Facial, Skeletal and Radiological Features of Larsen Syndrome: A Case Report
Ravishankar Pillenahalli Maheshwarappa1, Juhi Bansal2
1 Resident, Department of Radiology, University of Iowa Hospitals and Clinics, Iowa City, Iowa, USA.
2 Former Senior Resident, Department of Radiology, Adichunchanagiri Institute of Medical Sciences, Mandya, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ravishankar Pillenahalli Maheshwarappa, 200 Hawkins Drive, Iowa City, USA.
E-mail: ravi_spm@yahoo.co.in
Larsen syndrome is a rare congenital osteochondrodysplasia resulting in multiple joint dislocations and typical facial features. The inheritance pattern can be autosomal dominant or recessive, with the recessive pattern being more severe. This condition requires prolonged orthopaedic treatment and achievement of complete normal function is unlikely. The author hereby present a case report of three-year-old female child with this syndrome which was diagnosed by clinical examination and radiological findings.
Congenital, Multiple joint dislocations, Ostochondrodysplasia
Case Report
A three-year-old female child was referred to the Radiology department for Ultrasound (USG) Abdomen with complaints of constipation for the past six months. There was no history of fever, rash, vomiting or breathing difficulties. The abdominal scan did not reveal any significant abnormality. The child’s father also expressed concern about the inability of the child to walk since childhood. On further questioning, it was found that the elder brother of his child (10-year-old) also had short stature, however with limited disability. The children were from a non-consanguineous marriage and no significant peripartum history was found.
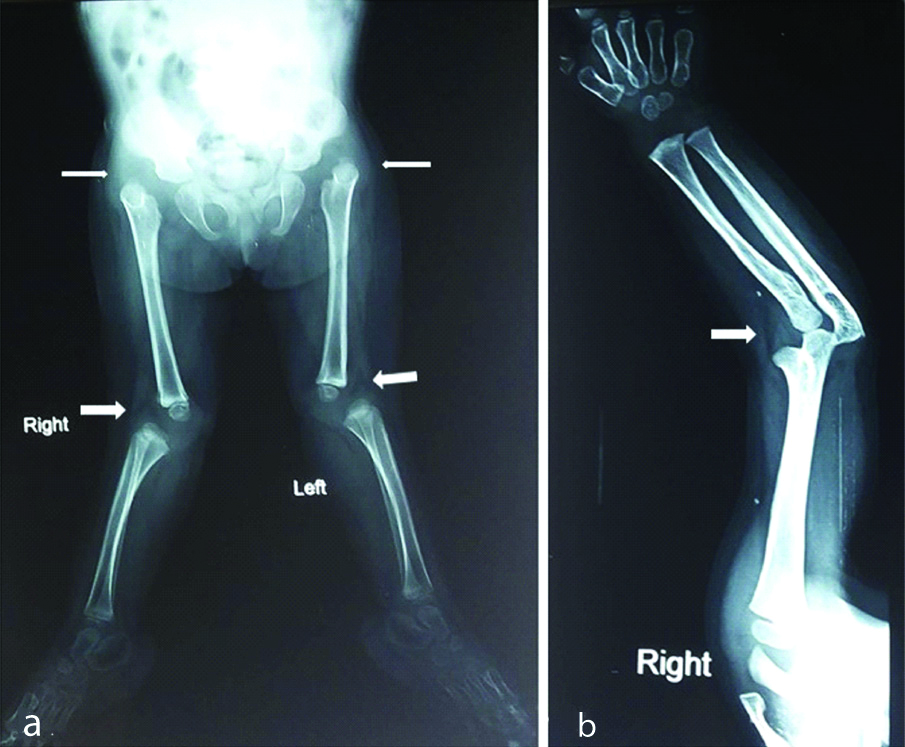
This child was found to have abnormally hyperextended knee joints along with abnormal elbow and hip joint; the patient had a slightly flattened nasal bridge [Table/Fig-1]. After radiography, it was found that child had bilateral dislocated knee, hip and elbow joints [Table/Fig-2]. The genetic testing for Filamin B, beta (FLNB) gene mutation could not be done as it was unavailable at the center. The patient was referred to orthopaedics department for further management where the dislocated joints were first managed by traction followed later by corrective surgery. On long-term follow-up, the patient was found to respond well.
Photograph of child showing depressed nasal bridge and typical facies. Dislocation of bilateral knee joints resulting in genu valgus deformity.

