Lymphadenopathy suggests enlargement of the lymph node and lymphadenitis suggests inflammation of the lymph node [1]. Lymph nodes are widely distributed and forms easily accessible component of lymphoid tissue. They are the commonest aspirated organs for diagnostic purpose [2]. Lymphadenopathy may be an incidental finding or it may be a primary or secondary manifestation of underlying neoplastic or non-neoplastic disease [3]. The spectrum of lesions may include inflammatory, infectious, autoimmune or malignant aetiology [1]. FNAC is a diagnostic technique employed to collect cells, tissues and/or fluid by aspiration using a thin needle attached with disposable syringe for the purpose of diagnosis of masses. It is an easy, simple and rapid diagnostic technique. Because of early availability of results with minimal trauma, complication or discomfort, the aspiration cytology is now considered as a valuable diagnostic technique [4]. Majority of the studies have emphasised on the cytomorphological pattern of lymph node lesions exclusively, either in the paediatric population or in the adult population. Only few studies have focused on comparing the cytomorphological pattern of the lymph node lesions between the paediatric population and the adult population. Hence, the current study was undertaken to compare the cytomorphological patterns of the lymph node lesions in paediatric population with that of adult population and to correlate with available histopathological diagnosis.
Materials and Methods
It was a retrospective observational study conducted in the Department of Pathology from January 2017 to June 2018 for a period of 18 months at a rural tertiary care referral institute, PESIMSR, Kuppam, Andhra Pradesh, India. Ethical clearance was obtained from the Institutional Ethics Committee bearing number PESIMSR/IHEC/12. The sample size was calculated using the following formula:
“n” is the sample size
“z2(1-α/2)” is the level of significance at 5% that is 95% confidence interval
“p” is the expected proportion of cytology samples
“d” is the desired error of margin
Two hundred and seventy four cases were analysed. All the patients presenting with peripheral lymphadenopathy requiring cytopathological evaluation (FNAC) were included in the study. Those cases in which cytology smears were inadequate for interpretation were excluded from the study.
With informed consent, FNAC was performed as per the standard operating procedure. Aspirates were deposited onto the slides. Subsequently alcohol fixed, air-dried and heat fixed smears were made. Alcohol fixed smears were stained routinely by Haematoxylin and Eosin (H&E) and Papanicolaou (PAP) method. Air-dried smears were stained by May Grunwald Giemsa (MGG) stain. Air-dried and heat fixed smears were stained by Ziehl-Neelson (ZN) stain for Acid-Fast Bacilli (AFB). Periodic Acid Schiff (PAS) staining was employed in selected cases for cytological evaluation. Various lesions were documented and categorised according to age, sex and site. Cytomorphological patterns of lymph node lesions were compared between paediatric and adult age group patients and analysed. Cytological diagnosis was compared with available histopathological diagnosis and concordance was calculated.
Statistical Analysis
Frequencies, Chi-square test and crosstabs were used for calculation. Cytological diagnosis was compared with histopathological diagnosis and the diagnostic efficacy of FNAC was evaluated. All statistical calculations were done through statistical software STATA version 13.
Results
A total of 274 cases were analysed, which included adults {225 cases (82.11%)} and paediatric age group {49 cases (17.88%)}. The age of the patients ranged from 6 months to 12 years in paediatric population and 13 to 80 years in adult population. The lesions were most common in 7-9 years in paediatric age group (mean=6.5). The lesions were most common in 3rd decade in adult age group (mean=38.12). In paediatric age group, males were predominantly affected constituting 33 cases (67.3%) with M:F ratio of 2.06:1. In adults, females were predominantly affected constituting 117 cases (52%) with M:F ratio of 0.92:1.
Cervical lymph node was the common site of involvement in both paediatric {47 cases (95.91%)} and adult age group {186 cases (82.66%)}. The other sites of involvement in the paediatric age group were axillary lymph node {one case (2.04%)} and inguinal lymph node {one case (2.04%)}. The other sites of involvement in the adult population were inguinal lymph nodes {20 case (8.88%)}, axillary lymph nodes {18 cases (8%)} and paraaortic lymph node {one case (0.44%)}. The laterality varied between both the populations. Right sided lymph nodes {25 cases (51.02%)} were commonly affected in paediatric age group. Left sided lymph nodes {112 cases (49.77%)} were predominantly involved in adult population.
