Bupivacaine is the most common Local Anaesthetic Agent (LA) used intrathecally for caesarean section [1]. Adjuvants are added, to decrease the dose of LA, improve the quality of anaesthesia and to prolong the duration of postoperative analgesia [2-5].
The onset, level and quality of Subarachnoid Block (SAB) depends upon factor affecting intrathecal spread of LA [6]. Density of LA influences its spread [7,8]. In an in-vitro study, the mean densities of fentanyl and morphine were found to be 0.9957 and 1.0013 respectively, whereas the density of hyperbaric bupivacaine was 1.0262 [9]. The mean density of Cerebrospinal Fluid (CSF) in term pregnant females is 1.00030 [10].
Alterations in the baricity of a solution to the extent of 0.0006 g/mL can alter the spread of local anaesthetic solution in CSF [11]. Mixing adjuvant during spinal anaesthesia in a single syringe before injecting the drugs intrathecally is an usual practice, which may affect the density of both the drugs, hence affecting their spread in CSF as well as action [6,12,13].
Use of LA and adjuvants separately in spinal anaesthesia may have different effects than using them as mixture. Using two separate syringes for hyperbaric Bupivacaine & Fentanyl can minimise the effect on density of both the drugs.
The aim of the study was to compare Intrathecal Fentanyl with hyperbaric Bupivacaine as either a mixture or sequentially in elective caesarean section under spinal anaesthesia in the terms of primary objectives as block characteristics (both sensory and motor block), haemodynamic changes {Blood Pressure (BP) and Heart Rate (HR)}, Duration of analgesia and secondary objectives as Fetal outcome (in terms of APGAR score) side effects if any.
Materials and Methods
With due approval from Ethical Committee (F.1/Acad/MC/JU/18/5155, 27.03.2018) Dr SN Medical College and associated groups of hospitals, Jodhpur (Raj) and Clinical Trials Registry India (CTRI), a prospective, hospital based, single-blinded, randomised, controlled, comparative study was carried out in the Department of Anaesthesiology on patients undergoing elective LSCS. Study period was from December 2018 to March 2019 and study carried out in Janana wing of MDM hospital and Umaid hospital, Jodhpur. This study is registered under the number CTRI/2018/12/016698.
Inclusion criteria: Parturients with singleton pregnancy, American Society of Anaesthesiologist (ASA) I and II physical status, weighing 50-80 kg, height 150-170 cm were included in the study.
Exclusion criteria: Parturient with multiple pregnancies, PIH, major systemic disease, any contraindication of SAB and having history of hypersensitivity to LA and fentanyl were excluded from study.
A written informed consent was taken from all patients participating in the study after complete explanation about the study protocol, anaesthetic technique, merits and demerits of the procedure and perioperative course of anaesthesia.
During pre-operative visits, patients detailed history, general physical examination and systemic examination was carried out. Basic demographic data like age, height, weight and all routine investigations were recorded.
On the day of surgery, in the operating room, patient was received with fasting of at least 8 hour, monitor for HR, non-invasive BP, electrocardiography and oxygen saturation (SpO2) was connected and baseline parameters were recorded.
After establishing 18 gauge venous cannula, Inj. Ranitidine 50 mg and Inj. Metoclopramide 10 mg I.V. was given. By computer generated data, patients were randomly allocated into one of the two groups- group M and group S.
Group M parturients received spinal anaesthesia using 7.5 mg bupivacaine heavy 0.5% premixed with 25 μg fentanyl in the same syringe. Group S parturients received the same medications sequentially without premixing using two different syringes; in the first syringe 25 μg fentanyl and in the second syringe 7.5 mg bupivacaine 0.5% without barbotage.
Preparation of drugs and SAB was given by the same anaesthesiologist. The vitals were recorded by another anaesthesiologist who was unaware to the technique and the drug used for spinal anaesthesia.
In sitting position, using all aseptic precautions, Quincke spinal needle, 25-gauge, was inserted in the L3-4 inter-vertebral space after checking free flow of CSF and negative aspiration of blood, drug was injected. Timing between the first and second syringes was kept as low as possible to prevent CSF loss with part of the fentanyl dose. Then the parturient was asked to lie down immediately after bupivacaine injection, 15°-20° left displacement of uterus was done until birth of baby by keeping a wedge under the right buttock. Vitals recorded just after the anaesthesia was considered to be at 0 time. Co-loading was done with Ringer’s lactate solution in a dose of 15 ml/kg started as fast drip during and continued after spinal anaesthesia. Surgery was allowed after achieving adequate level of block (T5). In cases with failure of SAB, general anaesthesia was given and such patients were excluded from the study.
