Anatomical variations are deviations from the standard structures and morphologies of bodily arrangements, a phenomenon commonly seen in arteries and nerves. A typical axillary artery extends from the outer border of the first rib to the lower edge of the teres major before the pectoralis minor divides the axillary artery into three parts. Within existing research, several variations have been seen in the branching of the axillary artery, particularly among the second and third divisions. This case report examines and describes the anatomical differences of the second and third division of the axillary artery in a 64-year-old Caucasian female; variations were found in the second division of the axillary artery, two thoracoacromial arteries, as well as the absence of the stemming lateral thoracic artery. Within the third division of the axillary artery, the subscapular artery supplying the latissimus dorsi (two branches), subscapularis (circumflex scapular artery), and the serratus anterior (two branches) muscles were identified and distally, the axillary artery bisected into the brachial and accessory brachial arteries. A genetic mutation, environmental factors, and embryological malformations are among the hypotheses associated with these anatomical variations. From a clinical standpoint, these variations may not produce impairment though the knowledge of an individual’s distinctive arrangements would aid in preventing unnecessary complications that could arise during particular interventions.
Case Report
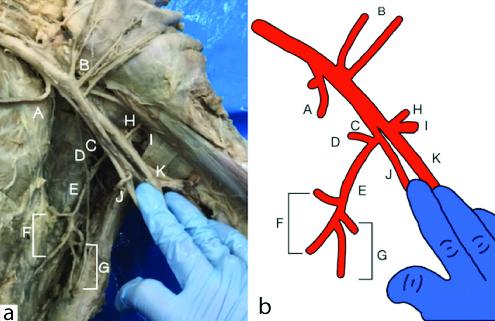
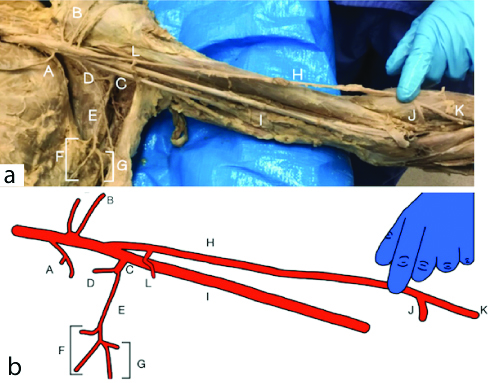
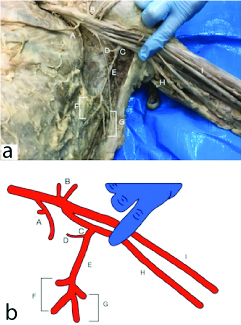
In 2017, the Axillary artery of a 64-year-old Caucasian female were dissected by first year physical therapy students at Texas Woman’s University School of Physical Therapy, Dallas. Upon dissection of the left upper extremity, the identified anatomical differences stemmed from the second and third division of the axillary artery. From the second division, an absent lateral thoracic artery and two thoracoacromial arteries were observed and identified by the muscles the arteries were supplying (pectoralis minor and deltoid muscles, [Table/Fig-1a,b]). Following the second division, the axillary artery bisected into two branches, the brachial and accessory brachial arteries. The accessory brachial artery was medial in comparison to the brachial artery, which was more lateral [Table/Fig-2a,b]. The subscapular artery then, branched from the accessory brachial artery producing the typical circumflex scapular and thoracodorsal arteries. From the thoracodorsal artery, four muscular branches were identified; two branches were irrigating the typical latissimus dorsi muscle, and two branches supplying the serratus anterior muscle [Table/Fig-3a,b]. At the proximal end of the forearm, the superficial brachial artery bisected into the radial and ulnar artery [Table/Fig-1a,b].
Variations of branching found in the left upper extremity axillary artery and its diagrammatic representation consisting of (A) Superior Thoracic, (B) Thoracoacromial, (C) Subscapular, (D) Circumflex Scapular, (E) Thoracodorsal, (F) Branches to the Serratus Anterior m., (G) Branches to the Latissimus Dorsi m., (H) brachial, (I) Accessory Brachial, (J) Ulnar, and (K) radial.