Reactive lymphadenitis was the commonest pattern observed in both the paediatric age group and in adult population. Chronic lymphoproliferative lesions and tuberculous lymphadenitis constituted the least common lesions in the adults and the paediatric population respectively. Malignant cases, tubercular lymphadenitis, chronic granulomatous lymphadenitis were more common in adults compared to the paediatric population. Statistically, the values were highly significant (p<0.001) [Table/Fig-1]. Reactive lymphadenitis was diagnosed when the smear showed polymorphous population of lymphoid cells (composed of centroblasts, centrocytes and mature lymphocytes admixed with tingible body macrophages, plasma cells and immunoblasts). Chronic granulomatous lymphadenitis was diagnosed when the smear showed Epithelioid Cell Granulomas (ECG) and smear for Acid Fast Bacilli were negative.
Distribution of lymph node lesions among paediatric and adult population.
| Category | Paediatric cases (n=49) | Adults (n=225) | Total cases (n=274) | p-value* |
|---|
| Reactive lymphadenitis | 33 (67.35%) | 73 (32.44%) | 106 (38.69%) | p<0.001 |
| Chronic granulomatous lymphadenitis | 5 (10.20%) | 52 (23.11%) | 57 (20.80%) |
| Malignancy | 0 | 37 (16.44%) | 37 (13.5%) |
| Primary | | 7 (3.11%) | |
| Non-Hodgkins lymphoma | - | 6 (2.67%) | |
| Hodgkins lymphoma | - | 1 (0.44%) | |
| Secondary | - | 30 (13.33%) | |
| Poorly differentiated carcinoma | - | 21 (9.33%) | |
| Squamous cell carcinoma | - | 8 (3.56%) | |
| Adenocarcinoma | - | 1 (0.44%) | |
| Mycobacterial lymphadenitis | 1 (2.04%) | 34 (15.11%) | 35 (12.77) |
| Caseous necrosis | 1 (2.04%) | 12 (5.33%) | |
| Epithelioid cell granuloma | - | 3 (1.33%) | |
| Caseous necrosis with epithelioid cell granuloma | - | 8 (3.56%) | |
| No caseous necrosis No granulomas | - | 11 (4.89%) | |
| Acute suppurative lesions | 6 (12.24%) | 18 (8%) | 24 (8.76%) |
| Necrotising lymphadenitis | 2 (4.08%) | 7 (3.11%) | 9 (3.28%) |
| Chronic Lymphoproliferative Lesion | 2 (4.08%) | 4 (1.78%) | 6 (2.19%) |
| Total | 49 (17.88%) | 225 (82.12%) | 274 |
*Chi-square test was the statistical tool used to perform statistical analysis
Mycobacterial lymphadenitis was diagnosed when the smear for Acid Fast Bacilli was positive. Among 35 cases of mycobacterial lymphadenitis, the cytomorphological patterns were categorised into four patterns. The patterns included Caseous Necrosis (CN) (Smears showing only CN); Epithelioid Cell Granuloma (ECG) (Smears showing only ECG), CN-ECG (Smears showing both CN and ECG) and NCNG (Smears showing neither CN nor ECG, but sattered epithelioid cells/macrophages/neutrophils may be seen). Most predominant pattern was CN constituting 13 cases (37.14%) followed by neither CN nor ECG (NCNG) constituting 11 cases (31.43%), presence of both CN and ECG (CN-ECG) constituting eight cases (22.8%) and ECG in three cases (8.57%). NCNG category showed only epithelioid cells in seven cases (20%) and showed both neutrophils and macrophages in four cases (11.42%). AFB grading was done on ZN stained smears based on grading system given by Kumar et al., [5]. Cytomorphological patterns of mycobacterial lesions were correlated with AFB Grading [5]. Grade 2+ was the most common pattern. Grade 1+ was seen more common in only CN pattern. Grade 2+ was common in patterns with no CN and ECG. Only one case with Grade 3+ AFB was seen in only CN pattern. In paediatric cases, one case of mycobacterial lymphadenitis was reported with AFB Grade 2+ displaying a CN pattern. [Table/Fig-2] displays the cytomorphological pattern correlation with the AFB grading.