a) X-ray of pelvis and bilateral lower extremities. There is dislocation of bilateral hip joints (thin white arrows) and knee joints (thick white arrows); b) X-ray of the right arm reveals dislocation of the elbow joint (white arrow).
Discussion
Larsen syndrome occurs in approx. 1 in 100,000 babies in the Western population [1]. The disease has an equal incidence in males and females. It can be inherited as either autosomal dominant or recessive form. The classic form of Larsen syndrome is caused by a mutation in the FLNB gene located on chromosome 3p14 and is inherited as an autosomal dominant form [2,3]. This gene has a role in the production of filamin B which plays a very important role in the development of skeletal system and connective tissues. The symptomatology in children with Larsen syndrome varies greatly from individual to individual even within the same family [3-6].
The typical features of the condition are multiple joint dislocations most commonly involving the hip, knee and elbow joints. Other skeletal manifestations include patellar dislocation, club foot, subluxation of the shoulder joints, short and broad fingers, supernumerary carpal and tarsal bones. The characteristic facial features include widely separated eyes, forehead prominence, depressed nasal bridge and flat mid facies. They generally are short in stature due to the scoliosis and cervical kyphosis [6]. In present case child had hypertelorism, flat mid facies, dislocation of bilateral hip, knee and elbow joints, inability to walk since childhood.
Other uncommon features present in children with Larsen syndrome include conductive and/or sensory neural hearing loss, eye diseases such as recurrent keratitis, cataract and congenital glaucoma, recurrent respiratory infections, cleft palate, oropharyngeal malformations, complete agenesis of anus and bifid uterus. Learning disabilities, developmental delay, life-threatening respiratory (breathing) abnormalities and cardiac malformations have also been described in a few patients [6-11].
The disease is usually identified on the basis of clinical findings. The radiographic examination is highly diagnostic. Radiographs disclose under-mineralisation and over-tubulation of the long bones, a bifid calcaneus and highly developed bone age in the carpal or extra carpal bones. Scoliosis, coronal clefts of the vertebrae and subluxation of the vertebrae may be observed [12,13]. Present case had typical multiple joint dislocations and family history of similar presentation in the elder sibling. Few typical and atypical presentations of Larsen syndrome reported in the literature are tabulated in [Table/Fig-3] [1,6,9-11,14-18].
Few typical and atypical presentations of Larsen syndrome described in the literature [1, 6, 9-11, 14-18].
| Author Name and Year | Salient clinical features | Radiological findings | Treatment |
|---|
| Chien M et al., 1995 [14] | Bilateral equinovarus, subluxation of the knees, dislocation of the radial heads, and thoracolumbar scoliosis. Flattened face, depressed nasal bridge, exophthalmos, hypertelorism, periodontitis. | Full mouth radiograph showed alveolar bone loss, Supra- and subgingival calculus. | Multiple orthopaedic surgeries and castings to correct deformities. |
| Roopesh Kumar VR et al., 2013 [15] | Claw-like deformity of both hands, frontal bossing, hypertelorism, widened nasal bridge, mild spasticity of all limbs, gibbous deformity at the thoracolumbar junction. | Radiograph of the cervical spine: Gross kyphotic deformity at C2-C3, atlantoaxial dislocation.Magnetic resonance image and computed tomographic scan: Spondyloptosis of C3 over C4; the spinal cord compression by atlantoaxial dislocation and posteriorly displaced C3 vertebral body, D12-L1 fusion with kyphotic deformity. | Corrective surgery in the cervical spine to relieve spinal cord compression. |
| Sajnani AK et al., 2010 [6] | Short stature, hip and knee dislocations, spinal abnormalities, myopia, facial abnormalities including prominent forehead, hypertelorism, flat mid facies, depressed nasal bridge, dental abnormalities. | Radiograph showing mid-face deficiency. Orthopantomogram revealed left permanent lateral incisor and the right mandibular second premolar and generalised alveolar bone loss. | Myopia corrective surgeries. Multiple orthopaedic corrective surgeries and castings. |
