Dental caries is a complicated disease caused by microbiological shifts within the biofilm, salivary flow, fluoride exposure, dietary sugar consumption, and preventive behaviours. Early Childhood Caries is an aggressive form of dental caries that begins on tooth surfaces, such as the labial surfaces of maxillary incisors, which may appear unaffected by decay [1]. In India, the prevalence of ECC is 44% among children aged 8 to 48 months and 40.6% among those aged zero to three years in rural South India, with 50.3% having non cavitated surfaces and 49.7% having cavitated surfaces [2,3]. Despite significant progress in caries control, the high prevalence of ECC in young children persists, even with recent advancements [4].
Any change in the amount or quality of saliva can jeopardise oral health. The anti-decay properties of saliva are affected by its flow and pH, which improve the overall oral environment by preventing tooth demineralisation through oral buffering. If, the pH of the mouth remains below 5.5 for an extended period, demineralisation can lead to caries [5]. Dental caries is most prevalent when the pH drops, with dissolution occurring below the critical level of 5.5; thus, maintaining a pH of 6.7 is crucial for the integrity of tooth structure [6]. The total calcium and phosphate content in saliva can influence this, potentially changing by one pH unit [7].
Fagamin SDF 38% from Tedequim is one such material that can be used in preventive treatment. This colourless liquid contains 38% (44,800 ppm) fluoride ions at a pH of 10, comprising 25% silver, 8% ammonia, 5% fluoride, and 62% water [8]. Ammonia helps stabilise the SDF solutions, fluoride ions facilitate the remineralisation process, and silver ions act as antibacterial agents [9]. SDF is non invasive, easy to apply, and has no significant side effects apart from the staining of carious lesions due to the deposition of silver phosphate and silver sulfide [10].
Salivary proteins and peptides are essential for the adhesion of oral microorganisms and the maintenance of tooth surfaces [11]. The flow rate, buffering capacity, pH, and consistency of saliva affect caries risk, with bicarbonate ions protecting teeth from acid attacks. A lack of saliva can lead to dental cavities [12]. However, very few studies have examined the changes in the pH of saliva before and after the application of commercially available 38% SDF solution at different time intervals [5,13,14]. Therefore, the main aim of present study was to evaluate the pH changes at three different intervals after the application of 38% SDF, as well as to compare these changes based on age, gender, and the number of decayed teeth.
Materials and Methods
This pre-post single-group quasi-experimental study was conducted in the Department of Paediatric and Preventive Dentistry at Rajarajeswari Dental College and Hospital in Bengaluru, Karnataka, India from September 2021 to February 2022. A total of 15 patients with ECC, aged 3-6 years, were selected for the application of 38% SDF. Ethical clearance was obtained from the Institution, with reference number RRDCET/01PEDO/2019.
Inclusion criteria: Children with active carious lesions, specifically those with four or more cavities, and parents who provided consent for the study were included.
Exclusion criteria: Children who had received a fluoride topical application within the last 48 hours, children with special healthcare needs, those with pulpally involved teeth, and children who had received antibiotic therapy within the past three months were excluded from the study.
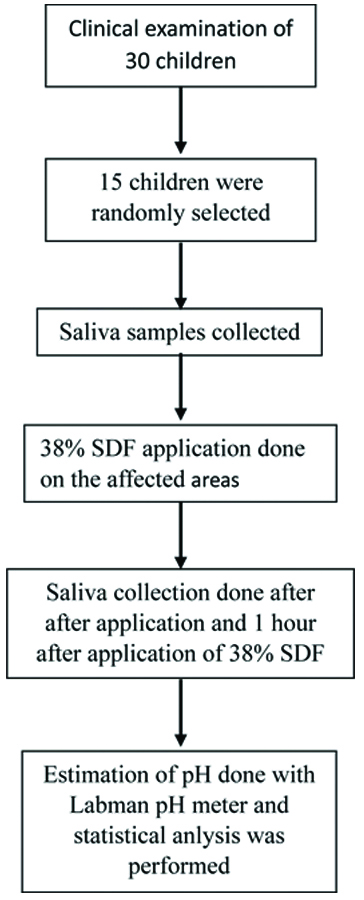
Sample size calculation: The sample size was estimated using GPower software version 3.1.9.2. Considering the effect size to be measured (f) at 40% [15], a study power of 80%, a margin of error of 5%, the number of repeated measures at three, and the correlation between repeated measures at 0.35, the total sample size needed was determined to be 15 [Table/Fig-1]. An examination of 30 children was conducted, and 15 children were selected through randomisation using computer-generated allocation. The proposed study was carried out on 15 patients aged 3 to 6 years with ECC. Informed consent was obtained after briefly explaining the clinical procedure and addressing all questions regarding SDF before their inclusion in the study.
