Cytomegalovirus (CMV) is a double-stranded Deoxyribonucleic Acid (DNA) virus which causes severe disease in immunocompromised individuals. Chorioretinitis accounts for 80-90% of CMV infection in patients with Acquired Immunodeficiency Syndrome (AIDS) having CD4 (Cluster of Differentiation) counts <50 μ/mL, and rarely in those with CD4 counts more than 100 μ/mL. In developing countries, CMV infection is known to cause blindness in 5-25% of Human Immunodeficiency Virus (HIV) infected individuals. After colitis, oesophagitis is the most common Gastrointestinal Tract (GIT) manifestation of CMV in immunocompromised individuals. In immunocompetent individuals the disease associated with CMV is often self-limiting. So, authors presented a case report of 40-year-old HIV infected male, with CD4 count of 75 μ/mL, having complaints of dysphagia and concomitant blindness. On the basis of an array of investigations, he was diagnosed as having CMV retinitis with oesophagitis. He had a predictable outcome after treatment with Gancyclovir (GCV). Thus, in immunocompromised individuals, especially with a CD4 count <100 μ/mL, surveillance of oesophagitis and retinitis with endoscopic and fundoscopic interventions, respectively, must be done. This can help in improving life expectancy in such individuals.
Case Report
A 40-year-old, immunocompromised male, presented with complaints of dysphagia with odynophagia since one month and painless loss of vision in both eyes, since three weeks. The loss of vision in both eyes was gradually progressive to almost only perception of light at present. Patient had no history of vomiting, cough, weight loss, breathlessness, strido, pain in eyes, watering of eyes, and redness of eyes. He was on therapy since five months for pulmonary tuberculosis and on Anti-Retroviral Therapy (ART) since six months (tenofovir/lamivudine/efavirenz). His last CD4 count (done three months back) was 75 cells/μL. On asking leading questions, it was revealed that he was not compliant to the treatment.
On general examination, patient appeared cachexic, afebrile, with pulse rate of 72/min, Blood Pressure of 120/80 mmHg. Systemic examination was unremarkable. On Visual examination, he had perception of rays in the right eye and perception of light in left eye.
On investigations, it was noted that was 6.5 g/dL, Renal Function Test (RFT) and Liver Function Test (LFT) were within normal limits. CMV IgM was 65 (>35 is positive) and CMV IgG was 0.92 (>0.75 is positive), performed using Enzyme Linked Immunosorbent Assay (ELISA) method.
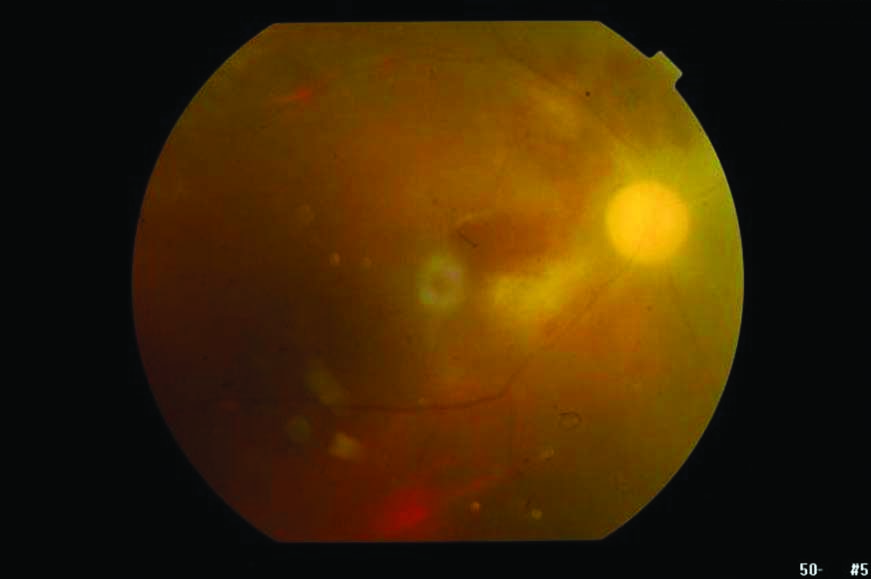
On fundoscopy, right eye showed evidence of retinal haemorrhages, pale disc and sclerosed vessels. Right eye also showed pale disc exudates and haemorrhage, and hazy view with vitritis [Table/Fig-1]. Left eye showed patch of retinitis below the optic nerve head and attenuated vessels [Table/Fig-2]. CMV retinitis in both eyes was suspected.
Right eye showing pale disc with surrounding exudates and haemorrhages; hazy view vitritis.

Left eye showed patch of retinitis below the optic nerve head, around vessels and whitening of retina.