Haemodynamic parameters such as HR, Systolic Blood Pressure (SBP), Diastolic Blood Pressure (DBP) were monitored at every 3 minutes for initial 15 minutes, than at every 5 minute for 30 minutes, and at every 10 minutes for next 30 minutes, and at every 15 minutes for next one hour. Every 30 minutes for next one hour, than at 1 hour interval for next 3 hour in post-operative room. Any episode of hypotension and bradycardia during the procedure was noted. Hypotension (Fall in BP by >20% of baseline values) was treated with a rapid infusion of crystalloids (200 mL) and a bolus of Ephedrine 6 mg intravenous (IV) was administered if hypotension persisted. Bradycardia (Fall in HR>20% of baseline values) was treated with injection atropine 0.6 mg IV. Electrocardiogram and oxygen saturation were monitored continuously.
Onset of Sensory block and peak level was assessed by pin prick method using a 20 gauge hypodermic needle, after 1 minute of SAB and every 1 minute until the level was established for four consecutive tests, after that assessment continued until 2 segment regression occur.
Onset of Motor block was assessed by Modified Bromage scale [14] Time to reach Modified Bromage scale 3 is taken as motor block onset time and assessed after 1 minute of spinal anaesthesia and after every minute till Modified Bromage 1 block was achieved. Duration of motor block was considered as time from motor block onset to reach Modified Bromage scale 6. Modified Bromage Score- Grade 1: Complete block (unable to move feet or knee); Grade 2: Almost complete block (able to move feet only); Grade 3: Partial block (Just able to move knees); Grade 4: Detectable weakness of hip flexion while supine (full flexion of knees); Grade 5: No detectable weakness of hip flexion while supine; Grade 6: Able to perform partial knee bend.
Evaluation of Block
Block start time (needle insertion) was recorded
Onset of sensory and motor block
Peak level of sensory block
Time to achieve maximum motor blockade, sensory blockade and duration of surgical procedure was also recorded
Two segment regression of sensory block from peak level
Duration of motor block
All times were recorded after intrathecal injection of the spinal anaesthetic drugs. Time of first analgesic requirement for post-operative pain relief was recorded.
Spinal anaesthesia-related side-effects; nausea, vomiting, respiratory depression, or shivering were recorded and managed. Itching was graded and managed as: Mild, Moderate and Severe [15]. Mild itching need no treatment, Moderate was treated with IV Chlorpheniramine Maleate, 10 mg, if not responding or in the case of severe itching IV Naloxone was given in a dose titrated according to the effect. Neonatal outcome was recorded in the form of APGAR score at 1 and 5 min.
The intraoperative quality of surgical anaesthesia was estimated using Ochsner Health System which measures patient satisfaction in four grades: Excellent- The patient felt comfortable during operation, no complaints; Good- A little discomfort but no need for additive medication; Fair- Discomfort, but controlled by nitrous oxide mask with or without fentanyl; and Poor- Unable to be controlled even with additive medication and shift to general anaesthesia was mandatory [16].
Statistical Analysis
Based on a previous study [15] using a SPSS software version 22.0 (SPSS Inc, Chicago, II, USA), the sample size in this study was 80 in each group assuming α error=0.05 and β error=0.2 or power (1-β)=0.8(80% power and 95% confidence level) and 5% drop out. Data were analysed using IBM SPSS. Statistics Windows, Version 20.0 (Trial version). The statistical significant difference among groups was determined by the unpaired t-test, chi-square test and fisher-exact test. The level of significance was set at p<0.05. Descriptive data were presented as mean±SD. Continuous data were analysed by student unpaired t-tests and chi-square test to assess the statistical difference between groups.
Results
One hundred and eighty parturients were assessed for eligibility, 16 did not fulfill inclusion criteria and were excluded. Four parturients refused participation in research study. Thus, finally 160 parturients were randomised in two groups (80 in each group). All the parturients in each group were analysed [Table/Fig-1]. Demographic parameters such as age, height, weight and American Society of Anaesthesiologists (ASA) status were comparable between groups [Table/Fig-2]. All patients passed smooth intraoperative course without complications within a mean duration range 40-55 minutes with no significant difference between the groups [Table/Fig-2].

