Thyrotoxic periodic paralysis is not uncommon in people of Asian origin. It presents as sudden onset paralysis resulting from hypokalemia due to intracellular shift of potassium because of thyroid hormone sensitive Sodium-Potassium ATPase. A 34-year-old male with history of weight loss, palpitation and increased sweating for three months presented with sudden onset weakness of both lower limbs, two hours post-dinner. On investigation, he was found to be having hypokalemia as well as thyrotoxicosis. His potassium was corrected and was put on non-selective beta blocker and carbimazole. The patient improved within 24 hours and was discharged with advice to continue with Inderal and Carbimazole and report after one month. Hyperthyroidism should be included in differential diagnosis of sudden onset lower limb weakness.
Beta blocker, Carbimazole, Hyperthyroidism, Hypokalemia
Case Report
A 34-year-old male presented to Accident and Emergency ward with complaints of inability to stand since two hours post-dinner the same night. He was watching television after taking his evening meal at about 8 PM. Around 9.30 PM while trying to get up his knees buckled and he fell onto the floor and was unable to stand. His pulse was noted to be 130/minute, blood pressure-160/90 mm Hg, temperature- 98.4° Fahrenheit. He was also noticed to be excessively sweating. The patient was conscious, speech was relevant and coherent. Orientation to time, place and person was normal and other higher functions were normal. Eye examination revealed retraction of upper eye lids. Muscle power was recorded to be 2/5 in both the lower limbs around all joints. Both knee and ankle jerks were depressed. Thyroid gland examination showed it to be enlarged, soft, non-tender, moving with deglutition. A bruit was heard on auscultation.
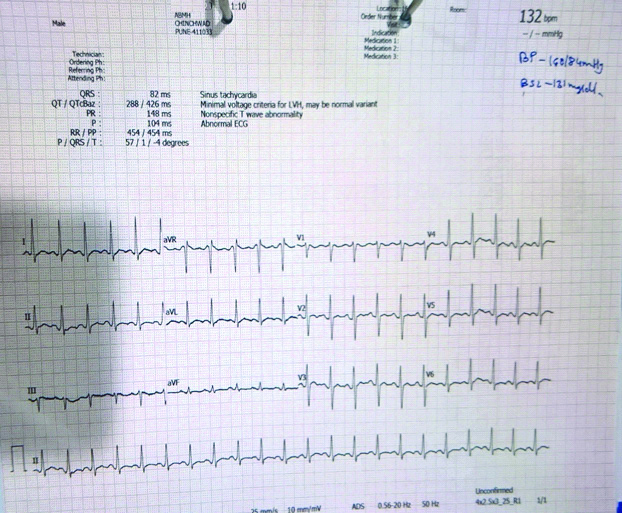
Examination of other systems was found to be non-contributory. Patient had history of increased perspiration, palpitations, weight loss of about six kilograms in past three months and shaking of hands and fingers. Electrocardiogram showed sinus tachycardia with rate 132/minute, rythm normal, T wave was found to be flattened and U wave was noted in limb and chest leads [Table/Fig-1]. His laboratory parameters were: Serum potassium-2.87 mEq/L (range 3.5-5 mEq/L), T3-10 nanomol/L (range 1.2-3.1), T4-280 nanomol/L (range 66-181), TSH-<0.05 microiu/mL (range 0.27-5.92) and anti-TPO was 0.22 units/mL (range 0-5.61).
Twelve lead Electrocardiogram showing sinus tachycardia with flattened T wave and presence of U wave noted in standard, aVL and chest leads.
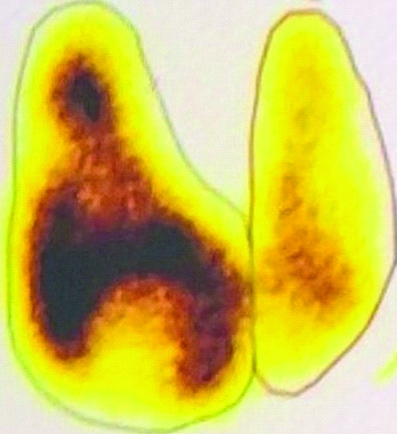
Ultrasound of thyroid showed enlarged thyroid, hypokalemia, nodular with a small cyst in left upper lobe. Doppler revealed increased vascularity and peak systolic velocity of inferior thyroid artery was 53 cm/second. Thyroid uptake study with 99 m Technetium was 27%. The scan revealed increased focal uptake in right upper and lower lobe; a cold nodule in left upper lobe and decreased uptake in lower lobe [Table/Fig-2].
A 99mTechnetium uptake shows increased and heterogenous uptake in right upper and lower lobe. Left upper lobe reveals almost no uptake and left lower lobe showing decreased uptake.
The clinical features, presence of goiter, bruit, hypokalaemia, thyroid function test, lower limb paralysis with depressed reflexes suggested the diagnosis of Thyrotoxicosis with hyperthyroidism and Thyroid periodic paralysis.