Correlation of cytomorphological pattern of mycobacterial lymphadenitis with AFB Grading.
| AFB grading | Cytomorphological pattern of mycobacterial lymphadenitis |
|---|
| CN | ECG | CN-ECG | NCNG | Total |
|---|
| Grade 1+ | 6 (75%) | - | - | 2 (25%) | 8 |
| Grade 2+ | 6 (23.08%) | 3 (11.54%) | 8 (30.77%) | 9 (34.62%) | 26 |
| Grade 3+ | 1 (100%) | - | - | - | 1 |
| Total | 13 | 3 | 8 | 11 | 35 |
CN- Smears showing only CN; ECG- Smears showing only ECG, CN-ECG- Smears showing both CN and ECG, NCNG- Smears showing neither CN nor ECG, but sattered epithelioid cells or neutrophils may be seen
Grade 1+=AFB was found after a careful search
Grade 2+=AFB were singly scattered
Grade 3+=AFB were found in large numbers arranged in faggots and singly
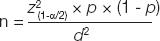
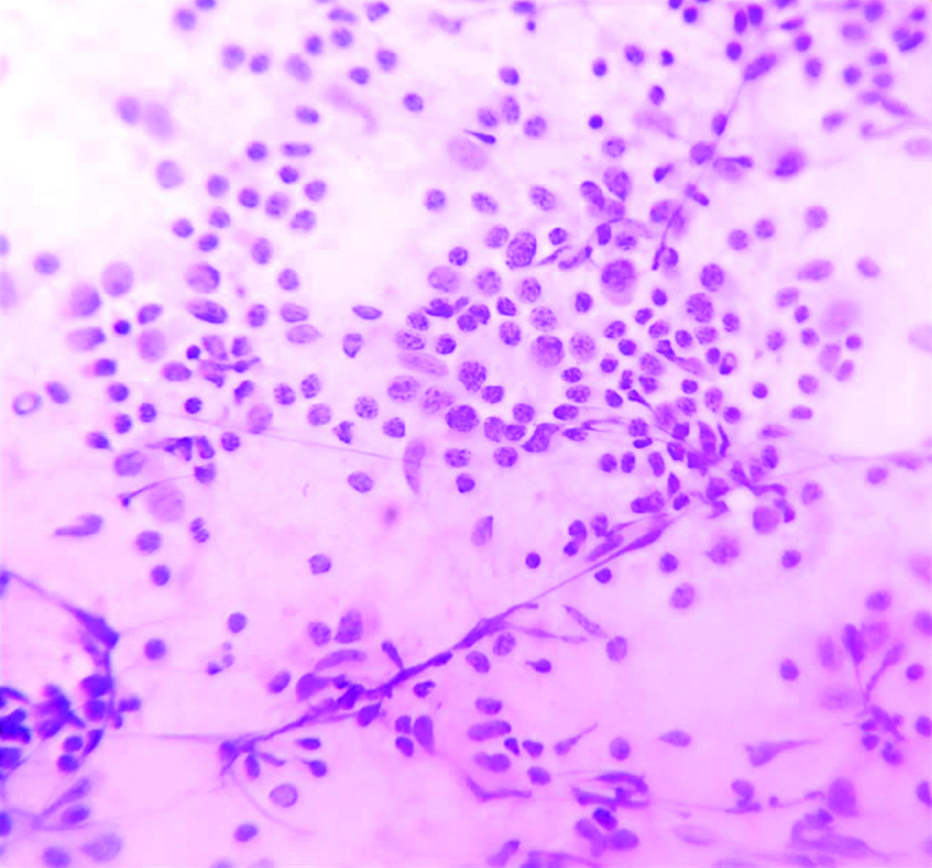
Acute suppurative lymphadenitis lesion was diagnosed when the smear showed abundant neutrophils admixed with few macrophages in a proteinaceous background [Table/Fig-3]. Necrotising lymphadenitis was diagnosed when the smear showed only necrosis and smear for Acid Fast Bacilli was negative. Chronic lymphoproliferative lesion was diagnosed when the smears were cellular and lymphoid population of cells were relatively monomorphic or bimodal and admixed with sparse tingible body macrophages and/or immunoblasts. The diagnosis was correlated with clinical presentation in each case [Table/Fig-4].
Microphotograph of cytology smears of acute suppurative lymphadenitis- displaying abundant neutrophils and few macrophages in a proteinaceous background (H&E, X400).

Microphotograph of cytology smear of lymphoproliferative lesion- displaying relatively monomorphic lymphoid cells in a proteinaceous background. Lymphoid cells show scant cytoplasm and round to oval nucleus with open chromatin (MGG, X400).