Demographic parameters in both groups.
| Parameter | Group M | Group S | p-value |
|---|
| Age (years)(Mean±SD†) | 24.66±3.39 | 25.13±3.87 | 0.410 |
| Weight (kg)(Mean±SD†) | 65.45±3.95 | 64.27±4.28 | 0.073 |
| Height (cm)(Mean±SD†) | 157.16±4.05 | 157.29±4.21 | 0.844 |
| Duration of surgery (minutes)(Mean±SD†) | 45.31±5.75 | 45.26±5.86 | 0.956 |
| ASA* grading | ASA I (%) | 85.00 | 88.75 | >0.05 |
| ASA II (%) | 15.00 | 11.25 | >0.05 |
†SD: Standard Deviation; *ASA: American society of anaesthesiologist
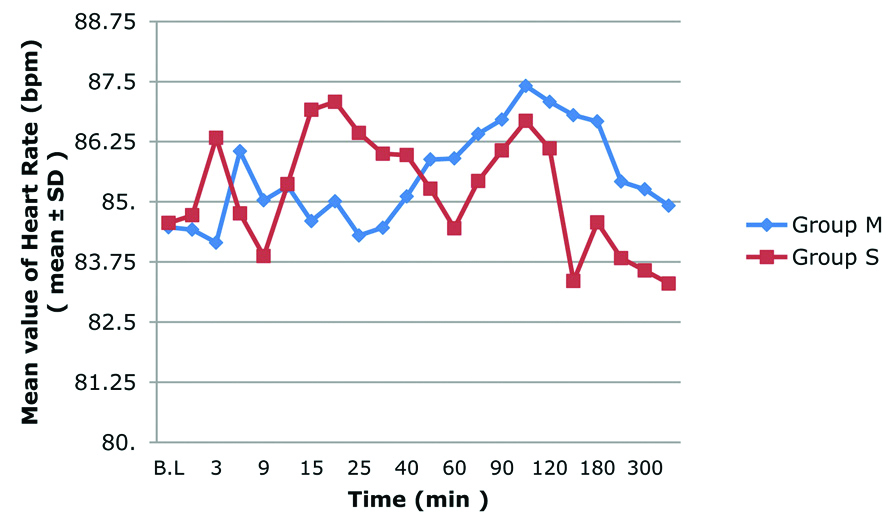
In this study, there was no significant difference in incidence of bradycardia [Table/Fig-3,4]. In group M, 8 (10%) patients developed bradycardia and in group S, 7 (8.75%) patients developed bradycardia. All patients responded to Inj. Atropine 0.6 mg IV bolus.
Comparison of Heart Rate (HR) in both groups.
Comparison of side effects, *By Fischer-exact test (level of significance at p<0.05).
| Complications | Group M | Group S | p-value* |
|---|
| N | % | N | % |
|---|
| Hypotension | Early (within 10 min) | 25 | 31.25 | 8 | 10.0 | <0.05 |
| Overall | 30 | 37.50 | 18 | 22.50 | 0.501 |
| Bradycardia | 8 | 10.00 | 7 | 8.75 | 1.000 |
| Nausea/Vomiting | 12 | 15.00 | 8 | 10.00 | 0.474 |
| Itching | 16 | 20.00 | 20 | 25.00 | 0.57 |
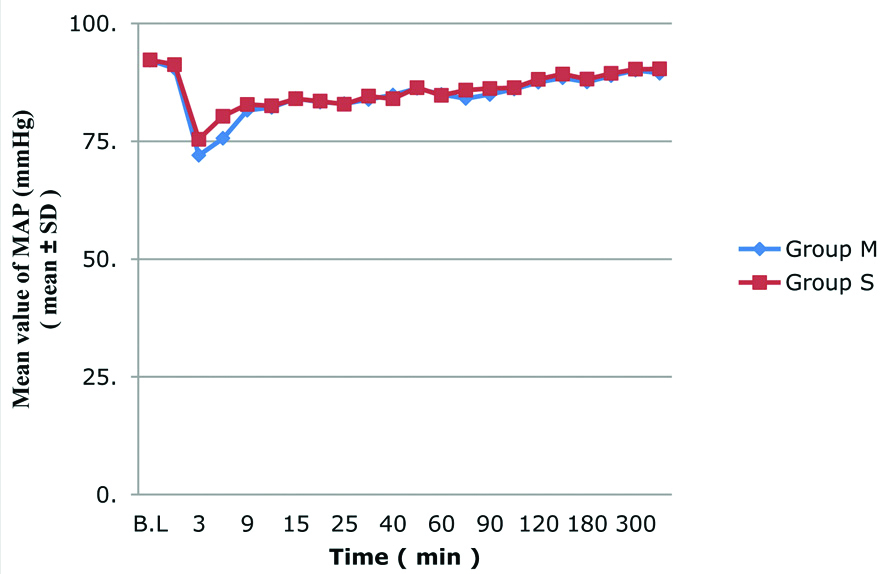
Overall, hypotension was recorded in 30 patients (37.50%) in Group M and 18 patients (22.50%) in Group S without significant difference. Early hypotension occurred in 25 patients (31.25%) in Group M at 3 minute and 6 minutes which was significantly higher than those in 8 patients of Group S (10.0%) [Table/Fig-4,5].
