Clinical spectrum of Autosomal Dominant Polycystic Kidney Disease (ADPKD) is very wide, ranging from no symptom or mild symptom to renal failure to catastrophic cerebral haemorrhage. Common presentations that can lead to the diagnosis are hypertension, recurrent urinary tract infection, renal failure, abdominal pain or mass, and haematuria. However, cardiovascular complication is the prime cause of morbidity and mortality in ADPKD. Hypertension is the early manifestation which can result in or contribute to other detrimental complications. Here, we report a case of 46-year-old female brought to the emergency department with sudden onset of altered sensorium with no prior history of hypertension, diabetes, heart ailments or any chronic illness. Her Blood Pressure (BP) was 210/100 mmHg with a systolic murmur, palpable kidneys and Glasgow coma scale of 10/15. Funduscopy showed early papilloedema but no retinopathy. Computed Tomography (CT) scan of brain showed Intracerebral Haemorrhage (ICH). Further evaluation led to the diagnosis of ADPKD. Magnetic resonance angiography of brain revealed no aneurysm. She was treated with antihypertensive drugs (telmisartan and nifedepine), prophylactic anticonvulsant (oral levetiracetam) and initially with mannitol as antiedema measure. She was discharged with no residual disability and she is maintaining normal BP on follow-up since 11 months. This case report illustrates that ICH due to undiagnosed or delayed diagnosis of hypertension can still be the leading presentation in ADPKD and more emphasis should be given for screening of masked hypertension which may help in preventing the serious cardiovascular complications.
Case Report
A 46-year-old female was brought to the emergency room with sudden onset of altered sensorium since 6-8 hours; with no history of fever, headache, vomiting or seizure. The accompanying attendants also denied history of hypertension, diabetes, heart diseases, bleeding diathesis or any prolonged illness or hospitalisation in the past or any significant illness in the family.
On physical examination, she had pulse rate of 92 beats/minute with regular rhythm, BP of 210/100 mmHg, body temperature of 99°F, respiratory rate of 18 breaths/minute and pulse oximetry of 92% on room air. Patient was stuporous, restless and Glasgow coma scale was 10/15. Pupils were unequal but reacting to light and plantar response was extensor bilaterally. Both the kidneys were palpable and a systolic murmur was auscultated over the mitral area. Other systemic examinations were unremarkable.
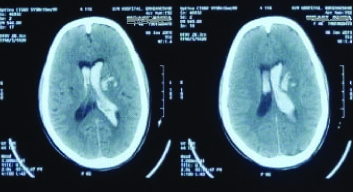
Clinical suspicion of haemorrhagic stroke prompted the physician to suggest a non-contrast CT scan of brain; which showed acute ICH involving left putamen and para-ventricular white matter with intra-ventricular extension suggestive of hypertensive ICH [Table/Fig-1]. Fundus examination showed early paplloedema but no haemorrhage or retinopathy.
CT scan of the brain showing intracerebral haemorrhage involving putamen with intraventricular extension.
Treatment was started with Antihypertensive drug Nifedipine 10mg oral twice daily, 20% Mannitol 100 mL thrice daily intravenously to decrease Intracranial Pressure (ICP), and as about 8% of ICH patients throw seizure within 30 days, prophylactic anti-convulsant drug oral Levetiracetam 500 mg twice daily was also administered besides other symptomatic measures [1].