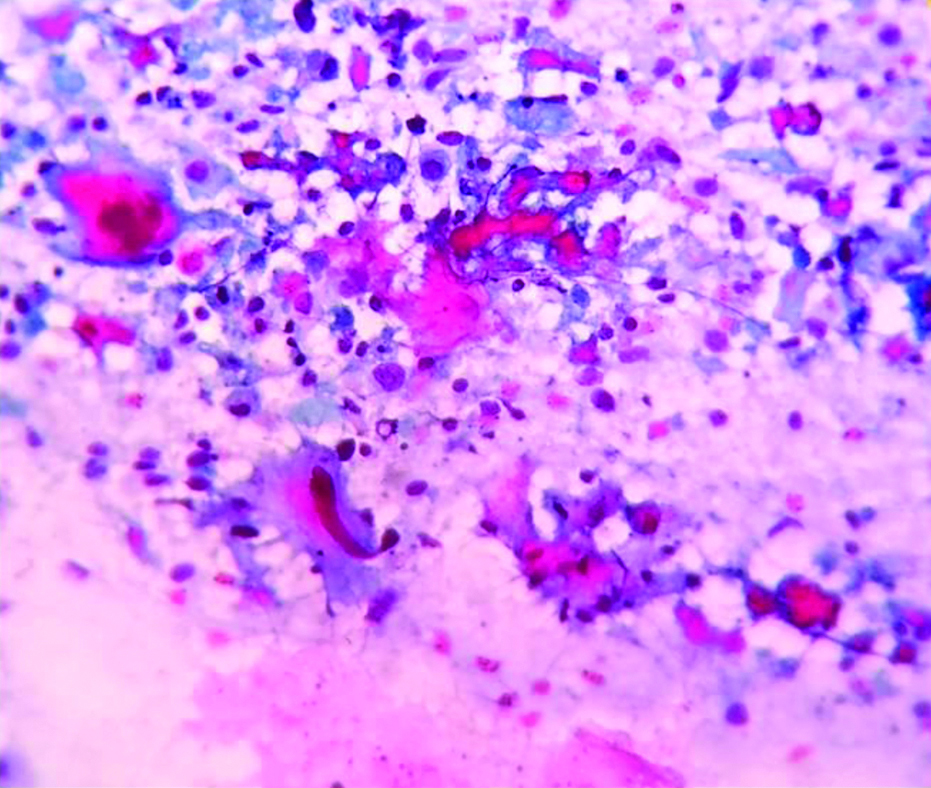
Malignant lesions were further categorised into primary and metastatic lesions. Primary malignancies included Non-Hodgkins lymphoma and Hodgkins lymphoma. Non-Hodgkins lymphoma was more common than Hodgkins lymphoma. Among metastasis, most common pattern was poorly differentiated carcinoma, followed by squamous cell carcinoma and least was adenocarcinoma. All malignant cases were seen in only adult population [Table/Fig-5,6].
Microphotograph of tissue section of Non-Hodgkin lymphoma-displaying relatively monomorphic lymphoid cells arranged in sheets. (H&E, X100).

Microphotograph of cytology smear of metastatic squamous cell carcinoma-displaying malignant squamous cells and tadpole cell in a background of few lymphocytes and proteinaceous material (PAP, X400).
Histopathological diagnosis was available in 13 cases. The diagnostic accuracy was 38.46% (five cases) by complete concordance and increased to 92.3% (12 cases) on applying partial concordance criteria in cytological diagnosis. Neoplastic lesions showed better Diagnostic Accuracy by Complete Concordance (DACC) in comparison with non-neoplastic lesions. Non-neoplastic lesions showed better Diagnostic Accuracy on applying Partial Concordance (DAPC) criteria [Table/Fig-7].