Study Procedure
Sample preparation: A clinical examination was conducted using a dental mirror and explorer on children, with visual inspection for cavitated dentinal caries. Children with four or more caries were selected for evaluation by the primary investigator [Table/Fig-2a]. Unstimulated saliva samples were collected before the application of SDF.
(a) Shows anterior view of a child with caries; (b) Shows 38% SDF solution and applicator tip; (c) Shows the application of SDF in carious lesion; (d) Shows 2 mL vial used for saliva collection.

A protective coating of Vaseline was applied to each child before the SDF application, followed by drying the carious lesions with compressed air. Excess liquid was removed prior to application, and the SDF was directly applied to the affected teeth to minimise systemic absorption [Table/Fig-2b,c]. The application time was one minute. Unstimulated saliva samples were collected immediately after application and one hour after application.
Saliva samples were collected from eligible subjects while they were seated upright with their heads inclined forward, and they were asked to spit approximately 2 mL of saliva into Eppendorf tubes [Table/Fig-2d]. All samples were sent to the laboratory for evaluation, and the laboratory investigator was blinded to the participants’ identities. Additionally, all participants were blinded to group allocation.
Laboratory procedure: The estimation of pH was conducted in the laboratory after samples were transported using a Labman digital pH meter, which was mounted on a sturdy stand to avoid variations in the readings. The meter features a long stem with a double-junction gel-filled electrode, allowing for the measurement of small sample quantities. The electrode was immersed in the sample, and the digital reading stabilised for a few seconds before being recorded as the final salivary pH value. The collected data underwent statistical analysis.
Statistical Analysis
Data analysis was performed using the Statistical Package for the Social Sciences (SPSS) for Windows, version 22.0, released in 2013 (Armonk, NY: IBM Corp.). The level of significance was set at α=0.05. Repeated measures Analysis of Variance (ANOVA) was used to compare mean salivary pH levels at different time intervals among study subjects. Bonferroni’s post-hoc test was employed for multiple comparisons of mean differences in salivary pH levels between different time intervals. Age-wise and gender-wise comparisons of mean salivary pH levels at different time intervals were conducted using an independent t-test.
Results
Among the 15 participants included in the study, the average age of the subjects was 4.60±1.06 years. Among the study participants, 9 (60.0%) were males and 6 (40.0%) were females. The mean salivary pH levels before the application of SDF was 6.45±0.22, immediately after SDF application was 6.95±0.18, and 1 hour after application was 7.30±0.27. The differences in the mean salivary pH levels between the various time intervals among children with ECC were statistically significant at p-value <0.001 [Table/Fig-3]. The mean salivary pH levels increased from before, to immediately after, and then after a 1-hour interval following the application of SDF, indicating that SDF plays a key role in reducing caries by increasing pH levels [Table/Fig-4].
Comparison of mean salivary pH levels at different time intervals among study subjects.
| Time | n | Mean±SD | Min | Max | p-value |
|---|
| Before | 15 | 6.45±0.22 | 6.1 | 6.8 | <0.001* |
| Immediate | 15 | 6.95±0.18 | 6.7 | 7.3 |
| After | 15 | 7.30±0.27 | 6.9 | 7.7 |
*Statistically significant
Mean salivary pH levels at different time intervals among study subjects.