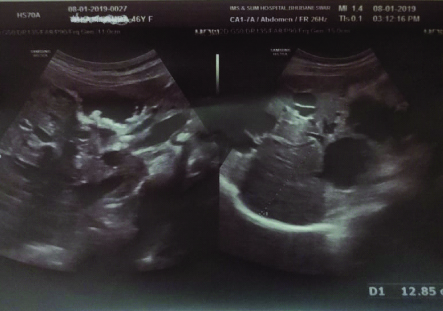
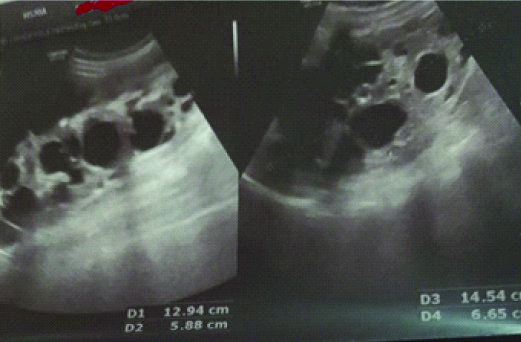
Laboratory investigations like complete blood count, liver function test, blood sugar, serum electrolytes and lipid profile were normal. Serum creatinine was 1.1 mg/dL and eGFR was 69 mL/min/1.73 m2. Urine examination revealed albuminuria of 1+, 0-1 red blood cells and 2-3 leukocytes per high power field. Ultrasonography of abdomen and pelvis showed multiple cysts in the liver and bilateral enlarged kidneys with multiple cysts replacing the parenchyma [Table/Fig-2,3]. Echocardiography revealed mitral valve prolapse with flail anterior mitral leaflet, concentric Left Ventricular Hypertrophy (LVH) and moderate to severe eccentric mitral regurgitation, ejection fraction of 62% and no wall motion abnormality [Table/Fig-4].
Ultrasonography showing multiple cysts in the liver.
Ultrasonography showing bilateral enlarged kidneys with multiple cysts.
Echocardiography of the patient showing mitral valve prolapse and eccentric mitral regurgitation.

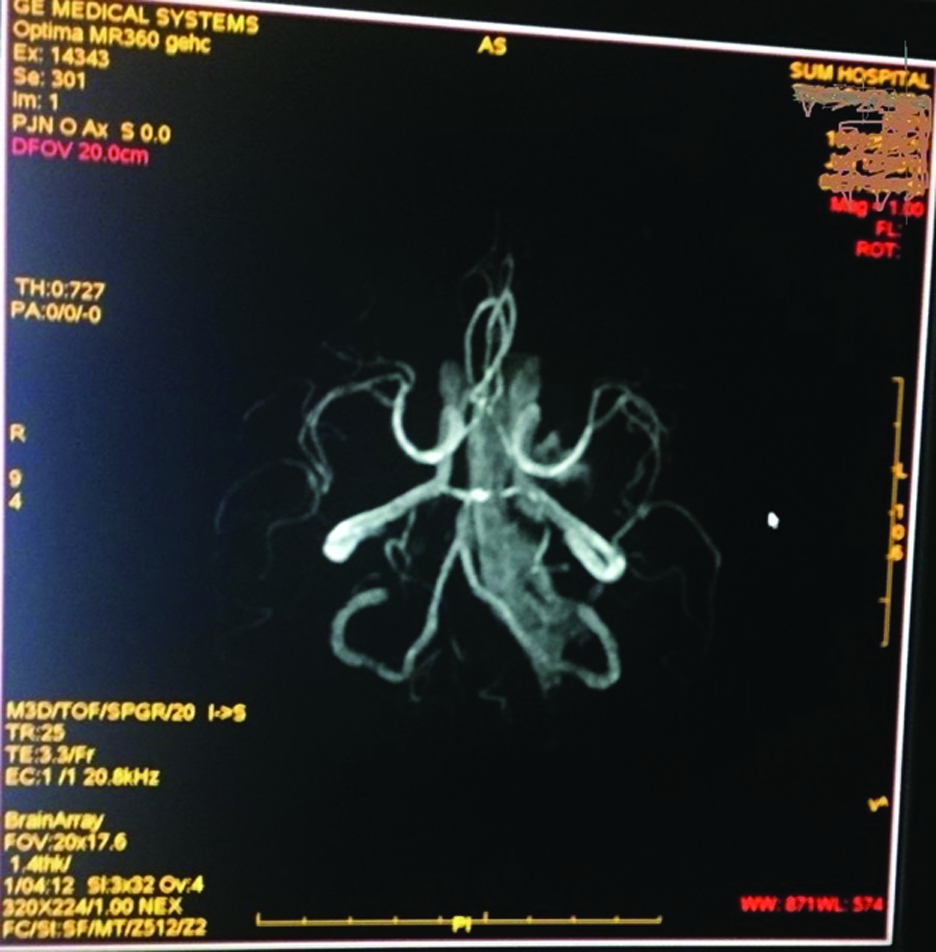
A final diagnosis of ADPKD with hypertensive ICH was made. Magnetic Resonance (MR) angiography of brain was done to find out cerebral aneurysm but detected no aneurysm or narrowing of vessels [Table/Fig-5]. Antihypertensive drug telmisartan 40 mg once daily was added and later escalated to 80 mg once daily to control her high BP.
