Thunderclap Headache in a Patient with Dengue
Krishnan Balagopal1, Jeyaseelan Nadarajah2, Baishyak Renuji3, Riya Ann Koshy4, Aswin Chembodi Gopalakrishnan5
1 Consultant Neurologist, Department of Neurology, MOSC Medical College, Kolenchery, Kochi, Kerala, India.
2 Interventional Radiologist, Department of Radiology, MOSC Medical College, Kolenchery, Kochi, Kerala, India.
3 Consultant Neurologist, Department of Neurology, MOSC Medical College, Kolenchery, Kochi, Kerala, India.
4 Resident, Department of Neurology, MOSC Medical College, Kolenchery, Kochi, Kerala, India.
5 Resident, Department of Neurology, MOSC Medical College, Kolenchery, Kochi, Kerala, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Krishnan Balagopal, Consultant Neurologist, Department of Neurology, MOSC Medical College, Kolenchery, Kochi-682311, Kerala, India.
E-mail: krishnan.balagopal@gmail.com
Dengue fever, Platelet transfusion, Posterior reversible encephalopathy syndrome
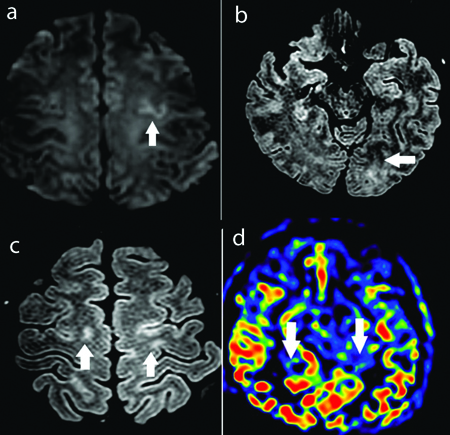
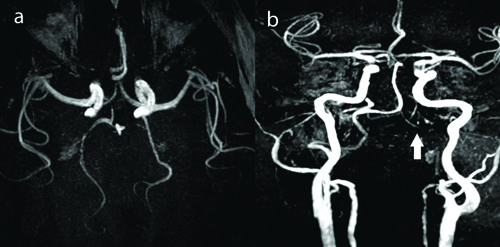
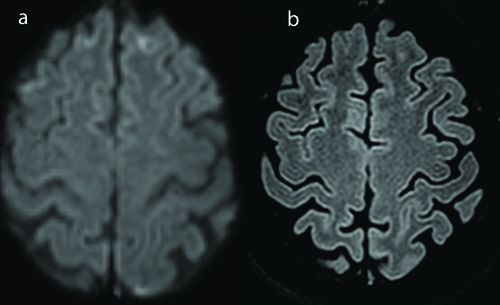
A 45-year-old female patient with no prior comorbidities was admitted with three-day history of high-grade intermittent fever followed by generalised tiredness. There was no history of joint pains, prior headache or seizures. Serology for dengue was positive and she was admitted in the Department of Internal Medicine. She was managed conservatively with hydration and antipyretics. She had drop in platelet counts to less than 10000/μL which required administration of platelet transfusion. Immediately after platelet transfusion, patient developed sudden onset of severe thunderclap headache associated with elevated blood pressures (>160/90 mm). The headache was noted to increase with blood pressure rise. There was no history of weakness of limbs or blurred vision. Clinical examination revealed no focal neurological deficits or meningeal signs. Magnetic Resonance Imaging (MRI) of the brain [Table/Fig-1] showed T2 weighted hyperintensities involving the left occipital and bilateral fronto parietal regions. There was evidence of focal restricted diffusion on Diffusion Weighted Imaging (DWI) sequences and no evidence of contrast enhancement. MR Angio (MRA) [Table/Fig-2] showed evidence of multifocal stenosis and narrowing involving the left vertebral and right posterior cerebral arteries. The scans were discussed with the neuroradiology team and were felt to be suggestive of Posterior Reversible Encephalopathy Syndrome (PRES). The differentials considered were primary CNS angiitis and cerebral venous thrombosis. She was managed with antioedema measures and anti-hypertensive agents-Mannitol at a dose of 0.5 mg/kg/day, hypertonic saline infusion at 15 mL per hour and labetalol 200 mg per day and had complete resolution of symptoms. She was discharged after improvement. At two weeks follow-up, patient was asymptomatic and had no deficits. Repeat MRI done after three months showed complete resolution of the abnormalities seen on the initial scans confirming a diagnosis of PRES [Table/Fig-3].
a) Axial DWI images showing focal cortical diffusion restriction in left frontal region (arrows). b,c) Axial FLAIR images showing cortical sub cortical high signal intensity in left occipital region and bilateral fronto parietal parasagittal location (arrows). d) Axial ASL colour map showing patchy region of elevated perfusion in bilateral occipital lobe (arrows).
a) MRA coronal images showing irregularity with multifocal stenosis in right PCA (arrow). b) MRA axial image showing stenosis in Left Vertebral Artery V4 segment (arrow).
a) T2 FLAIR and b) Diffusion images showing complete resolution of lesions.