Comparison of diagnostic accuracies for lymph node lesions.
| Histopathology | Cases | Cytology | Discordant cases |
|---|
| DACC | DAPC |
|---|
| Non neoplastic | 7 (53.8%) | 2 (28.57%) | 7 (100%) | 0 |
| Chronic inflammatory lesion | 1 (7.69%) | 0 | 1 (100%) | 0 |
| Chronic granulomatous lymphadenitis | 2 (15.3%) | 1 (50%) | 2 (100%) | 0 |
| Reactive lymphadenitis | 1 (7.69%) | 1 (100%) | 1 (100%) | 0 |
| Mycobacterial lymphadenitis | 3 (23.07%) | 0 | 3 (100%) | 0 |
| Neoplastic | 6 (46.15%) | 3 (50%) | 5 (83.33%) | 1 (16.66%) |
| Squamous cell carcinoma | 4 (30.76%) | 2 (50%) | 3 (75%) | 1 (25%) |
| Adrenocortical carcinoma | 1 (7.69%) | 1 (100%) | 1 (100%) | 0 |
| Non-Hodgkins lymphoma (High grade) | 1 (7.69%) | 0 | 1 (100%) | 0 |
| 13 | 5 (38.46%) | 12 (92.30%) | 1 (7.69%) |
DACC: Diagnostic accuracy by complete concordance
DAPC: Diagnostic accuracy after considering partial concordance
“Complete Concordance” was applied to the cases in which cytological diagnosis was exactly identical to the final histopathological diagnosis.
“Partial Concordance” was applied to the cases in which the cytological diagnosis showed minor deviation from final histopathological diagnosis, but the lesion belong to the same category or one of the cytological differential diagnosis matched with final histopathological diagnosis.
“Discordance” was considered in cases where cytological diagnosis differed significantly from the final histopathological diagnosis.
The statistical values were calculated by Galen and Gambino method. For the detection of neoplastic lesions, cytological diagnosis had four true positive cases, zero false positive cases, two false negative cases, seven true negative cases, sensitivity of 100%, specificity of 77.8%, false positive error rate of 0%, false negative error rate of 15.38%, positive predictive value of 66.7%, negative predictive value of 100%, and diagnostic efficacy of 84.61%. The p-value determining the efficacy of cytological diagnosis for detecting neoplasms was statistically highly significant (p=0.009).
Discussion
Lymphadenopathy presenting as a clinical manifestation of the regional or systemic disease serves as an excellent clue to diagnose the underlying disease. It can arise either from benign or malignant aetiology [6]. FNAC is considered as first line investigation and plays an important role in the diagnosis of lymph node lesions [1,3]. The merits of FNAC was summarised by de May with the acronym SAFE which means Simple, Accurate, Fast and Economical [4]. Lymph node lesions can be found in patients with wide age range [6]. In the present study, the age of the paediatric population ranged from 6 months to 12 years, with clustering of cases seen in the age group of 7-9 years with a mean of 6.5 years. Singh N et al., had documented maximum number of cases in the age group of 5-10 years in their study [7]. Ahmed HG et al., had observed a mean of 7 years in their study [8]. In the present study, males were predominantly affected. Akhter R et al., Singh N et al., Ahmed HG et al., and Sawaimul K et al., had documented similar observation in their study [2,7-9].
Cervical lymph nodes were the most common group of lymph nodes involved in the present study. Singh N et al., Ahmed HG et al., and Sawaimul K et al., had documented similar observation [7-9]. Reactive lymphadenitis was the most common cytological pattern of lymph node lesions followed by tuberculous lymphadenitis in the studies conducted by Akhter R et al., Singh N et al., and Sawaimul K et al., [2,7,9]. Ahmed HG et al., had observed that reactive lymphadenitis was the most common pattern followed by granulomatous lymphadenitis [8]. In contrast to other studies, in the present study the reactive lymphadenitis was the most common pattern followed by acute suppurative lymphadenitis in the paediatric age group.
In adult population, age of the patients ranged from 13 to 80 years and clustering of cases was seen in 3rd decade. Shrivastav A et al., observed female predominance in the age group of 21-50 years [4]. Badge SA et al., and Janagam C and Atla B, also showed female preponderance in their study [3,10]. In contrast, males were predominantly affected in the adult population in the present study. Similarly, Malhotra AS et al., and Gayathri MN et al., also showed male preponderance in 3rd decade [6,11]. However, the studies had documented very wide age range. Cervical lymph node was predominantly involved in the present study. Badge SA et al,, Shrivastav A et al., Malhotra AS et al., and Gayathri MN et al., documented similar observations [3,4,6,11]. Tuberculous lymphadenitis was the most common cytological pattern of lymph node lesions followed by reactive lymphadenitis in the studies conducted by Shrivastav A et al., and Farooq S et al., [4,12]. In contrast, in the present study the reactive lymphadenitis was the most common pattern followed by chronic granulomatous lymphadenitis in the adult population.