MR angiography of the brain showing major cerebral vessels with no aneurysm.
Patient regained full consciousness (GCS of 15) on 5th day of hospitalisation and discharged on 11th day of hospitalisation with normal BP of 130/80 mmHg with no residual neurological deficit. She was advised regular follow-up every month and to continue with antihypertensive drugs (telmisartan 80 mg once daily, nifedipine 10mg twice daily) and oral levetiracetam 500 mg twice daily. On follow-up since 11 months, patient is maintaining normal BP and her eGFR was improved to 77 mL/min/1.73 m2 and albuminuria decreased to trace on her last visit.
Discussion
ICH is a medical emergency as 50% of deaths occur within first 48-72 hours due to increased ICP, mass effect or herniation of brain. The most common risk factor attributed to ICH is hypertension and it is an important modifiable risk factor for recurrence as well. Cerebral amyloid angiopathy, advanced age, anticoagulant therapy, prior history of stroke, alcohol and drug abuse are other risk factors [1,2]. Subarachnoid Haemorrhage (SAH) was the closest differential diagnosis in the index case. However, clinically absence of severe headache, meningeal sign and presence of very high BP raised the suspicion of ICH. Chang MY et al., in their comparison study between ICH and SAH in ADPKD patients, reported ICH patients were significantly older and BP on admission was significantly higher [3]. Moreover, CT scan and MR angiography of brain ruled out SAH in the index case. Further, ICH is two times more common than SAH and haemorrhage into basal ganglion especially putamen is the typical site for hypertensive ICH [1,2].
Polycystic kidney disease can be Autosomal Dominant or Autosomal Recessive (ARPKD), depending on the inheritance pattern. A significant proportion of ARPKD patients succumb in neonatal life or manifest in early childhood whereas ADPKD is the most common form and frequently diagnosed in adults [4,5]. The characteristic feature of ADPKD is continuous development of fluid-filled cysts replacing the normal tissues of both kidneys and eventually leading to end-stage renal failure [4]. Most of the patients with this most common inherited kidney disease remain asymptomatic in early life. It is usually diagnosed in fourth to fifth decade of life on presentation with hypertension or abdominal masses or flank pain. Other common presentations are recurrent cyst infection or pyelonephritis, haematuria, kidney stones besides renal failure [4,5]. Diagnosis in the index patient was made considering the age, presence of liver cysts, and mitral valve prolapse besides enlarged kidneys with multiple cysts. Ultrasonography is the diagnostic modality of choice and age-dependent criteria in those with positive family history are established whereas without family history; bilateral enlarged kidneys with >10 cysts in each make the diagnosis with consideration of age, associated manifestations and absence of other genetic cystic disorders in the family [6-8].
The main extra-renal complication is liver cysts and found in >80% of patients of ADPKD [9]. However, cardiovascular complication is the major cause of mortality and morbidity in these patients. Florijn KW et al., reported the mortality in ADPKD as 1.6-3.2 times higher than the general population [10]. Hypertension is the most frequent cardiovascular complication and manifests in 50-70% of cases, even before the renal function impairment [5,8]. Multiple factors including increased activation of renin-angiotensin-aldosterone system, increased sympathetic activity and endothelial dysfunction play a role in the pathogenesis of hypertension [5]. Other common complications are LVH (~50%), mitral regurgitation (~30%), mitral valve prolapse (~25%), aortic regurgitation (10-20%) and intracranial aneurysm (6-20%) [5,9]. LVH is an independent risk factor for cardiovascular mortality and also seen in normotensive ADPKD patients where the possible causative factors are ambulatory BP, increased level of fibroblast growth factor 23, insulin resistance and ACE gene polymorphism [5,11]. Echocardiographic evaluation is recommended for all ADPKD patients with a murmur. But, mitral valve prolapse attribute neither to the progression of renal failure nor to the cardiovascular mortality [9,11]. Not only, uncontrolled hypertension can cause cerebral haemorrhage but it may predispose to aneurysmal rupture as well. Intracranial aneurysm is a lethal complication and its rupture can cause mortality rate of 4-7% and residual neurologic deficits in up to 50% of survivors [5,11]. The most common site for aneurysm (80-90% of cases) is anterior circle of Willis [8].