Patient was given about 60 milli equivalent of potassium chloride over eight hours. Next day morning, his weakness improved, muscle power returned to grade 5/5 around all joints and he was able to stand on his own. The patient was put on Carbimazole 30 mg/day along with 40 mg of Inderal daily.
He was discharged after one day and was advised to continue the medicines. During the treatment with anti-thyroid drugs paralysis did not recur. In three months time, patient had become euthyroid both clinically and biochemically. He underwent total thyroidectomy successfully.
Total thyroidectomy was done in view of the presence of cold nodules. Post-thyroidectomy patient was put on 100 micro gram of thyroxine. After two months, post-thyroidectomy the patient was maintaining well and there was no recurrence of paralysis.
Discussion
Thyrotoxic periodic paralysis is regularly reported from people of Asian origin. People of Indian, Chinese, Japanese ethnicity present with sudden onset weakness of the limbs mostly in the morning hours after heavy carbohydrate meal or exercise. Most of them are middle aged and males [1,2]. Many do not have prior history suggestive of Thyrotoxicosis.
Sudden onset paralysis brings many differential diagnosis into consideration [3]:
(a) Familial hypokalemic periodic paralysis: There would be a positive family history, age less than 16 years in 80% of cases, precipitation of attack after heavy carbohydrate meal or exercise. Tendon reflexes will be depressed or absent. Rare involvement of respiratory muscles. Facial muscles will not be involved.
(b) Acute inflammatory demyelinating polyneuropathy: No age limit, weakness and paralysis with ascending progression, no family history, usually preceded by infection, reflexes depressed or absent with dysautonomia, risk of severe respiratory muscle involvement and involvement of facial muscles most importantly potassium level will be normal.
(c) Thyrotoxic proximal myopathy: Duration rather than severity of thyrotoxic state is important, no family history, no age bar, no hypokalemia, deep tendon reflexes normal or brisk.
The index patient recovered from thyroid periodic paralysis within 4-6 hours after correction of potassium. Treatment with non-selective Beta blocker and Carbimazole was also required for full recovery and to prevent recurrence of hypokalemic paralysis followed later on by total thyroidectomy in view of cold nodules. The prevalence of malignancy varies from 9-32.8% as per some reports [3-5]. There is fairly strong evidence of genetic mutation of Potassium inward rectifying channel (Kir 2.6) in the pathogenesis of thyroid periodic paralysis. Loss of function of Kir 2.6 along with enhanced Catecholamine activity in thyrotoxicisis leads to increased activity of Sodium-Potassium ATPase (Na+K+ATPase) resulting in hypokalemic paralysis [6].
Thyrotoxic periodic paralysis is a rare disease in western countries [7]. First case was reported by Rossenfield M [8]. Since then, many cases of thyrotoxic periodic paralysis have been reported mostly from Asians such as Chinese, Japanese, and people of Indian origin [9]. There has been no large scale studies in India, so it is presently not known as to what is the approximate percentage of thyrotoxic patients developing thyrotoxic periodic hypokalemic paralysis, although the reports of cases trickle in.
Chang C-C et al., reported 135 cases of thyrotoxic periodic paralysis over 10-year period recorded at an academic centre. There was a huge difference of 130:1 (male to female) in this series. Most of the cases were in age range of 16-62 (mean 30.6±8.2) [10]. Glucose induced hypokalemia (mean 2.47±0.6 mmol/L) was identified in only 34% of patients. There was no personal or family history of hyperthyroidism.
Darrow M et al., studied two cases of Japanese origin presenting with thyrotoxic hypokalemic periodic paralysis with normal sinus rhythm [11] in contrast to the index case presenting with sinus tachycardia, a hall mark of Thyrotoxicosis. Goldberger ZD suggested resting sinus tachycardia in the presence of hypokalemia to be a valuable key to the diagnosis of thyrotoxic perodic paralysis even before investigations for thyrotoxicosis [12].
Kalita J et al., in the series of 52 patients with hypokalemic periodic paralysis 17.3% of their cases were diagnosed as thyrotoxic periodic paralysis. Two of the cases had bulbar paralysis and another two had respiratory muscle weakness. Thyrotoxic periodic paralysis patients, the paralysis was precipitated by heavy carbohydrate meal and febrile illness [13]. The index patient did not give history of high carbohydrate meal, exercise or fever. He developed weakness about two hours after last meal.
Rolim ALR et al., described the most common causes of thyrotoxic periodic paralysis as well as Familial hypokalemic Periodic Paralysis (FPP) to be endocrine channelopathy [14]. There have been irrefutable evidence showing the role of genetic mutations in Kir 2.6 channel in the pathogenesis of thyroid periodic paralysis. Loss of function mutation of Kir 2.6 along with increased activity of Sodium-Potassium ATPase with catecholamines enhancing it, resulting in hypokalemia. Kung AWC opined that assessment of thyroid function test in patients presenting with hypokalemia and muscle weakness serves to differentiate thyroid periodic paralysis with other forms of hypokalemic periodic paralysis [15]. Immediate supplementation with potassium chloride is warranted. The dose may vary from 40-200 milli mol. When the patient recovers there is no further requirement of potassium for prophylaxis. Mainstay of therapy later on is good control of hyperthyroidism. Similar management with potassium chloride, non-selective beta-blockers and definitive treatment of underlying hyperthyroidism is advocated by others [16].