[Table/Fig-8] shows the distribution of overall cytopathological pattern of lymph node lesions in various studies. In the present study, non-neoplastic lesions were more common than neoplastic lesions. Similar results were documented in the other studies. Reactive lymphadenitis (38.69%) was the most common non-neoplastic lesion observed in the present study. Bhatta S et al., Singh N et al., Janagam C and Atla B, Gayathri MN et al., and Farooq S et al., documented similar observation [1,7,10-12]. In contrast, Malhotra AS et al., Fatima S et al., and Gupta P et al., showed tuberculous lymphadenitis as the most common cytopathological pattern [6,13,14] [Table/Fig-8]. Gayathri MN et al., had included another entity named non-specific lymphadenopathy (18.5%) [11]. Similarly, Fatima S et al., had included non-diagnostic (12%) entities and Gupta P et al., included inadequate (4.67%) category in their study [13,14].
Comparison of overall cytopathological pattern of lymph node lesions in various studies [1,6,7,10-14].
| Authors (Place, Year of Publication) | Total cases | Reactive lymphadenitis | Granulomatous lymphadenitis | Mycobacterial/Tuberculous lymphadenitis | Necrotising lymphadentis | Acute suppurative lesions | Lymphoproliferative lesion | Malignancy |
|---|
| Fatima S et al., [13] (Pakistan, 2011) | 377 | 16.1 | - | 52.7 | - | 4.20 | 5.50 | 8.70 |
| Gayathri MN et al., [11] (India, 2015) | 1774 | 26.2 | 14.7 | 14.65 | - | 3.94 | - | 21.93 |
| Singh N et al., [7] (India, 2016) | 498 | 71.05 | 8.33 | 17.11 | - | 3.51 | - | 1.61 |
| Gupta P et al., [14] (India, 2016) | 300 | 19 | 9.33 | 45.33 | - | 01 | - | 5.67 |
| Malhotra AS et al., [6] (India, 2017) | 234 | 42.64 | - | 44.02 | - | - | - | 14.1 |
| Janagam C and Atla B [10] (India, 2017) | 200 | 47.5 | - | 30 | - | - | - | 15 |
| Bhatta S et al., [1] (Nepal, 2018) | 206 | 54.36 | - | 35.92 | - | 1.45 | - | 8.27 |
| Farooq S et al., [12] (India, 2018) | 100 | 37 | - | 32 | - | 9 | - | 28 |
| Present Study (India, 2020) | 274 | 38.69 | 20.80 | 12.77 | 3.28 | 8.76 | 2.19 | 13.50 |
Tuberculosis still remains as one of the leading cause of cervical lymphadenopathy in India. The diagnosis of tuberculosis in lymph nodes can be done by demonstrating AFB in FNA smears with ZN stain or Auramine-rhodamine stain, mycobacterial culture or by amplification of bacterial DNA by Polymerase Chain Reaction (PCR). Due to their cost and duration of time they are of limited use [15]. More recently, the WHO endorsed the GeneXpert which utilises a DNA-PCR technique for simultaneous detection of Mycobacterium tuberculosis (MTB) and Rifampicin resistance related mutations employing an automated bench top Cartridge Based Nucleic Acid Amplification (CB-NAAT) assay. It not only has the advantage of rapidity diagnosis but also detects even low MTB genomic copies in various specimens. However, GeneXpert does not eliminate the need of conventional microscopy, culture and anti-tubercular drug sensitivity which are required to monitor the course of the disease and resistance to drugs other than rifampicin [16].
Only those cases in which smears were positive for AFB were diagnosed as mycobacterial lymphadenitis in the present study. CN was the predominant cytological feature in mycobacterial lymphadenitis. AFB grading was correlated with the cytological pattern of mycobacterial lymphadenitis. Hemalatha A et al., had included a pattern where numerous macrophages were seen along with presence of numerous neutrophils [17]. Nidhi P et al., had included polymorphs with necrosis in their study [18]. Similar to the present study, Chand P et al., observed caseous necrotic material admixed with degenerated inflammatory cells as predominant pattern [19]. Maximum AFB positivity was seen in this group in their study. In contrast, studies conducted by Badge SA et al., Malhotra AS et al., and Hemalatha A et al., documented CN with ECG as the predominant pattern of tuberculous lymphadenitis [3,6,17]. The correlation of different grades of AFB staining pattern with cytomorphological patterns of tuberculous lymphadenitis provides information about the disease activity and immunity of the patient [5]. Only few studies have correlated AFB grading with the cytological patterns of mycobacterial lymphadenitis.