Variations of branching found in the left upper extremity axillary artery and its diagrammatic representation consisting of consisting of (A) Superior Thoracic, (B) Thoracoacromial, (C) Subscapular, (D) Circumflex Scapular, (E) Thoracodorsal, (F) Branches to the Serratus Anterior m., (G) Branches to the Latissimus Dorsi m., (H) Brachial, (I) Accessory Brachial, (J) Ulnar, (K) Radial, and (L) Branches to Latissismus dorsi.
Variations of branching found in the left upper extremity axillary artery and its diagrammatic representation consisting of (A) Superior Thoracic, (B) Thoracoacromial, (C) Subscapular, (D) Circumflex Scapular, (E) Thoracodorsal, (F) Branches to the Serratus Anterior m., (G) Branches to the Latissimus Dorsi m., (H) Accessory Brachial, and (I) Brachial arteries.
Discussion
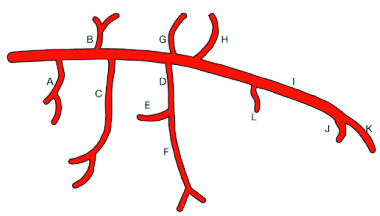
Several axillary artery variations have been found and illustrated in existing literature [1-3], with one variant being most commonly accepted among texts and taught in many anatomy courses [Table/Fig-4]. Hence, understanding the typical branching of the axillary artery is crucial to allow for the identification of atypical deviations [4].
Most commonly accepted variation of the axillary artery. The branches consist of (A) Superior Thoracic, (B) Thoracoacromial, (C) Lateral Thoracic, (D) Subscapular, (E) Anterior Circumflex Humeral, (F) upper part, Circumflex Scapular and lower part-branches of serratus anterior, (G) branches of latissimus dorsi, (H) Posterior Circumflex Humeral, (I) Brachial, (J) Ulnar, (K) radial, and (L) Deep Brachial arteries.
Variations in upper extremity arteries are routinely documented in dissections, and literature finds various authors noting branching patterns diverging from typical anatomical arrangements. Banerjee A et al., reported finding that nearly 62.5% of the population may have axillary artery variations [5], and according to Kumar N et al., anatomical differences are primarily located in the circumflex humeral, subscapular (third division of the axillary artery), and lateral thoracic arteries (second division of axillary artery) [6]. This case report outlines variations of the lateral thoracic, thoracoacromial, brachial, and thoracodorsal arteries.
Upon examining the variability of the lateral thoracic artery in 420 human cadavers, Loukas M et al., found that the lateral thoracic artery was present in 96.7% of the specimens [2]. Although the lateral thoracic artery is commonly present, a sizable morphological variability was reported, and from those findings, 67.2% were reported to be categorised as having the most common variation type.
Variations of the thoracoacromial artery within the axillary artery are rare [6], however, the absence of the thoracoacromial trunk with a terminal branch coming directly from the axillary artery, is the most common modification [7].
Our case report depicts four muscular branches stemming from the thoracodorsal artery, with two separate thoracoacromial arteries stemming directly from the axillary artery. In corroboration, Rikimaru H et al., describes the thoracoacromial artery rising from the axillary artery’s second division, cleaving into a deltoid and pectoral branch [8].
Additionally, the present case report illustrates the axillary artery bifurcation into a brachial and accessory brachial artery at the lower border of the teres major. Similarly, Chakravarthi KK et al., report a variation in a small percentage of 70 human dissected cadavers, making the occurrence of this variation relatively uncommon [9]. George BM et al., observed the axillary artery bifurcating into equal-sized trunks, the superficial and deep trunk [10]; the superficial continued as the brachial artery, and the deep trunk later bifurcated into the profunda brachii and the circumflex humeral-scapular trunk artery. Our findings are distinctive in that the accessory brachial branched into the subscapular artery, which produced the circumflex scapular and thoracodorsal arteries.