| Marques LHS et al., 2017 [10] | Progressive bilateral hearing loss, hypertelorism, flat facies, multiple lower limb deformities. | CT of the temporal bone showed irregular malleus, short process of the incus and incudo-malleolar joints. | Lower limb deformities treated with multiple corrective surgeries. Hearing loss treated with hearing aids. |
| Madera M et al., 2008 [16] | Subglottic stenosis, cervical kyphosis, bilateral skew foot deformities. | Radiography showed worsening cervical kyphosis and instability of the congenital cervical kyphosis. MRI and CT showed thecal sac compression by cervical scoliosis. | Corrective surgery for cervical kyphosis. Capsulotomy for bilateral skew foot deformities. Rigid cervical collar for cervical kyphosis. |
| Je BK et al., 2006 [17] | Saccular aneurysm of the descending aorta along with other typical features of Larsen syndrome including multiple joint dislocations, foot equinovarus deformity, frontal bossing, depressed nasal bridge, hypertelorism, bluish sclera, left exotropia and sagittal synostosis. | Radiograph showing bilateral knee dislocation. CT scan showed aneurysm of descending thoracic aorta. | Aneurysm was clamped and the aneurysm neck closed by a Hemashield patch. Corrective surgeries for orthopaedic deformities. |
| Jain VV et al., 2014 [11] | Dural ectasia, cervicothoracic kyphosis with anterior subluxation of C6 over C7 and C7 over T1, polycystic kidney disease. Other typical orofacial abnormalities of Larsen were also noted. | Radiographs showing kyphotic deformity. MRI spine showed dural ectasia. | Surgical stabilisation of the spine rigid cervical collar. Previous surgeries include cleft palate repair and polydactyly removal (thumb), bilateral knee quadriceps plasty, and bilateral herniorrhaphies. |
| Nash R et al., 2012 [9] | Bilateral hearing loss, narrow ear canal, congenital right-sided hip and knee dislocations. No facial dysmorphia. | CT scan showed maloriented stapes on the oval window. | Conservative management for hearing loss. |
| Liang CD and Hang CL 2001 [1] | Multiple cardiac abnormalities small patent ductus arteriosus, a small atrial septal defect of the secundum type, bicuspid aortic valve. Dilated aortic sinuses, mild subaortic stenosis, and mitral valve prolapse with mitral regurgitation, elongated aorta. Other typical facial and skeletal abnormalities of Larsen were also noted. | Aortography showed elongated aorta. Echocardiography revealed multiple cardiac anomalies. | Conservative management for cardiac anomalies. Orthopaedic abnormalities treated with serial castings and open knee reduction. |
| Kodra N et al., 2019 [18] | Cleft palate, flat mid facies, hypertelorism, creases under the eyes, a small nose with anteverted nares, arachnodactyly of fingers and toes, laterally deviated great toes, and mild pectus carinatum. Hallmark finding of absence of joint dislocation. | Not described. | Not mentioned. |
| Present case report (2020) | Hyperextended knee joints along with abnormal elbow and hip joint. Patient had a slightly flattened nasal bridge, hypertelorism, flat mid facies. | Dislocation of bilateral hip joints and knee joints. X-ray of the right arm reveals dislocation of the elbow joint. | Dislocated joints were first managed by traction followed later by corrective surgery. |
CT- Computed tomography
The condition is usually managed by multidisciplinary approach requiring orthopaedic treatment, surgical procedures and physiotherapy. These patients should undergo annual orthopaedic screening to evaluate the progressive scoliosis. Genetic counseling should be offered to the patients with this condition. They should be informed that there is a 50% risk of referring the mutation to the offspring [1,9,18].
Conclusion(s)
Larsen syndrome is a genetic disorder characterised by multiple joint dislocations and typical fascial features. Early diagnosis and treatment are crucial in limiting the functional disability of the patients. Careful evaluation of the family members for the presence of this disorder plays an important role in reducing the healthcare burden on the family.