In a retrospective study including 900 cases of ICH, Ryu SJ reported 11.2% of PKD patients had cerebral haemorrhage; of which 8% had hypertensive bleed and inadequately treated for long-standing hypertension [12]. The index case presented with ICH with no aneurysm, retinopathy or prior history of hypertension but masked hypertension cannot be ruled out. The prevalence of masked hypertension in ADPKD is reported as high as 29.7% in adults and even higher in children and adolescents [13-15]. Ambulatory BP monitoring is critical to detect BP variability, non-dipper and masked hypertension and they all bear a great risk for cardiovascular complications [13-16].
Hypertension, apart from being a potential risk factor for cardiovascular mortality and morbidity; also augments the progression of kidney failure in ADPKD. Therefore, an early and efficacious control of hypertension is warranted. The most noted HALT-PKD study also showed that early and strict control of BP results in significant overall improvement [17]. Increased activation of renin-angiotensin-aldosterone system is the principal factor for the development of hypertension in ADPKD and hence ACE (Angiotensin Converting Enzyme) inhibitor or ARB (Angiotensin Receptor II Blocker) is the recommended first-line drug but combination of ACE and ARB has no added advantage [17]. Beta-blocker, calcium channel blocker or thiazide diuretics can be used in patients with contraindication to ACE inhibitor/ARB or to further control the BP [16,18]. So far, vasopressin-2-receptor antagonist Tolvaptan is the only FDA approved drug for ADPKD and indicated only in patients with rapidly progressing renal failure [7].
By the age of 60 years, about 50% of ADPKD patients progress to end-stage renal failure [8]. Total Kidney Volume (TKV) or more precisely height-adjusted TKV is the most important prognostic factor for ADPKD that determines the risk and rate of progression to end-stage renal failure. The larger the TKV, more rapid is the progression and loss of GFR. Again, age is another important prognostic factor and proteinuria, obesity, early onset of hypertension, multiparous women with hypertension and PKD1 mutation are other prognostic factors [7,8]. Further, in a retrospective cohort study it was observed that ADPKD, in patients on chronic dialysis is a significant risk factor for intracranial haemorrhage [19]. Approximately, 40% of patients with hypertensive ICH die within a month but survivors can have a near complete recovery [1,2].
Conclusion(s)
The Intracerebral Haemorrhage (ICH) due to undiagnosed or delayed diagnosis of hypertension can be the leading presentation in ADPKD patient even today. A robust screening method for hypertension especially masked hypertension with ambulatory BP monitoring for early diagnosis and control of hypertension may reduce the severe cardiovascular complications and thereby morbidity and mortality.
[1]. Aguilar MI, Brott TG, Update in intracerebral hemorrhageThe Neurohospitalist 2011 1(3):148-59.10.1177/194187521140905023983850 [Google Scholar] [CrossRef] [PubMed]
[2]. Smith WS, Johnston SC, Hemphill JC III, Intracranial HemorrhageHarrison’s Principle of Internal Medicine 2018 20th Ed(chap. 421)McGraw Hill:3091-95. [Google Scholar]
[3]. Chang MY, Kuok CM, Chen YC, Ryu SJ, Tian YC, Wu-Chou YH, Comparison of intracerebral hemorrhage and subarachnoid hemorrhage in patients with autosomal-dominant polycystic kidney diseaseNephron Clin Pract 2010 114(2):158-64.10.1159/00025656819907190 [Google Scholar] [CrossRef] [PubMed]
[4]. Harris PC, Torres VE, Polycystic kidney diseaseAnnu Rev Med 2009 60:321-37.10.1146/annurev.med.60.101707.12571218947299 [Google Scholar] [CrossRef] [PubMed]