Upper Gastrointestinal (GI) endoscopy was done in view of dysphagia and odynophagia. It revealed a large circular ulcer in the mid-oesophagus, which had an irregular margin and everted edge [Table/Fig-3]. Viral oesophagitis was suspected at this stage. Multiple biopsy samples were obtained to differentiate between herpes simplex and CMV infection. Histology of the biopsy specimen showed Cowdry B inclusion bodies, suggesting CMV virus as an aetiologic agent [Table/Fig-4].
Upper GI endoscopy showing a large circular ulcer with raised margins (black arrow).

H&E stained slide (100X) showing stratified squamous lining epithelium with atypical squamous cells, at places (arrow) intranuclear inclusion bodies in the squamous cells can be seen, (Cowdry B bodies).

Patient was given IV Gancyclovir (GCV) 5 mg/kg BD for four weeks and then 5 mg/kg once daily for two weeks. This resulted in improvement of the symptoms. Anti-Retroviral Therapy (ART) was continued along with Anti-Koch Therapy (AKT). Vision improved significantly to finger counting from six feet in the right eye and three feet in left eye, and also there was improvement in dysphagia. The ophthalmic findings of CMV retinitis showed resolution [Table/Fig-5,6].
Right eye showing resolution of haemorrhage and exudates as compared to previous fundoscopic examination [Table/Fig-1].
Left eye showing resolution of retinitis in comparison to [Table/Fig-2].

Tests for CMV antigeminemia were also positive. AKT was continued for total duration of eight months. ART was continued and CD4 counts were advised after three months. Total stay in hospital was six weeks but patient did not report back following post discharge.
Discussion
Cytomegalovirus (CMV) is a self-limiting infection in immunocompetent hosts. It may cause serious morbidity and even mortality in congenitally infected new borns, in transplant recipients and HIV infected individuals. In 80-90% of HIV infected individuals CMV presents as chorioretinitis [1]. The other manifestations are that of the GIT, peripheral nerves, encephalopathy and caudaequina syndrome [2]. CMV causes a mild flu-like illness initially. It may cause serious infections in immunocompromised individuals due to reactivation of this latent infection [3]. Ophthalmic manifestations of CMV range from blepharitis to retinitis and retinal detachment that can cause complete blindness. Various stages of ophthalmic involvement of the eye have been described [4-6].
Oesophagitis is the most common manifestation of CMV involvement in GIT after colitis. The presenting symptoms may be that of nausea, vomiting, dysphagia, chest pain, fever and anorexia. It is prevalent in patients with immunocompromised status such as bone marrow transplant recipients, patients on long term renal dialysis, those having HIV infections and those on immunosuppressive agents. Diagnosis is made by typical lesions on endoscopy, and histopathologic findings of biopsy of these lesions. Study of CMV antigens is not a very sensitive test and thus not diagnostic [7-9].
Both CMV retinitis and CMV oesophagitis are AIDS-defining conditions, typically found in patients with CD4 counts of <100 cells/μL and a viral load of >1,00,000 copies/mL [10]. HIV can affect any organ in the body. In 80% of HIV-infected patients ocular manifestations are observed, which in the vast majority reflect the systemic disease and may be the first sign of a disseminated infection. More than half of the patients with ocular involvement by CMV can have retinal microangiopathy which is a poor prognostic sign [11].
CMV retinitis usually appears in the late stages of the disease, in patient with a low CD4 count i.e., <50 μL/l [12,13]. The natural course causes damage of the retina in 2-3 months. The most common complications are macular damage (with marked decrease in visual acuity), optic neuropathy, optic nerve atrophy and retinal detachment. A routine fundoscopic screening examination in HIV affected individuals is necessary, especially in those with low CD4 counts [14]. Screening is necessary atleast every three months in such patients because CMV retinitis is often asymptomatic in the beginning for a long period and can directly present with complete blindness [15]. Routine eye screening by an ophthalmologist is clinically useful for HIV-1-infected patients with CD4 count less than 200/μL. Retinal detachment is a severe condition associated which needs surgical intervention [16].
A significant number of patients in India, with HIV-AIDS have evidence of active CMV infection. A study reported 32.4% of patients with AIDS had active CMV infection [17]. Biswas J et al., showed that ocular involvement was seen in 40% of HIV infected individuals [17].
Ophthalmic involvement by CMV is the most common cause of retinitis in immunocompromised patients, accounting to about 2/3rd of involvement of all target organs. However, involvement of the other organs is not uncommon, such as pulmonary, GIT or the nervous system. Colitis is the most common form followed by oesophagitis. GI involvement is 5-10% of the total involvement [18].