Conclusion(s)
Thyroid periodic paralysis may present with hypokalemia, lower limb paralysis at the initial presentation. History, clinical features, goiter, eye signs, if present and tachycardia helps in differential diagnosis. Thyroid hormone estimation and Technetium uptake study confirms the diagnosis. Thyroid periodic paralysis should always be considered while evaluating hypokalemic paralysis.
[1]. Vijayakumar A, Ashwath G, Thimmappa D, Thyrotoxic periodic paralysis: Clinical challengesJournal of Thyroid Research 2014 2014:64950210.1155/2014/64950224695373 [Google Scholar] [CrossRef] [PubMed]
[2]. Saroja AO, Naik KR, Khanpet MS, Uncommon dyselectrolytemia complicating Guillain-Barré syndromeJ Neurosci Rural Pract 2013 4(3):328-30.10.4103/0976-3147.11879424250175 [Google Scholar] [CrossRef] [PubMed]
[3]. Cerci C, Cerci SS, Eroglu E, Dede M, Kapucuoglu N, Yildiz M, Thyroid cancer in toxic and non-toxic multinodular goiterJ Postgrad Med 2007 53(3):157-60.10.4103/0022-3859.3385517699987 [Google Scholar] [CrossRef] [PubMed]
[4]. Kunjumohamed FP, Al-Busaidi NB, Al-Musalhi HN, Al-Shereiqi SZ, Al-Salmi IS, The prevalence of thyroid cancer in patients with hyperthyroidismSaudi Med J [Internet] 2015 36(7):874-77.10.15537/smj.2015.7.1146326108596 [Google Scholar] [CrossRef] [PubMed]
[5]. Al-Wattar WM, Incidence of thyroid cancer in long standing multinodular goiter: Prospective studyJ Res Med Dent Sci 2018 6(5):6 [Google Scholar]
[6]. Goh SH, Thyrotoxic periodic paralysis: Reports of seven patients presenting with weakness in an Asian emergency departmentEmerg Med J [Internet] 2002 19(1):78-79.10.1136/emj.19.1.7811777887 [Google Scholar] [CrossRef] [PubMed]
[7]. Patil MM, Kamalanathan S, Das AK, Sahoo J, Thyrotoxicosis with periodic paralysisInt J Clin Exp Physiol 2014 1(1):310.4103/2348-8093.129750 [Google Scholar] [CrossRef]
[8]. Rossenfield M, Akute aufsteigende Lahmung bei Morbus BasedowBerl Klin Wochnschr 1902 39:538 [Google Scholar]
[9]. Sharma ZD, Gokhale VS, Chaudhari N, Kakrani AL, Thyrotoxicosis presenting first time as hypokalemic paralysisThyroid Res Pract 2013 10(3):11410.4103/0973-0354.116132 [Google Scholar] [CrossRef]
[10]. Chang CC, Cheng CJ, Sung CC, Chiueh TS, Lee CH, Chau T, A 10-year analysis of thyrotoxic periodic paralysis in 135 patients: Focus on symptomatology and precipitantsEur J Endocrinol [Internet] 2013 169(5):52910.1530/EJE-13-038123939916 [Google Scholar] [CrossRef] [PubMed]
[11]. Darrow M, Brammer WK, Rowley A, Thyrotoxic periodic paralysis: Two case studiesArch Phys Med Rehabil 1995 76(7):685-87.10.1016/S0003-9993(95)80641-5 [Google Scholar] [CrossRef]
[12]. Goldberger ZD, An electrocardiogram triad in thyrotoxic hypokalemic periodic paralysisCirculation 2007 115:e179-80.10.1161/CIRCULATIONAHA.106.65239617296862 [Google Scholar] [CrossRef] [PubMed]
[13]. Kalita J, Goyal G, Bhoi SK, Chandra S, Misra UK, Comparative study of thyrotoxic periodic paralysis from idiopathic hypokalemic periodic paralysis: An experience from IndiaAnn Indian Acad Neurol [Internet] 2012 15(3):18610.4103/0972-2327.9970822919190 [Google Scholar] [CrossRef] [PubMed]
[14]. Rolim ALR, Silva MRD da, Thyrotoxic periodic paralysis- Clinical diagnosis and managementThyroid Disorders-Focus Hyperthyroidism [Internet] 2014 ch.610.5772/58475 [Google Scholar] [CrossRef]
[15]. Kung AWC, Thyrotoxic periodic paralysis: A diagnostic challengeJ Clin Endocrinol Metab 2006 91(7):2490-95.10.1210/jc.2006-035616608889 [Google Scholar] [CrossRef] [PubMed]
[16]. Salih M, Duschek EJJ, Thyrotoxic periodic paralysis: An unusual presentation of hyperthyroidismNeth J Med 2017 75(8):6 [Google Scholar]