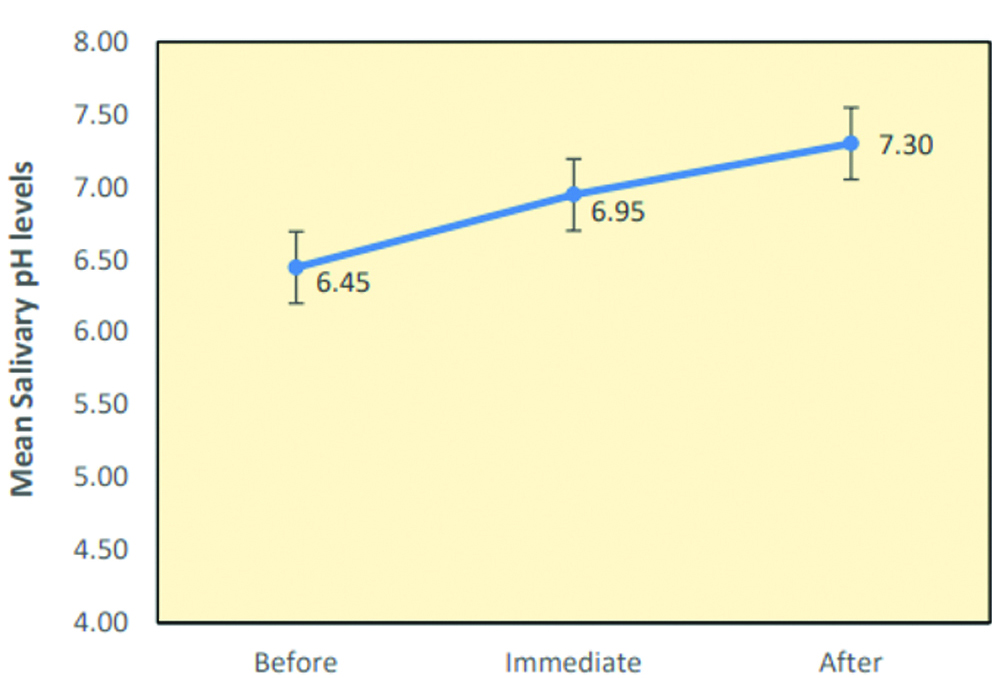
Multiple comparisons of the mean differences between time intervals revealed that the mean salivary pH level after 1 hour of SDF application was significantly higher compared to the levels immediately after application and before application, with mean differences being statistically significant at p-value <0.001 [Table/Fig-5].
Multiple comparison of mean differences in salivary pH levels between different time intervals using Bonferroni’s Post-hoc test.
| (I) Time | (J) Time | Mean diff.(I-J) | 95% CI for the difference | p-value |
|---|
| Lower | Upper |
|---|
| Before | Immediate | -0.50 | -0.62 | -0.38 | <0.001* |
| After | -0.85 | -1.07 | -0.63 | <0.001* |
| Immediate | After | -0.35 | -0.49 | -0.22 | <0.001* |
*Statistically significant
A comparison of mean pH between the 3-4 year and 5-6 year age groups was conducted using an Independent Student’s t-test. In both groups, there was a consistent increase in pH across the consecutive time intervals, but this was not statistically significant (p>0.05) [Table/Fig-6]. As age increased, pH also increased before application, immediately after application, and after the application of SDF. A higher mean pH was observed in older individuals; however, no significant statistical difference between pH and different age groups was found (p>0.05).
Age-wise comparison of mean salivary pH levels at different time intervals using independent Student’s t-test.
| Time | Age | n | Mean±SD | Mean diff. | p-value |
|---|
| Before | 3-4 y | 6 | 6.33±0.24 | -0.19 | 0.11 |
| 5-6 y | 9 | 6.52±0.18 |
| Immediate | 3-4 y | 6 | 6.95±0.16 | 0.01 | 0.96 |
| 5-6 y | 9 | 6.94±0.21 |
| After | 3-4 y | 6 | 7.42±0.26 | 0.19 | 0.19 |
| 5-6 y | 9 | 7.22±0.26 |
A comparison of mean pH at different time intervals between the two genders was also performed using an independent Student’s t-test. In males, the increase in pH was greater compared to their female counterparts across the three different time intervals. Consequently, a higher mean pH was recorded in males than in females, but this was not statistically significant (p>0.05) [Table/Fig-7].