[5]. Ecder T, Schrier RW, Cardiovascular abnormalities in autosomal-dominant polycystic kidney diseaseNat Rev Nephrol 2009 5(4):221-28.10.1038/nrneph.2009.1319322187 [Google Scholar] [CrossRef] [PubMed]
[6]. Pei Y, Obaji J, Dupuis A, Paterson AD, Magistroni R, Dicks E, Unified criteria for ultrasonographic diagnosis of ADPKDJ Am Soc Nephrol 2009 20(1):205-12.10.1681/ASN.200805050718945943 [Google Scholar] [CrossRef] [PubMed]
[7]. Rastogi A, Ameen KM, Al-Baghdadi M, Shaffer K, Nobakht N, Kamgar M, Autosomal dominant polycystic kidney disease: Updated perspectivesTherapeutics and Clinical Risk Management 2019 15:1041-52.10.2147/TCRM.S19624431692482 [Google Scholar] [CrossRef] [PubMed]
[8]. Chebib FT, Torres VE, Autosomal dominant polycystic kidney disease: Core curriculumAm J Kidney Dis 2016 67(5):792-810.10.1053/j.ajkd.2015.07.03726530876 [Google Scholar] [CrossRef] [PubMed]
[9]. Luciano RL, Dahl NK, Extra-renal manifestations of autosomal dominant polycystic kidney disease (ADPKD): Considerations for routine screening and managementNephrol Dial Transplant 2014 29:247-54.10.1093/ndt/gft43724215018 [Google Scholar] [CrossRef] [PubMed]
[10]. Florijn KW, Noteboom WM, van Saase JL, Chang PC, Breuning MH, Vandenbroucke JP, A century of mortality in five large families with polycystic kidney diseaseAm J Kidney Dis 1995 25:370-74.10.1016/0272-6386(95)90096-9 [Google Scholar] [CrossRef]
[11]. Krishnappa V, Vinod P, Deverakonda D, Raina R, Autosomal dominant polycystic kidney disease and the heart and brainCleve Clin J Med 2017 84(6):471-81.10.3949/ccjm.84a.1610728628430 [Google Scholar] [CrossRef] [PubMed]
[12]. Ryu SJ, Intracranial hemorrhage in patients with polycystic kidney diseaseStroke 1990 21:291-94.10.1161/01.STR.21.2.2912305406 [Google Scholar] [CrossRef] [PubMed]
[13]. Sans AL, Roca-Cusachs A, Torra R, Calero F, Arias P, Ballarin J, Relationship between renal size and blood pressure profile in patients with autosomal dominant polycystic kidney disease without renal failureNefrologia 2010 30(5):567-72. [Google Scholar]
[14]. Massella L, Mekahli D, Paripovic D, Prikhodina L, Godefroid N, Niemirska A, Prevalence of hypertension in children with early-stage ADPKDClin J Am Soc Nephrol 2018 13(6):874-83.10.2215/CJN.1140101729674338 [Google Scholar] [CrossRef] [PubMed]
[15]. Valero FA, Martinez-Vea A, Bardaj A, Gutirrez C, Garcia C, Richart C, Ambulatory blood pressure and left ventricular mass in normotensive patients with autosomal dominant polycystic kidney diseaseJ Am Soc Nephrol 1999 10:1020-22. [Google Scholar]
[16]. Rahbari-Oskoui F, Williams O, Chapman A, Mechanisms and management of hypertension in autosomal dominant polycystic kidney diseaseNephrol Dial Transplant 2014 29:2194-201.10.1093/ndt/gft51324463189 [Google Scholar] [CrossRef] [PubMed]
[17]. Schrier RW, Abebe KZ, Perrone RD, Torres VE, Braun WE, Steinman TI, Blood pressure in early autosomal dominant polycystic kidney diseaseN Engl J Med 2014 371(24):2255-66.10.1056/NEJMoa140268525399733 [Google Scholar] [CrossRef] [PubMed]
[18]. Helal I, Al-Rowaie F, Abderrahim E, Kheder A, Update on pathogenesis, management, and treatment of hypertension in autosomal dominant polycystic kidney diseaseSaudi J Kidney Dis Transpl 2017 28(2):253-60.10.4103/1319-2442.20277428352004 [Google Scholar] [CrossRef] [PubMed]
[19]. Yoo DJ, Agodoa L, Yuan CM, Abbott KC, Nee R, Risk of intracranial hemorrhage associated with autosomal dominant polycystic kidney disease in patients with end stage renal diseaseBMC Nephrology 2014 15:3910.1186/1471-2369-15-3924571546 [Google Scholar] [CrossRef] [PubMed]