Moreover, the standard arrangement of the thoracodorsal artery is designed to supply the latissimus dorsi with blood, a norm unbeknown to the specimen subject to this report. We found the specimen’s thoracodorsal artery branches into four distinct arteries; two branches to supply the latissimus dorsi and two to supply the serratus anterior. It is noteworthy that the lateral thoracic artery, which ordinarily supplies the serratus anterior, was non-existent in the second section of the axillary artery. Kumar N et al., reported vaguely similar findings where the thoracodorsal artery originated independently off the second division of the axillary artery, though this specific deviation differs from our findings [6].
There are various reasons these types of anomalies can be found in the upper extremity. One of the causes can be attributed to genetic changes, including those among individuals with trisomy 13, 18, and 21. Since cadaver donations are confidential, we are unable to support or entirely rule out the concept of a genetic anomaly. However, there is a high rate of having significantly shortened life spans among individuals with these types of trisomies and given that our specimen was in her sixties, it is highly unlikely that the cause of her anatomical variation is due to a genetic disorder, though it is a possibility for other subjects [11].
The most likely explanation for these anatomical variances described in this report’s specimen could be abnormal changes during the embryological stages, specifically during cell differentiation [12]. The time frame for the formation of any anatomic anomaly occurs around the time of expansion of the small bud formation or precursors for the upper extremities appears, which is around the fourth week of embryonic development. Possibly, the buds which later form into the upper limb suffer small changes in the loose mesenchyme cells related to the ectoderm, creating anatomical deviation [12,13] including those mentioned within this report. Between weeks four and six, the precursor of the upper limb buds will increase in size and change pattern, creating the distal portion of the upper limb by the end of the 6th week. At this point, cellular division is complete and the window for opportunity for embryo variations has closed, therefore, any atypical anatomical variations will have taken place prior to the end of this embryological period.
We postulate teratogenic components to be an additional contributing factor to upper extremity anomalies. Literature shows that 10-15% of congenital structural abnormalities are a result of maternal exposure to environmental factors during embryonic development rather than genetic causes [14]. The effects of teratogens that are conducive to upper extremity variations, abnormalities, malformations, and defects can be caused by: 1) ionising radiation and infectious agents such as varicella, mumps, influenza, parvovirus, and other viral infections; 2) thermo-disruptions, specifically hyperthermia, during weeks 4 and 14 of embryonic development; 3) maternal chemical exposure to toluene which may lead to toluene embryopathy, can cause limb deformities of the embryo; 4) mothers who were alcoholics during their pregnancies have resulted in children with structural impairments found in nearly 50% of cases; and 5) the maternal use of drugs such as metronidazole, paramethadione, trimethadione, angiotensin converting enzyme inhibitors, dicumarol, coumarin derivatives, and cocaine during pregnancy [14]. Although the specific reason behind this type of anatomical variations is still unknown, it is imperative to report and learn about the different modifications. Having a clear delineated configuration of the upper extremity’s architecture could be beneficial in treatments, surgical interventions, and the prevention of complications.
Conclusion(s)
This case report illustrates a unique variation of the axillary artery in a female specimen. Akin to many other findings of similar nature, obvious limitations exist for providing specific explanations as to why these variations transpired. Regardless of the reason for its formation, the axillary artery has several deviations from the standard structures, such as the one depicted within this report. Though the majority of variations go undetected throughout an individual’s life, knowledge of these atypical arrangements would aid the prevention of difficulties that occur during interventions. Specific comprehension of typical and unorthodox arterial patterns in human anatomy is essential for any health professional working with the upper extremity, particularly experts in reparative surgery and angiography. The knowledge of this new-found additional artery modification may aid surgeons, physical therapists, occupational therapists, and other health professionals in understanding the possible functional variances among individuals with this difference in anatomical structure.