PRES is a clinico-radiological syndrome that was initially described by described by Hinchey et al., in 1996 [1]. The characteristic features include holocranial headache, altered mental status, seizures, and visual disturbances [2]. Visual disturbances can range from blurring of vision to field defects and cortical blindness [3]. Seizures can progress to convulsive and non-convulsive status epilepticus [4]. Other clinical features may include brainstem symptoms like nausea, gait ataxia and vomiting. The radiological features include white matter vasogenic oedema affecting the posterior occipital and parietal lobes of the brain. Conditions causing a sudden increase on blood pressure are those implicated in the pathogenesis of PRES. Peak blood pressures seen in this condition are usually in the range of 150 to 170 mmHg systolic. These include conditions like acute kidney injury, eclampsia and Guillain-Barré syndrome. Other causes include autoimmune diseases like thrombotic thrombocytopenic purpura and systemic lupus erythematosus, exposure to immunosuppressive drugs such as cyclosporine, tacrolimus and other chemotherapy agents [5]. The common pathogenesis is the breakdown of the blood-brain barrier causing endothelial dysfunction. Most of these cases have a good long term prognosis and recover well without any neurological sequelae. The evaluation of PRES includes a detailed clinical assessment including ophthalmological evaluation of fundi, vasculitis markers in serum, MRI imaging with MRA and lumbar puncture if needed. Differentials include Primary CNS Angiitis, Acute Demyelinating Encephalomyelitis (ADEM), Progressive Multifocal Leukoencephalopathy (PML) and ischaemic stroke. Management includes treatment of primary pathology, control of blood pressures, anticonvulsants and antioedema measures if needed. Thunderclap headaches are described as the most severe headache ever by patients and reach their peak within a few minutes. The two most common causes include Subarachnoid haemorrhage and PRES [6]. Other causes include arterial dissections, intracranial haemorrhage, tumuors and venous thrombosis. There are two mechanisms that may be responsible for PRES in this case. The symptoms were caused immediately after platelet transfusion and this could have been a precipitating factor. There are multiple case reports of transfusion associated PRES. Blood transfusion leads to increased blood flow and viscosity, which causes impaired hypoxic vasodilation. This in turn leads to an increase in vascular resistance, leading to generalised cerebral vessel constriction [7].
There are a few case reports of PRES occurring as a complication of dengue fever itself and the pathogenesis has not been fully understood [8,9]. The main reason could be related to endothelial dysfunction that leads to vasogenic oedema and decreased cerebral blood flow. Also, inflammatory cytokine release can increase vascular permeability with consequent brain oedema and PRES. The patient in the present case had dengue fever but developed symptoms immediately after a transfusion. The precipitating factor in the present case could have been both the dengue per se and the transfusion associated complication. This report highlights the importance of prompt recognition and treatment of this rare but important cause of headache in dengue patients.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jun 04, 2024
Manual Googling: Jul 16, 2024
iThenticate Software: Jul 30, 2024 (3%)
[1]. Hinchey J, Chaves C, Appignani B, Breen J, Pao L, Wang A, A reversible posterior leukoencephalopathy syndromeN Engl J Med 1996 334(8):494-500. [Google Scholar]
[2]. Dou YH, Fuh JL, Chen SP, Wang SJ, Reversible cerebral vasoconstriction syndrome after blood transfusionHeadache 2014 54(4):736-44. [Google Scholar]
[3]. Sudulagunta SR, Sodalagunta MB, Kumbhat M, Nataraju AS, Posterior reversible encephalopathy syndrome (PRES)Oxf Med Case Reports 2017 2017(4) [Google Scholar]
[4]. Ninomiya I, Kanazawa M, Akaiwa Y, Shimohata T, Okamoto K, Onodera O, Apparent diffusion coefficient reduction might be a predictor of poor outcome in patients with posterior reversible encephalopathy syndromeJ Neurol Sci 2017 381:01-03. [Google Scholar]
[5]. Fugate JE, Rabinstein AA, Posterior reversible encephalopathy syndrome: Clinical and radiological manifestations, pathophysiology, and outstanding questionsLancet Neurol 2015 14(9):914-25. [Google Scholar]
[6]. Schwedt TJ, Thunderclap HeadacheContinuum (Minneap Minn) 2015 21(4 Headache):1058-71. [Google Scholar]
[7]. Mitaka H, Seijo L, Motohashi K, Nakai M, Burger A, Posterior reversible encephalopathy syndrome induced by red blood cell transfusionQJM 2019 112(8):617-18. [Google Scholar]
[8]. Mai NTH, Phu NH, Nghia HDT, Phuong TM, Duc DT, Chau NVV, Dengue-associated posterior reversible encephalopathy syndrome, VietnamEmerg Infect Dis 2018 24(2):402-04. [Google Scholar]
[9]. Biswas HK, Ibu KTI, Biswas R, Ahmed MNU, Posterior reversible encephalopathy syndrome associated with dengue fever induced intrauterine death: A case reportClin Case Rep 2024 12(3):e8575 [Google Scholar]