Comparison of Mean Arterial Pressure in both groups.
There was no significant difference between onset time and peak level (T4-T6) of sensory block in both the groups. Time to reach the peak level of sensory block was significantly higher in group M (4.95±1.10 min) as compared to group S (4.56±1.68 min), with range of time between 3-8 minute. Time for 2 segment regression from peak sensory block was higher in group S (143.75±11.4 min) as compared to group M (107.6±7.55 min) that was statistically significant (p<0.0001) [Table/Fig-6].
Comparison of block characteristics in both groups.
| Parameter | Group M (Mean±SD) | Group S (Mean±SD) | p-value |
|---|
| Onset time of sensory block (minutes) | 1.02±0.09 | 1.00±0.10 | 0.083 |
| Onset time of motor block (Min) | 2.02±0.63 | 1.98±0.64 | 0.711 |
| Time to reach peak level of sensory block (Min) | 4.95±1.10 | 4.56±1.68 | 0.032 |
| Duration of motor block (Min) | 156.7±12.39 | 182±12.42 | <0.0001 |
| Duration of sensory block (Min) | 283.37±28.37 | 304.62±25.89 | <0.0001 |
| Two segment regression time for sensory block (Min) | 107.6±7.55 | 143.75±11.40 | <0.0001 |
| Peak level of sensory block | T4 (%) | 31.25 | 32.50 | 0.911 |
| T5 (%) | 51.25 | 52.50 |
| T6 (%) | 17.50 | 15.00 |
†SD: Standard Deviation; *ASA: American society of anaesthesiologist; level of significance at p<0.05
In the present study, there was no significant difference between onset time of motor block in both the groups. Time to achieve complete motor block was earlier in group S (5.33±0.98 min) than group M (5.76±1.02 min). The p-value was 0.008, which was statistically significant. Duration of motor block was significantly higher in group S (182±12.42 min) than group M (156.7±12.39 min), p-value <0.0001 [Table/Fig-6]. Time to 1st dose of analgesia required was higher in group S (304.62±25.89 min) as compare to group M (283.37±28.37 min). It was statistically significant, p-value <0.0001 [Table/Fig-6].
There was no significant difference in the incidence of itching and nausea /vomiting [Table/Fig-4]. In this study, 37.50% patients in group S labeled the effect as excellent and they would prefer this technique in future, whereas 12.50% patients in group M labeled it excellent. The difference in both the groups was found to be statistically significant (p<0.001) [Table/Fig-7].
Comparison of patients satisfaction score.
| Satisfaction score | Group M | Group S |
|---|
| N | % | N | % |
|---|
| Poor | 0 | 0.0 | 0 | 0.0% |
| Fair | 28 | 35.00 | 19 | 23.75 |
| Good | 42 | 52.50 | 31 | 38.75 |
| Excellent | 10 | 12.50 | 30 | 37.50 |
| Total | 80 | 100.00 | 80 | 100.00 |
There was no significant difference in the APGAR Score at 1 minute and 5 minute in both the groups [Table/Fig-8].