The pattern of immunologic response to MTB is mainly due to Type IV delayed hypersensitivity. It is characterised by proliferation of Th1 cells and production of cytokines (gamma interferon) and tumor necrosis factor-alpha by the activated macrophages. These macrophages aggregate around the center of the lesion to form a granuloma to effectively counteract the bacilli without causing further tissue destruction. Necrosis is seen in the central part is caseous type of necrosis. When the macrophage activity is feeble, the tissue destruction occurs. The lesion intensifies and the surrounding tissue undergoes destruction. The central necrosis undergoes liquefaction and contains abundant acid fast bacilli in it. Thus, granulomatous reaction with scanty or no necrosis would be associated with only few bacilli and lesions with scant or no granuloma would be expected to show more number of bacilli [17].
Malignant lesions are common in older age as elderly patients respond to infection with slight to moderate lymph node enlargement in contrast to children. Hence, elderly patients presenting with lymphadenopathy should be subjected to FNAC to rule out malignant lesion [1]. FNAC may be the only tool in the diagnosis of metastatic lesions in the lymph nodes. It can help to detect occult primary malignancies. For the diagnosis of lymphomas, the FNAC may suggest an initial diagnosis, which can be subsequently followed by histopathology and immunohistochemistry for confirmation of the diagnosis [20].
Histopathological diagnosis was available in 13 cases only (seven Non-neoplastic and six Neoplastic lesions). Out of seven non-neoplastic lesions, there was no discordance. But one case of neoplastic lesion showed discordance between cytological and histopathological diagnosis. It was reported as acute inflammatory lesion on cytology but it turned out to be moderately differentiated squamous cell carcinoma. The probable reason for misdiagnosis could be due to presence of abundant neurophils obscuring the diagnostic malignant cells. In the present study, DACC and diagnostic accuracy after applying partial concordance criteria (DAPC) was calculated. Most of the studies had not clearly specified about the criteria to be followed to consider concordance. This may be important because, not all the cases diagnosed by cytology can perfectly match with histopathological diagnosis, which is considered as gold standard.
For the detection of neoplastic lesion, the present study showed sensitivity of 100%, specificity of 77.8% and high diagnostic efficacy (84.61%). Malhotra AS et al., had documented a lower sensitivity (94.49%). Balaji J et al., had observed lower sensitivity (96%) and higher specificity (100%) in their study [6,21]. FNAC is an efficacious investigative procedure for the diagnosis of lymph node lesions. A variety of lymph node lesions may be diagnosed by cytology. Cytology plays a very important role as different lesions needs distinct line of management. It aids the clinician in decision making. It may be considered as primary investigative modality which helps the clinician to plan the further management of the patients.
Limitation(s)
Histopathology could not be performed in all the cases. This is because, most of the cases are empirically treated based on cytological diagnosis. Number of mycobacterial lymphadenitis cases in paediatric age group was very less. Hence, statistical analysis could not be performed.
The distribution of cytological patterns of lymph node lesions in paediatric and adult population were different. The values were found to be statistically highly significant. The distribution pattern may reflect diverse aetiologies, characteristics of offending agent, immune status and susceptibility of the target population.
Conclusion(s)
Distribution of cytological patterns of lymph node lesions in paediatric and adult populations are different and are found to be statistically significant. The distribution pattern may reflect diverse aetiologies, characteristics of offending agent, immune status and susceptibility of the target population. Cytological evaluation of lymph node lesions has high diagnostic efficacy for the diagnosis of neoplastic lesions.
*Chi-square test was the statistical tool used to perform statistical analysis
CN- Smears showing only CN; ECG- Smears showing only ECG, CN-ECG- Smears showing both CN and ECG, NCNG- Smears showing neither CN nor ECG, but sattered epithelioid cells or neutrophils may be seen
Grade 1+=AFB was found after a careful search
Grade 2+=AFB were singly scattered
Grade 3+=AFB were found in large numbers arranged in faggots and singly
DACC: Diagnostic accuracy by complete concordance
DAPC: Diagnostic accuracy after considering partial concordance