Gender-wise comparison of mean salivary pH levels at different time intervals using independent Student’s t-test.
| Time | Gender | n | Mean±SD | Mean diff. | p-value |
|---|
| Before | Males | 9 | 6.44±0.24 | -0.01 | 0.96 |
| Females | 6 | 6.45±0.22 |
| Immediate | Males | 9 | 6.97±0.20 | 0.05 | 0.63 |
| Females | 6 | 6.92±0.17 |
| After | Males | 9 | 7.40±0.27 | 0.25 | 0.08 |
| Females | 6 | 7.15±0.21 |
Finally, a comparison of mean pH between the two groups concerning the number of decayed teeth was conducted using an Independent Student’s t-test. The increase in pH was more pronounced in children with more than 5 carious teeth compared to children with 5 or fewer carious teeth. Thus, as the number of carious teeth increased, pH also increased immediately and after the application of SDF, resulting in a more alkaline pH and a reduction in caries incidence (p>0.05) [Table/Fig-8].
Comparison mean salivary pH levels at different time intervals based on the caries scores using independent Student’s t-test.
| Time | Caries | n | Mean±SD | Mean diff. | p-value |
|---|
| Before | ≤5 no. | 5 | 6.42±0.16 | -0.04 | 0.75 |
| >5 no. | 10 | 6.46±0.25 |
| Immediate | ≤5 no. | 5 | 6.88±0.19 | -0.10 | 0.34 |
| >5 no. | 10 | 6.98±0.18 |
| After | ≤5 no. | 5 | 7.22±0.29 | -0.12 | 0.44 |
| >5 no. | 10 | 7.34±0.27 |
Discussion
The study assessed the impact of SDF application on salivary pH at three different time intervals, showing that the mean salivary pH increased as the time interval increased. SDF is a colourless liquid solution containing silver, fluoride, and ammonia, which aids in remineralisation and reduces dentin hypersensitivity. Each 38% SDF solution includes 24.4-28.8% silver and 5.0-5.9% fluoride, with a total of 55,800 ppm fluoride ion and 249,000 ppm silver ion, and a pH of 10.2. It is speculated that applying SDF to multiple teeth may increase the body’s fluoride concentration. The mode of action involves the release of fluoride and silver ions to minimise mineral loss [15].
Acid production is caused by the carbohydrate metabolism of bacteria. According to research, fluoride inhibits the carbohydrate metabolism of lactobacilli and oral streptococci, thereby reducing acid formation. Under low pH conditions, F- and H+ combine to form hydrofluoric acid, which diffuses into bacteria and dissociates into H+ and F-. This process increases H+ and F- concentrations inside bacteria while reducing H+ levels in saliva. Consequently, this increases acidity in the bacterial cytoplasm and interferes with enolase activity, leading to increased phosphoenolpyruvate production for glucose uptake. The fluoride content affects salivary pH, which may be related to a decrease in Streptococcus mutans and glucose metabolism [13].
Fluoride concentration in saliva is influenced by portable water intake and topical fluoride treatments, which are applied to prevent caries [14]. A study by Achmad H et al., showed significant differences in fluoride concentrations during three time frames, indicating that time differences significantly affect fluoride concentration. The maximum fluoride concentration was observed less than an hour after the application of topical fluoride and also an hour after SDF application; thereafter, the concentration returned to its starting point [16].
In present study, the comparison of mean salivary pH levels at different time intervals revealed an increase in pH levels, from 6.45 before the application of SDF to 6.95 immediately after and 7.30 after the application. The mean salivary pH levels continued to increase from before to the immediate and subsequent time intervals after the application of SDF, indicating that SDF plays a key role in reducing caries by increasing pH levels. This finding aligns with a previous study by Navami G et al., which measured plaque pH at various intervals after the application of SDF. In that study, it was observed that the plaque pH did not drop to an acidic level, likely due to the action of SDF supplementing the salivary buffering system [17].
Salman BN et al., conducted a study comparing the effects of fluoride varnish with SDF and NaF and found that after five minutes, the pH of both groups increased, resulting in decreased salivary acidity [5]. Sarkar A et al., and Setiawan S et al., demonstrated that there is a significant difference in salivary pH before and after tooth brushing with fluoridated toothpaste [13,18]. Apriani A et al., assessed the differences between fluoride varnish and Casein Phosphopeptide-Amorphous Calcium Phosphate (CPP-ACP) in decreasing salivary pH and concluded that an increased pH was observed after using varnish for one month, with no statistically significant difference between the two materials in terms of pH [19].
