous SLE (BSLE), linear cutaneous LE, chilblains LE etc. Among these bullous SLE is a rare entity constituting <1% (0.26 per million) of the cases [2,3]. It has characteristic histological appearance, immune deposition pattern, circulating antibody against mostly type VII collagen and frequently parallels internal organ involvement signifying flare of SLE [4].
BSLE is an extremely uncommon subtype of systemic lupus erythematosus with cutaneous affection; first described in 1973 by Pedro and Dahl [5]. As per Gilliam and Sontheimer classification there are many forms of chronic cutaneous SLE, besides BSLE.
Bullous SLE mediated by two different immunological mechanisms. In the first type autoantibodies have been detected against NC1 (non-collagenous 1) domain of Collagen VII which disturbs normal interaction between Extra Cellular Matrix (ECM) & Collagen VII causing dermal-epidermal separation and creation of subepidermal bullae. Presence of neutrophil-predominant inflammation is due to antibodies activating complements and peptides that can mediate leukocyte activation and adherence to the BMZ [6]. In the second type, also referred to as SLE with blisters; blisters develop due to extensive hydropic degeneration of the basal cell layer and severe oedema in the papillary dermis with no immunological mechanism [7]. Immunoelectron Microscopy (IEM) studies have shown the Ig deposits are located either in the upper dermis beneath or on the lamina densa at the DEJ excluding the possibility the blisters due to a primary bullous disease, such as Bullous Pemphigoid (BP) [6].
Camisa and Sharma proposed the diagnostic criteria for BSLE as per American College of Rheumatology Association (ARA) guidelines. It consists of: 1) Clinical- Vesicles and bullae in sun exposed areas; 2) Histopathological - Subepidermal bullae & neutrophilic infiltrations in the dermal papillae; 3) DIF- IgG ± IgM/IgA in the basement membrane zone; 4) IIF: Negative or positive for circulating BMZ antibodies [4,8]. Gammon WR et al., have elucidated another set of diagnostic criterias based on additional IEM ultrastructural features into three catagories. Type I characterised by same Clinical, Histology, DIF and IIF features as above with IEM: Ig deposits codistribute with anchoring fibrils/type VII collagen. Type II have Clinical, Histologic, DIF: Same as type 1, IIF: Negative & IEM: Ig deposits do not co-distribute with anchoring fibrils/type VII Collagen [6,9].
Bullae of BSLE can be discoid or annular with erythematous base, located on sun exposed areas. The differential diagnosis of blistering eruptions in patients with SLE includes Dermatitis Herpetiformis (DH), linear IgA dermatitis, BP & Epidermolysis bullosa acquisita (EBA). Though, DH & linear IgA dermatitis can be differentiated by type & pattern of deposition of direct immunofluorescence. In 1 M NaCl-split skin as a substrate for IIF, bullous pemphigoid antibody localises to the roof of split skin, whereas in bullous SLE antibody binds to base [4]. Epidermolysis bullosa acquisita differs in clinical presentation & response to treatment. BSLE lesions show a dramatic response to dapsone unlike EBA which is frequently treatment resistant. In EBA skin becomes fragile, not seen in BSLE. When in a linear disposition, herpes zoster can be considered in the differential, but it can be easily differentiated by histopathology [7].
Blisters may develop in LE patients due to photosensitivity, acute lupus flare, drugs or a severe form of acute or subacute cutaneous LE that resembles Toxic Epidermal Necrolysis (TEN). In TEN, diffuse or patchy erythema evolves rapidly into flaccid bullae (positive Nikolsky sign) and shows widespread epidermal detachment [9].
The treatment of cutaneous SLE includes topical steroids, calcineurin inhibitors, retinoids, cryotherapy and systemic agents like rituximab, methotrexate, dapsone, intravenous immunoglobulins etc., [3,10].
Conclusion
The case is presented here because though it is an unusual entity, it has distinct clinical, histologic & immunological features which are important clues to arrive at a correct diagnosis excluding the differentials. Once diagnosed the proper treatment can easily cure it. So awareness of this disease entity is must for practising physicians for early recognition and initiation of prompt therapy.
Financial or Other Competing Interests
None.
Patient consent was obtained before publication of this work.
[1]. Patel P, Werth V, Cutaneous lupus erythematosus: A reviewDermatol Clin 2002 20:373-85.10.1016/S0733-8635(02)00016-5 [Google Scholar] [CrossRef]
[2]. Gera C, Williams A, Thomas EA, Calton N, New onset bullous lupus erythematosus in a systemic lupus erythematosus patient after initiation of hydroxychloroquinCHRISMED J Health Res 2014 1(2):110-12.10.4103/2348-3334.134276 [Google Scholar] [CrossRef]
[3]. Harris-Stith R, Erickson QL, Elston DM, Bajar KD, Bullous eruption: A manifestation of lupus erythematosusCutis 2003 72:31-37. [Google Scholar]
[4]. Shirahama S, Yagi H, Furukawa F, Takigawa M, A case of bullous systemic lupus erythematosusDermatology 1994 189(l):95-96.10.1159/0002469418049573 [Google Scholar] [CrossRef] [PubMed]
[5]. Vijayalakshmi AM, Jayavardhana A, Bullous systemic lupus erythematosus and lupus nephritis in a 10-year-old boyIndian Pediatr 2007 44:861-63. [Google Scholar]
[6]. Gammon WR, Briggaman RA, Bullous SLE: A Phenotypically Distinctive but Immunologically Heterogeneous Bullous DisorderJ Invest Dermatol 1993 100(1):28S-34S.10.1111/1523-1747.ep123552108423389 [Google Scholar] [CrossRef] [PubMed]
[7]. Sáez-de-Ocariz M, Espinosa-Rosales F, López-Corella E, León-Bojorge B, Bullous lesions as a manifestation of systemic lupus erythematosus in two Mexican teenagersPediatr Rheumatol online J 2010 8:1910.1186/1546-0096-8-1920615233 [Google Scholar] [CrossRef] [PubMed]
[8]. Camisa C, Sharma HM, Vesiculo bullous systemic lupus erythematosus. Report of two cases and a review of the literatureJ Am Acad Dermatol 1983 9:924-33.10.1016/S0190-9622(83)70210-0 [Google Scholar] [CrossRef]
[9]. Uva L, Miguel D, Pinheiro C, Freitas JP, Gomes MM, Filipe P, Cutaneous manifestations of systemic lupus erythematosusAutoimmune Dis 2012 2012:83429110.1155/2012/83429122888407 [Google Scholar] [CrossRef] [PubMed]
[10]. Wu Y, Kuo TT, Lu P, Chen M, Yang C, Cutaneous lupus erythematosus manifesting as unilateral eyelid erythema and swellingDermatol Sin 2012 (30):25-28.10.1016/j.dsi.2011.09.008 [Google Scholar] [CrossRef]