CT- Computed tomography
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Mar 30, 2020
Manual Googling: Jun 19, 2020
iThenticate Software: Jul 28, 2020 (14%)
[1]. Liang CD, Hang CL, Elongation of the aorta and multiple cardiovascular abnormalities associated with larsen syndromePaediatr Cardiol 2001 22(3):245-46.10.1007/s00246001021311343154 [Google Scholar] [CrossRef] [PubMed]
[2]. Krakow D, Robertson SP, King LM, Morgan T, Sebald ET, Bertolotto C, Mutations in the gene encoding filamin B disrupt vertebral segmentation, joint formation and skeletogenesisNat Genet 2004 36(4):405-10.10.1038/ng131914991055 [Google Scholar] [CrossRef] [PubMed]
[3]. Vujic M, Hallstensson K, Wahlström J, Lundberg A, Langmaack C, Martinson T, Localization of a gene for autosomal dominant Larsen syndrome to chromosome region 3p21.1-14.1 in the proximity of, but distinct from, the COL7A1 locusAm J Hum Genet 1995 57(5):1104-13. [Google Scholar]
[4]. Kiel EA, Frias JL, Victorica BE, Cardiovascular manifestations in the Larsen syndromePaediatrics 1983 71(6):942-46. [Google Scholar]
[5]. Johnston CE 2nd, Birch JG, Daniels JL, Cervical kyphosis in patients who have Larsen syndromeJ Bone Joint Surg Am 1996 78(4):538-45.10.2106/00004623-199604000-000078609132 [Google Scholar] [CrossRef] [PubMed]
[6]. Sajnani AK, Yiu CKY, King NM, Larsen syndrome: A review of the literature and case reportSpec Care Dentist 2010 30(6):255-60.10.1111/j.1754-4505.2010.00163.x21044106 [Google Scholar] [CrossRef] [PubMed]
[7]. Mitra N, Kannan DN, Kumar V, Kavita G, Larsen syndrome: A case reportJournal of Nepal Paediatric Society 2012 32(1):85-87.10.3126/jnps.v32i1.5349 [Google Scholar] [CrossRef]
[8]. Ott IO, Issing PR, Bilateral, mixed hearing loss with a predominant sensorineural component in Larsen’s syndromeJ Laryngol Otol 2008 122(3):e610.1017/S002221510700146618279569 [Google Scholar] [CrossRef] [PubMed]
[9]. Nash R, Majithia A, Ujam A, Singh A, Ossicular malposition in Larsen syndrome: A case reportJ Surg Case Rep 2012 2012(11):rjs00710.1093/jscr/rjs00724968394 [Google Scholar] [CrossRef] [PubMed]
[10]. Marques LHS, Martins DV, Juares GL, Lorenzetti FTM, Monsanto RDC, Otologic manifestations of Larsen syndromeInt J Paediatr Otorhinolaryngol 2017 101:223-29.10.1016/j.ijporl.2017.08.02028964299 [Google Scholar] [CrossRef] [PubMed]
[11]. Jain VV, Anadio JM, Chan G, Sturm PF, Crawford AH, Dural ectasia in a child with Larsen syndromeJ Paediatr Orthop 2014 34(7):e44-49.10.1097/BPO.000000000000018624674893 [Google Scholar] [CrossRef] [PubMed]
[12]. Al-Kaissi A, Ammar C, Ben Ghachem MB, Hammou A, Chehida FB, Facial features and skeletal abnormalities in Larsen syndrome-A study of three generations of a Tunisian familySwiss Med Wkly 2003 133(45-46):625-28. [Google Scholar]
[13]. Klein C, Bulaid Y, Deroussen F, Plancq MC, Printemps C, Gouron R, Congenital dislocation of the knee in a three-year-old-child with Larsen syndrome: Treatment with a hexapod-type external fixatorThe Knee 2018 25(5):966-71.10.1016/j.knee.2018.07.00630111500 [Google Scholar] [CrossRef] [PubMed]
[14]. Chien M, Punwani I, Watanabe K, Advanced periodontitis associated with Larsen’s syndrome: Case reportPaediatr Dent 1995 17(1):62-64. [Google Scholar]
[15]. Roopesh Kumar VR, Madhguiri VS, Sasidharan GM, Gundamaneni SK, Yadav AK, Larsen syndrome with C3-C4 spondyloptosis and atlantoaxial dislocation in an adultSpine (Phila Pa 1976) 2013 38(1):E43-47.10.1097/BRS.0b013e318278e59d23080426 [Google Scholar] [CrossRef] [PubMed]
[16]. Madera M, Crawford A, Mangano FT, Management of severe cervical kyphosis in a patient with Larsen syndrome. Case reportJ Neurosurg Paediatr 2008 1(4):320-24.10.3171/PED/2008/1/4/32018377309 [Google Scholar] [CrossRef] [PubMed]
[17]. Je BK, Yoo SY, Lee W, Kim WS, Kim IO, Aneurysm of the ductus arteriosus in a patient with Larsen syndromePaediatr Radiol 2006 36(11):1215-18.10.1007/s00247-006-0316-x17006654 [Google Scholar] [CrossRef] [PubMed]
[18]. Kodra N, Diamonstein C, Hauser NS, A case study of atypical Larsen syndrome with absent hallmark joint dislocationsMol Genet Genomic Med 2019 7(5):e648-e.10.1002/mgg3.64830916490 [Google Scholar] [CrossRef] [PubMed]