Neonatal Pemphigus in a Neonate of a Mother Suffering from Pemphigus Vulgaris- A Case Presentation
Sandeep Kulkarni1, Pooja Jaideep Sahu2, Aishwarya Patil3, Bhushan Madke4, Vikrant Saoji5
1 Assistant Professor, Department of Dermatology, Jawaharlal Nehru Medical College, Sawangi, Wardha, Maharashtra, India.
2 Junior Resident, Department of Dermatology, Jawaharlal Nehru Medical College, Sawangi, Wardha, Maharashtra, India.
3 Junior Resident, Department of Dermatology, Jawaharlal Nehru Medical College, Sawangi, Wardha, Maharashtra, India.
4 Professor and Head, Department of Dermatology, Jawaharlal Nehru Medical College, Sawangi, Wardha, Maharashtra, India.
5 Professor, Department of Dermatology, Jawaharlal Nehru Medical College, Sawangi, Wardha, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Pooja Jaideep Sahu, Radhika Bai Hostel, Jawaharlal Nehru Medical College, Sawangi, Wardha-442004, Maharashtra, India.
E-mail: poojasahu61@yahoo.in
Neonatal pemphigus is a transient, self-limiting entity featuring appearance of evanescent blisters in a neonate born to mother diagnosed with immuno-bullous blistering disorders. A case report of neonatal pemphigus born to a 30-year-old female with Pemphigus Vulgaris is being reported. Higher maternal antibody titre causing clinically evident blistering in neonate is not commonly reported. This report, thus, emphasises the need for diagnostic considerations and vigilant surveillance of neonatal pemphigus in neonates born to mothers with immunobullous disorders. Since the cases reported in the literature and the references assessed revealed that neonatal pemphigus is infrequent, but the understanding about the disease permits for an early diagnosis to be made.
Desmoglein, Immunobullous, Immunoflourescence, Pemphigoid gestationis
A 30-year-old female patient pregnant for eight months reported to Department of Dermatology with multiple, painful, slowly progressive oral erosions; crusted lesions on scalp, upper extremities, trunk and back along with interspersed vesicobullous lesions for a duration of three months [Table/Fig-1,2]. Cutaneous erosions were associated with itching and burning sensations. No feature of systemic involvement like fever, malaise or myalgia were seen. Patient was an elderly primigravida with no evidence of aggravation of pre-existing lesions during ongoing pregnancy.
A clinical photograph showing multiple erosions distributed on chest shoulders, abdomen and face.

A clinical photograph showing multiple erosions distributed on back and extremities.

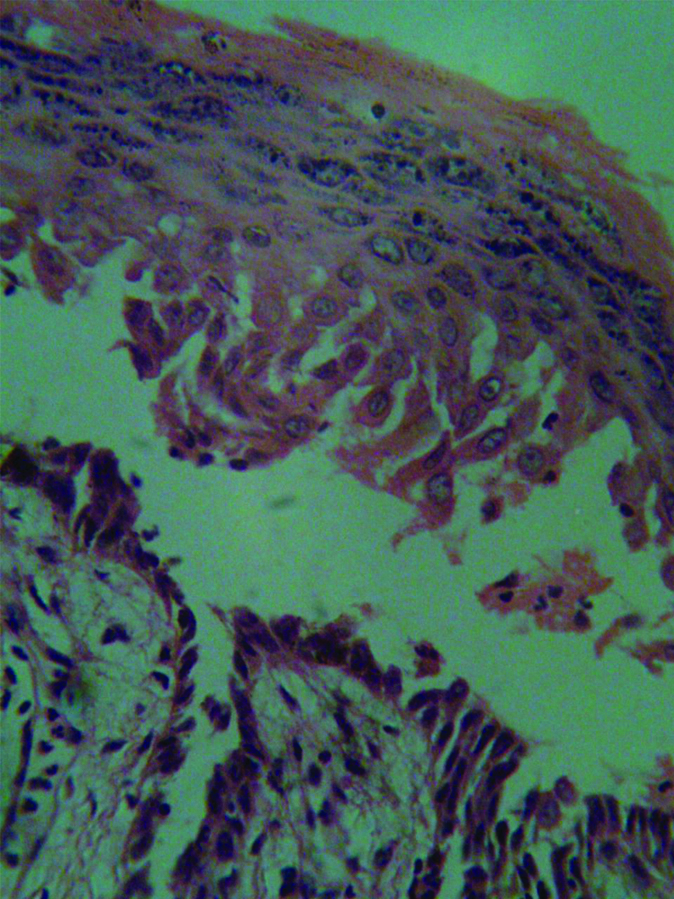
Given the clinical course of the disease with pattern of muco-cutaneous distribution along with morphological characteristics of the lesions; a presumptive diagnosis of autoimmune vesicobullous disorder was kept. Tzanck smear done from few intact vesicular lesions revealed acantholytic cells [Table/Fig-3]. Histopathological examination revealed suprabasal intraepidermal split with basal keratinocytes lining the floor with blister cavity comprising of acantholytic and mononuclear inflammatory cells [Table/Fig-4]. Baseline desmoglein titre was done at a private centre. Direct immunofluorescent microscopy revealed fishnet pattern of immunofluorescence with characteristic suprabasal configuration of immunoreactant distribution.