Comparison of APGAR score in both groups.
| Time | APGAR score | t-value | p-value |
|---|
| Group M (Mean±SD) | Group S (Mean±SD) |
|---|
| 1 min | 8.87±0.46 | 8.78±0.60 | 1.024 | 0.307 |
| 5 min | 9.37±0.48 | 9.27±0.52 | 1.246 | 0.214 |
Discussion
The present study aimed to compare effects of fentanyl and hyperbaric bupivacaines sequentially versus as a mixture in single syringe in Caesarean section. Intrathecal injection of Fentanyl and hyperbaric Bupivacaine sequentially provided better quality of sensory block and less frequency of hypotension in comparison to when used as a mixture. Time to reach the peak level of sensory, motor block was higher in group M. Two segment regression of sensory block, time to first rescue analgesia and duration of motor block was higher in group S.
As regards the outcome incidence of hypotension at 3 and 6 minutes after administration of drug was less in group S than group M [Table/Fig-5]. The mixture of hypobaric fentanyl and hyperbaric bupivacaine sinks down when patient is in sitting posture, but when patients lies down, both the drugs creep up together and act at same level; hence the early hypotension in group M. When used sequentially, hyperbaric bupivacaine being denser than fentanyl, sinks more to a lower level and takes a longer time to reach the final level; hence the delayed onset of the sympathetic block giving time for a compensatory mechanism to prevent hypotension. This delaying of onset of sympathetic block match the results of other studies [15,17-19] which concluded that isobaric bupivacaine produced more rapid onset of hypotension compared to hyperbaric bupivacaine.
In this study, mean time to onset of sensory and motor block was lesser in group S than group M that was statistically not significant [Table/Fig-6]. Keera AAI and Elnabtity AMA, found similar result in their study [15]. Sachan P et al., did the same study but with clonidine instead of fentanyl and concluded that onset of sensory and motor block was faster with separate injection group than with mix injection group, but was not statistically significant [13]. Joshi P et al., Bansal N and Ladi SD have done similar study but found significant difference [17,20].
Mean time to peak sensory block level and to complete motor block was higher in group M than group S, which was statistically significant in present study [Table/Fig-6]. This difference might be due to the preferential cephalad spread of fentanyl because of its hypobaric nature which is lost when the drugs are premixed. Desai S et al., also observed that the time to reach highest level of block was less when Morphine and Fentanyl were administered sequentially with spinal anaesthesia than when given as a mixture [12]. Similar results were found in some other studies too [13,21].
Mean time to segment regression of sensory block and total duration of motor block observed were less in group M than group S, that were statistically highly significant in the present study [Table/Fig-6]. Mean time to 1st rescue analgesia was required early in group M (283.37±28.37 minute) than group S (304.62±25.89 minute), which was statistically highly significant. (p<0.0001) This difference might be due to the fact that injecting Fentanyl and Bupivacaine as a mixture dilutes Fentanyl and receptor occupancy might decrease leading to less pronounced effect. And if Fentanyl is administered separately a greater spread and therefore formation of stronger bonds with the receptor leading to a denser and prolonged block may occur. This was supported by observations of Desai S et al., Gray JR et al., as they also found that duration of analgesia is increased when intrathecal morphine is administered with normal saline (hypobaric) than with dextrose saline (hyperbaric) [12,22]. Deshpande JP et al., and Thakur A et al., also reported that duration of analgesia is longer when clonidine is used sequentially than when it was given in mixture with hyperbaric Bupivacaine in other surgery like lower limb surgery and inguinal herniorrhaphy [23,24]. Result of this study also coincide with previous studies [17,20,21].
In this study, the incidence of itching, nausea/vomiting, respiratory depression, bradycardia were not statistically significant between the groups [Table/Fig-3,4]. The present results are in line with other studies [15,17,21].
In this study, 37.50% patients in group S labeled the effect as excellent and they would prefer this technique in future whereas 12.50% patients in group M labeled it as excellent. The difference in both the groups was found to be statistically significant (p<0.001) [Table/Fig-7]. In other studies VAS score was used [15,17,21].
The APGAR score in this study were statistically comparable in both groups and similar to other studies [15,17,21].
Limitation(s)
The temperature and rate of the injected drug was not recorded as it affects the spread of drugs.
Conclusion(s)
Two syringe techniques of fentanyl and hyperbaric bupivacaine provide significant improvement in the quality of sensory block without incidence of hypotension and provide prolonged post-operative analgesia as compared to one syringe technique.
†SD: Standard Deviation; *ASA: American society of anaesthesiologist
†SD: Standard Deviation; *ASA: American society of anaesthesiologist; level of significance at p<0.05