[1]. Roswell AR, Davies DM, Eisenberg N, Taylor GI, The anatomy of the subscapular-thoracodorsal arterial system: Study of 100 cadaver dissectionsBr J Plast Surg 1984 37:574-76.10.1016/0007-1226(84)90152-8 [Google Scholar] [CrossRef]
[2]. Loukas M, Du Plessis M, Owens DG, Kinsella CR, Litchfield RL, Nacar A, The lateral thoracic artery revisitedSurg Radiol Anat 2013 36:543-49.10.1007/s00276-013-1234-x24281130 [Google Scholar] [CrossRef] [PubMed]
[3]. Olinger A, Benninger B, Branching patterns of the lateral thoracic, subscapular, and posterior circumflex humeral arteries and their relationship to the posterior cord of the brachial plexusClin Anat 2010 234:407-12.10.1002/ca.2095820235185 [Google Scholar] [CrossRef] [PubMed]
[4]. Moore KL, Agur AMR, Dalley AF, Upper LimbIn Essential Clinical Anatomy 2015 5th edBaltimore, MDWolters Kluwer:397-484. [Google Scholar]
[5]. Banerjee A, Kumari C, Jhajhria SK, Variation in the branching pattern of third part of axillary artery- A case reportJ Clin Diagn Res 2017 11:01-04.10.7860/JCDR/2017/21605.924528384847 [Google Scholar] [CrossRef] [PubMed]
[6]. Kumar N, Aithal AP, Nayak SB, Bhaskar R, A rare case of atypical thoracodorsal artery: A challenge for flap reconstructionSurg Radiol Anat 2018 40:899-902.10.1007/s00276-018-2009-129594336 [Google Scholar] [CrossRef] [PubMed]
[7]. Trotter M, Henderson JL, Gass H, Brua RS, Weisman S, Agress H, The origins of branches of the axillary artery in whites and in American NegroesAnat Rec 1930 46:133-37.10.1002/ar.1090460205 [Google Scholar] [CrossRef]
[8]. Rikimaru H, Kiyokawa K, Inoue Y, Tai Y, Three-dimensional anatomical vascular distribution in the pectoralis major myocutaneous flapPlast Reconstr Surg 2005 115:1342-52.10.1097/01.PRS.0000156972.66044.5C15809597 [Google Scholar] [CrossRef] [PubMed]
[9]. Chakravarthi KK, Siddaraju KS, Venumadhav N, Sharma A, Kumar N, Anatomical variations of brachial artery- Its morphology, embryogenesis and clinical implicationsJ Clin Diagn Res 2014 8:01-20.10.7860/JCDR/2014/10418.530825653931 [Google Scholar] [CrossRef] [PubMed]
[10]. George BM, Nayak S, Kumar P, Clinically significant neurovascular variations in the axilla and the arm- A case reportNeuroanat 2007 6:36-38. [Google Scholar]
[11]. Pruszewicz A, Wiskirska-Woźnica B, Wojnowski W, Czerniejewska H, Jackowska J, Jarmuż M, Phenotype-genotype discordance in congenital malformations with communication disorders resembling trisomy 18 (Edwards syndrome)Am J Case Rep 2014 15:41-44.Published 2014 Jan 2310.12659/AJCR.88403324478819 [Google Scholar] [CrossRef] [PubMed]
[12]. Tickle C, Experimental embryology as applied to the upper limbJ Hand Surg Br 1987 12(3):294-300.10.1016/0266-7681(87)90177-X [Google Scholar] [CrossRef]
[13]. Aszewski JA, Singh P, Embryology, Hand. [Updated 2019 Feb 19]In: StatPearls [Internet] 2019 Jan Treasure Island (FL)StatPearls PublishingAvailable from: https://www.ncbi.nlm.nih.gov/books/NBK538240/ [Google Scholar]
[14]. Gilbert-Barness E, Teratogenic causes of malformationsAnnals of Clinical & Laboratory Science 2010 40(2):99-114.Retrieved March 20, 2019, from http://www.annclinlabsci.org/content/40/2/99.full10.33176/AACB-19-0002231205377 [Google Scholar] [CrossRef] [PubMed]
[15]. Sarkar S, Kundu B, De Bose A, Saha PK, Variation of branching pattern of axillary arteryInt J Anat Var 2014 7:27-29. [Google Scholar]