Tzanck smear showing acantholytic cells.

Photomicrograph showing histopathology of skin biopsy specimen of mother -40x view showing suprabasal intraepidermal split.
Diagnosis of Pemphigus vulgaris was established based on clinico-pathological correlation corroborated by immunofluorescent studies. Pre-treatment baseline titre of anti desmoglein 3 antibodies in serum was estimated by Indirect immunoflorescence for prognostic implications.
Patient was instituted on a regimen containing oral prednisone in dose of 1 mg/kg/day for a period of one week after pre-treatment screening of haematologic, hepatic and renal profiles; anticipating remission of ongoing disease progression. In view of pregnancy near term, the patient was not subjected to high dose pulsed corticosteroid and cyclophosphamide regimens. Obstetrician’s opinion was sought and the patient was delivered by caesarean section after ensuring fetal maturity.
New born revealed few flaccid bullous lesions involving both cheeks and erosions over upper chest and extremities [Table/Fig-5]. On day one of neonatal period which followed an evanescent course to be covered by crusts in 2-3 days to follow. Neonate was managed with oral prednisone in dose 1 mg/kg/day for three days and topical antibiotics for erosions.
Clinical photograph showing multiple erosions and few intact bullae on upper and lower back, and posterior aspect of right upper arm.

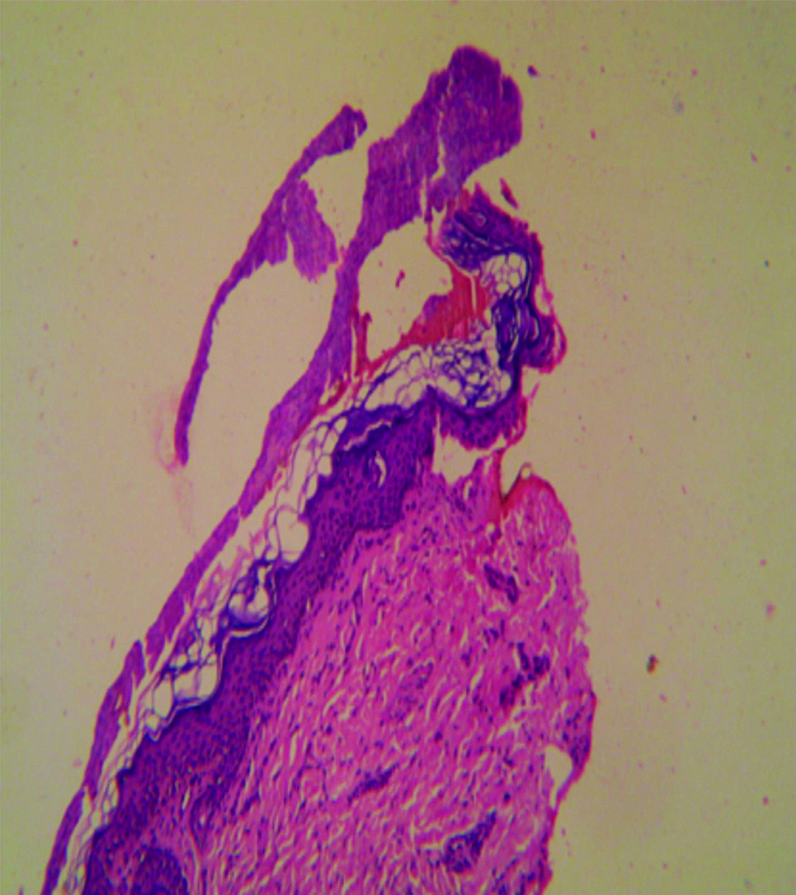
Histopathological examination of specimen taken from vesicular lesion from the neonate revealed intra epidermal-suprabasal blister lined by basal cells forming floor [Table/Fig-6].