Findings of CMV oesophagitis on endoscopy are not very characteristic for the diagnosis. In this case the endoscopic findings show a large ulcer with raised margins. A report by Ohnuma H et al., described a large irregular map like ulcer with raised margins in an immunocompromised patient who was receiving chemotherapy for oesophageal cancer, whose aetiologic agent was known to be CMV [19].
A case report described an ulcer with a white base on endoscopy, in a study of CMV oesophagitis in patients on chemoradiotherapy for oesophageal cancer [20]. In another study, involving two Japanese patients, CMV infection was confirmed by histopathology of the biopsy specimen and viral antigenemia. The viral antigenemia was negative and biopsy results were also normal post antiviral treatment in these patients [21]. Irregular ulcers with raised margins were seen on endoscopy which on histopathology by Giemsa staining showed intracytoplasmic inclusion bodies [21]. In 2018, Fernandes MBT et al., published a study on GI CMV disease and tuberculosis of the GIT [22].
The three antiviral drugs used in CMV infection are GCV, foscarnet and cidofovir. Foscarnet is used in patients resistant to GCV or in those who have major side effects like leucopenia due to GCV. Foscarnet is nephrotoxic. Valagancyclovir (VGCV) is a pro-drug of GCV and has benefits of once a day dosing, more bioavailabibility and prevention of resistance to the drug [21]. In studies by Jabs DA et al., and Lapere SR et al., intravenous GCV injections have shown good response in patients with CMV retinitis [23,24].
Conclusion(s)
The index patient had concomitant retinitis and oesophagitis due to CMV. There should be surveillance like early fundoscopic screening and GIT endoscopy, in immunocompromised patients with CD4 counts less than 100 μ/mL. Patients with CMV oesophagitis may present with symptoms, but CMV retinis may remain asymptomatic for a long time until it presents as severe visual impairment. Prophylaxis can prevent major CMV manifestations in these patients. Even though the prophylaxis strategy is cost-effective, but, surveillance is even less costly and is a better option for early diagnosis and prevention of complications. Tissue biopsy is diagnostic in such cases. Biopsy of oesophageal ulcer was diagnostic in this case. Since vision was improving vitreous biopsy was not performed.
CMV can involve more than one organ in immunocompromised people. Thus, a possibility of more than one organ involvement in a HIV infected patient should always be kept in mind for better life expectancy in such patients.
[1]. Jacobson MA, Mills J, Serious cytomegalovirus disease in the acquire immunodeficiency syndrome (AIDS)Ann Intern Med 1988 108:585-94.10.7326/0003-4819-108-4-5852831765 [Google Scholar] [CrossRef] [PubMed]
[2]. Kestelyn PG, Cunningham ET, HIV/AIDS and blindnessBull World Health Organ 2001 79:208-13. [Google Scholar]
[3]. Mujtaba S, Varma S, Sehgal S, Cytomegalovirus co-infection in patients with HIV/AIDS in north IndiaIndian J Med Res 2003 117:99-103. [Google Scholar]
[4]. Regillo C, Cytomegalovirus infection. Retina and VitreousAmerican Academy of Ophthalmology 2006 :192-193. [Google Scholar]
[5]. Wiegand TW, Young LHY, Cytomegalovirus retinitisInt Ophthalmol Clin 2006 46:91-110.10.1097/00004397-200604620-0001016770157 [Google Scholar] [CrossRef] [PubMed]
[6]. Kanski JJ, Bowling B, Clinical ophthalmology: A systematic approachElsevier Health Sciences 2011 Apr 28 10.1016/B978-0-7020-4093-1.00019-7 [Google Scholar] [CrossRef]
[7]. Hoshino K, Shibata D, Miyagi T, Cytomegalovirus-associated gastric ulcers in a patient with dermatomyositis treated with steroid and cyclophosphamide pulse therapyEndoscopy 2011 43:E277-78.10.1055/s-0030-125642221915824 [Google Scholar] [CrossRef] [PubMed]
[8]. Kakugawa Y, Kami M, Matsuda T, Endoscopic diagnosis of cytomegalovirus gastritis after allogeneic hematopoietic stem cell transplantationWorld J Gastroenterol 2010 16:2907-12.10.3748/wjg.v16.i23.290720556837 [Google Scholar] [CrossRef] [PubMed]