Photomicrograph showing histopathology of skin biopsy specimen of neonate -40X view showing suprabasal intraepidermal split.
Based on maternal history and clinical evaluation supported by laboratory parameters; the neonate was diagnosed as a case of neonatal pemphigus born to mother with gestational pemphigus due to passive transfer of maternal antibodies through placental circulation. Written informed consent was obtained from the mother of the newborn.
Discussion
Neonatal pemphigus is a rare, transient, self-limiting entity characterised by appearance of evanescent blisters involving face, trunk and extremities in neonates born to mothers with immunobullous blistering disorders (Pemphigus vulgaris and pemphigoid gestationis) [1]. Blistering occurs as a result of passive transfer of antibodies against Desmoglein 3 and Bullous Pemphigoid Antigen 2 (BPAg2) from maternal placenta [1-3].
Not many cases have been reported on neonatal pemphigus but a few among them were-
Adriana Amarl Carvalho et al., reported a case of newborn male with extensive vesico-bullous lesions on the anterior side of his chest and abdomen at birth. Based on mothers medical history, the patient’s lesions and evaluation of clinical and laboratory evidence, diagnosis of the child was made, the patient was discharged on the 16th day, because the extensive lesions had improved significantly. He was evaluated on the 23rd day where he was in complete remission of the condition [2].
Itsukaichi M et al., reported a case of a dichorionic diamniotic twins born at 37 weeks of gestation by cesarean section to a 34-year-old primigravid Japanese woman, with a high antidesmoglein 3 autoantibody titre, flaccid bullae and erosions on both of the twins’ lips and in their oral cavities at 13 days of age that led to the diagnosis of neonatal Pemphigus Vulgaris. Treatment with petroleum jelly and tube feeding until the erosions were in remission, after which the twins were breastfed, and no new erosions were seen. Symptoms of both twins healed completely within 10 days. The titres of the antidesmoglein 3 autoantibody of both twins were negative at 50 days of age [4].
Pemphigus vulgaris and pemphigoid gestationis are immunobullous disorders characterised by production of autoantibodies against intercellular adhesion proteins desmogleins 1,3 and BPAg2 (BP 180) respectively. These antibodies bring about suprabasal acantholysis due to loss of cellular adhesion molecule and thus underlie the crux of blister formation. Similar blisters may be produced in neonate due to passive transplacental transfer of maternal antibodies to foetus in-utero [1-3]. These antibodies which bring about suprabasal acantholysis result in formation of superficial and flaccid blisters which leave raw erosions on rupture which later are covered by crusts.
Pemphigoid gestationis usually presents with group of tense bullae involving umbilicus, trunk and extremities in a segmental or herpetiform configuration. Maternal serology may show evidence of antibodies for both pemphigus vulgaris and pemphigoid gestationis; but clinical manifestations are usually of one disorder alone [2].
Pregnancy as such is a state of relative depression of T-cell based immunity (CMI) with humoral immunity getting an upper hand; resulting in excessive production of antibodies. Most of the antibodies produced belong to IgG class and the antibody titre determines the severity of clinical manifestations.
The clinico-immunological severity and activity of the disease near term is determined by titre of circulating antibodies which may result in neonatal blistering due to transplacental transfer of maternal IgG proteins [5]. The severity of the manifestations and duration of blistering in neonate is unequivocally guided by maternal antibody titres. Even cases of neonatal pemphigus with clinically asymptomatic mother have been reported [6]. There is homology in nature of desmogleins expressed in maternal oral mucosa and neonatal skin; thereby explaining more probability of neonatal blistering in neonates born to mothers with severe oral disease [1,3] having high titre of antibodies especially against desmoglein 3.
Anecdotal reports [4,7] of neonates presenting with blisters born to mothers with Pemphigus Vulgaris did not reported of protraction of blistering beyond neonatal period because of catabolism of maternal antibodies. Such evanescent and transient blisters in neonates can be managed symptomatically or with short term steroid regimens and usually does not warrant critical reception.