[9]. Wilco CM, Chalasani N, Lazenby A, Cytomegalovirus colitis in acquired immunodeficiency syndrome: A clinical and endoscopic studyGastrointest Endsc 1998 48:3910.1016/S0016-5107(98)70126-9 [Google Scholar] [CrossRef]
[10]. Jacobson MA, Zegans M, Pavan PR, O’Donnell JJ, Sattler F, Rao N, Cytomegalovirus retinitis after initiation of highly active antiretroviral therapyThe Lancet 1997 349(9063):1443-45.10.1016/S0140-6736(96)11431-8 [Google Scholar] [CrossRef]
[11]. Jabs DA, Ocular manifestations of HIV infectionTrans Am Ophthalmol Soc 1995 93:623 [Google Scholar]
[12]. Ausayakhun S, Keenan JD, Ausayakhun S, Jirawison C, Khouri CM, Skalet AH, Clinical features of newly diagnosed cytomegalovirus retinitis in northern ThailandAm J Ophthalmol 2012 153(5):923-31.10.1016/j.ajo.2011.10.01222265148 [Google Scholar] [CrossRef] [PubMed]
[13]. Leenasirimakul P, Liu Y, Jirawison C, Khienprasit N, Kamphaengkham S, Ausayakhun S, Risk factors for CMV retinitis among individuals with HIV and low CD4 count in northern Thailand: Importance of access to healthcareBrit J Ophthalmol 2016 100:1017-21.10.1136/bjophthalmol-2016-30855627297217 [Google Scholar] [CrossRef] [PubMed]
[14]. Holland GN, AIDS and ophthalmology: The first quarter centuryAm J Ophthalmol 2008 145(3):397-408.e391.10.1016/j.ajo.2007.12.00118282490 [Google Scholar] [CrossRef] [PubMed]
[15]. Nishijima T, Yashiro S, Teruya K, Kikuchi Y, Katai N, Oka S, Routine eye screening by an ophthalmologist is clinically useful for HIV-1-infected patients with CD4 count less than 200/μLPLoS One 2015 10(9):e013674710.1371/journal.pone.013674726375282 [Google Scholar] [CrossRef] [PubMed]
[16]. Jabs DA, Ahuja A, Van Natta M, Dunn J, Yeh S, Comparison of treatment regimens for cytomegalovirus retinitis in patients with AIDS in the era of highly active antiretroviral therapyOphthalmology 2013 120(6):1262-70.10.1016/j.ophtha.2012.11.02323419804 [Google Scholar] [CrossRef] [PubMed]
[17]. Biswas J, Madhavan HN, George AE, Kumaraswamy N, Solomon S, Ocular lesions associated with HIV infection in India: A series of 100 consecutive patients evaluated at a referral centerAm J Ophthalmol 2000 129:09-15.10.1016/S0002-9394(99)00415-8 [Google Scholar] [CrossRef]
[18]. De Silva R, Stoopack PM, Raufman JP, Esophageal fistulas associated with mycobacterial infection in patients at risk for AIDSRadiology 1990 175(2):449-53.10.1148/radiology.175.2.23264722326472 [Google Scholar] [CrossRef] [PubMed]
[19]. Ohnuma H, Sato Y, Takayama T, Esophageal cancer complicated by cytomegalovirus esophagitis during chemoradiotherapy: Case reportGastrointest Endsc 2003 57:622-26.10.1067/mge.2003.15012665790 [Google Scholar] [CrossRef] [PubMed]
[20]. Umemoto K, Kojima Y, Nagata N, Yokoi C, Sakurai T, Kobayakawa M, Cytomegalovirus esophagitis developing during chemoradiotherapy for esophageal cancer: Two case reportsJournal of Medical Case Reports 2016 10(1):25910.1186/s13256-016-0947-y27655584 [Google Scholar] [CrossRef] [PubMed]
[21]. Emery VC, Prophylaxis for CMV should not now replace pre-emptive therapy in solid organ transplantationRev Med Virol 2001 11:83-86.10.1002/rmv.31011262527 [Google Scholar] [CrossRef] [PubMed]
[22]. Fernandes MBT, Cardoso PANM, Altoé LB, de Castro IJ, da Silva GAR, de Araújo Eyer-Silva W, Gastrointestinal CMV disease and tuberculosis in an AIDS patient: Synergistic interaction between opportunistic co-infectionsCase Reports in Medicine 2018 2018:804789210.1155/2018/804789229991949 [Google Scholar] [CrossRef] [PubMed]
[23]. Jabs DA, Ahuja A, Van Natta ML, Lyon AT, Yeh S, Danis R, Long-term outcomes of cytomegalovirus retinitis in the era of modern antiretroviral therapy: Results from a United States cohortOphthalmology 2015 122(7):1452-63.10.1016/j.ophtha.2015.02.03325892019 [Google Scholar] [CrossRef] [PubMed]
[24]. Lapere SR, Rice JC, Cytomegalovirus retinitis in Cape Town, South Africa: Clinical management and outcomesS Afr Med J 2017 107(6):514-17.10.7196/SAMJ.2017.v107i6.1225028604324 [Google Scholar] [CrossRef] [PubMed]