Syphillitic pemphigus (Bullous lesions of congenital syphilis) [8], pemphigus neonatorum (staphylococcal scalded skin syndrome), Transient bullous dermolysis of newborn [9], Transient neonatal pustular melanosis [10], Epidermolysis bullosa simplex may be considered among list of differentials; but are differentiated based on maternal clinical profile and serology, morphology and distribution of neonatal blisters along with diagnostic histopathology and immunoflorescence.
Conclusion(s)
Maternal antibody titres so high to cause clinically evident, transient blistering in neonate born to mother with Pemphigus Vulgaris is commonly observed. Thus, it becomes imperative to exercise more clinical vigilance in approaching such cases. Nonetheless, having self-limiting and transient course; it may still raise panic alarm amongst clinicians from other disciplines as well as parents; which needs to be addressed by appropriate counselling.
Author Declaration:
Financial or Other Competing Interests: No
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Sep 13, 2019
Manual Googling: Nov 14, 2019
iThenticate Software: Nov 30, 2019 (14%)
[1]. Jones Samantha V, Dermatoses of PregnancyIn: Rook’s Textbook of Dermatology, Ninth Edition Griffiths Christopher, Barker Jonathan, Bleiker Tanya, Chalmers Robert and Creamer Daniel 2016 John Wiley & Sons, Ltd:3253 [Google Scholar]
[2]. Carvalho AA, Santos Neto DAD, Carvalho MADR, Eleutério SJP, Xavier AREO, Neonatal pemphigus in an infant born to a mother with pemphigus vulgaris: a case report. pênfigo neonatal em filho de mãe com pênfigo vulgar: relato de casoRev Paul Pediatr 2019 37(1):130-134.10.1590/1984-0462/;2019;37;1;0000430066824 [Google Scholar] [CrossRef] [PubMed]
[3]. Parlowsky T, Welzel J, Amagai M, Zillikens D, Wygold T, Neonatal pemphigus vulgaris: IgG4 autoantibodies to desmoglein 3 induce skin blisters in newbornsJ Am Acad Dermatol 2003 48(4):623-25.10.1067/mjd.2003.17012664033 [Google Scholar] [CrossRef] [PubMed]
[4]. Itsukaichi M, Takakuwa K, Yamaguchi M, Serikawa T, Tanaka K, Kojima K, Twins with neonatal pemphigus vulgaris born to a mother with pemphigus vulgaris: a case reportPediatr Dermatol 2013 30(4):e59-60.10.1111/j.1525-1470.2012.01828.x22937811 [Google Scholar] [CrossRef] [PubMed]
[5]. Amagai M, Tsunoda K, Zillikens D, Nagai T, Nishikawa T, The clinical phenotype of pemphigus is defined by the anti-desmoglein autoantibody profileJ Am Acad Dermatol 1999 40(2 Pt 1):167-70.10.1016/S0190-9622(99)70183-0 [Google Scholar] [CrossRef]
[6]. Bonifazi E, Milioto M, Trashlieva V, Ferrante MR, Mazzotta F, Coviello C, Neonatal pemphigus vulgaris passively transmitted from a clinically asymptomatic motherJ Am Acad Dermatol 2006 55:S113-14.10.1016/j.jaad.2005.03.06417052526 [Google Scholar] [CrossRef] [PubMed]
[7]. Kodagali SS, Subbarao SD, Hiremagaloor R, Pemphigus vulgaris in a neonate and his motherIndian Pediatr 2014 51(4):316-17.PubMed PMID: 24825277 [Google Scholar]
[8]. Kim JK, Choi SR, Lee HJ, Kim DH, Yoon MS, Jo HS, Congenital syphilis presenting with a generalized bullous and pustular eruption in a premature newbornAnnals of Dermatology 2011 23(Suppl 1):S127-30.10.5021/ad.2011.23.S1.S12722028559 [Google Scholar] [CrossRef] [PubMed]
[9]. Fassihi H, Diba VC, Wessagowit V, Dopping-Hepenstal PJ, Jones CA, Burrows NP, Transient bullous dermolysis of the newborn in three generationsBr J Dermatol 2005 153(5):1058-63.10.1111/j.1365-2133.2005.06873.x16225626 [Google Scholar] [CrossRef] [PubMed]
[10]. Ghosh S, Neonatal pustular dermatosis: An overviewIndian Journal of Dermatology 2015 60(2):21110.4103/0019-5154.15255816225626 [Google Scholar] [CrossRef] [PubMed]