In present study, the comparison of mean differences between time intervals in the 3-4 and 5-6-year age groups revealed that salivary pH in the 3-4-year group was low before the time interval. However, after the application of SDF, the pH increased to higher values immediately and one hour post-application. Similarly, the salivary pH in the 5-6-year group also increased after the application of SDF, although this change was not statistically significant. Therefore, a higher mean pH was observed in younger individuals, but no statistical difference in pH was found between the different age groups. In contrast, a study conducted by Apriani A et al., on older individuals showed a higher salivary pH after one month of using fluoride varnish, although the results were not significant [19]. Additionally, the salivary pH of children aged 8-9 years increased after treatment with CPP-ACP, according to Anamaria B et al., [20].
In the present study, salivary pH in males before the time interval was lower, but after the application of SDF, it increased to higher values immediately and one hour post-application, although this change was not statistically significant. A higher mean pH was recorded in males than in females, but this difference was also not statistically significant. Currently, there are no studies comparing the salivary pH of children of different genders at various time intervals following the application of SDF. Studies by Patir A et al., and Percival RS et al., demonstrated that caries rates are higher in females than in males, with contributing risk factors including differences in salivary composition and flow rates, dietary habits, and specific variants of the Amelogenin X-linked (AMELX) gene [21,22]. Females tend to acquire their teeth at an earlier age than males, which results in longer exposure to the oral environment and bacteria, leading to increased susceptibility to caries [23]. This may explain why salivary pH is higher in males than in females.
In a comparison of the mean difference between time intervals with caries, children with caries ≤5 exhibited low salivary pH levels before the time interval. At immediate time intervals, the pH increased, and after the time interval, it reached even higher values. In contrast, children with caries >5 also had low pH levels before the time interval; however, immediately after application, the pH increased significantly, reaching its highest values after one hour of application. This suggests that as caries increase, the pH also rises immediately following the application of SDF, making the pH more alkaline and potentially reducing the incidence of caries.
A study by Chhabra N and Chhabra A demonstrated that combining SDF and Sodium Fluoride (NaF) leads to a significantly greater arrest of moderate lesions than using SDF or NaF alone, particularly in advanced lesions [24]. Additionally, Gao SS et al., reported that SDF was 80% effective in preventing new caries incidence in deciduous teeth and 65% effective in permanent first molars. This indicates that SDF could be useful in preventing and arresting caries across all teeth and surfaces [25].
The findings of present study revealed that salivary pH continued to increase after one hour of application, indicating an increase in fluoride concentration that contributes to caries prevention. Abdellatif EB et al., indicated that the maximal concentration of fluoride in saliva is reached in less than an hour after topical fluoride administration [10]. On the other hand, another study found that saliva fluoride content increased immediately following SDF treatment but subsequently returned to baseline levels after six hours [26]. This rise in fluoride concentration affects enamel remineralisation in the oral cavity [27]. Products that raise fluoride concentration enhance salivary fluoride bioavailability and remineralisation potential by releasing bioavailable fluoride ions from enamel surfaces, forming a layer of Calcium Fluoride (CaF2). This treatment is recommended for challenging carious lesions, dentin hypersensitivity, and patients at risk, using fluoride ions and silver particles to minimise mineral loss and prevent cariogenic biofilm development [12]. The saliva concentration following SDF treatment may be influenced by fluoride and silver ions that penetrate tooth enamel and dentin [8]. The application of SDF significantly increases pH levels, thereby assessing and preventing caries prevalence, making it an effective treatment for reducing caries activity.
Limitation(s)
The present study did not include a control group. A comparison of pH changes following the application of different fluoride varnishes could have been useful. Additionally, SDF causes a blackish discolouration of teeth, so an alternative varnish could have been considered. Further studies using a larger sample size, along with an estimation of the fluoride concentration and its effect on dental caries, would be beneficial.
Conclusion(s)
The study concluded that the application of SDF increases fluoride concentration in saliva, which can inhibit tooth demineralisation. A comparison of mean salivary pH levels at different time intervals revealed that the mean pH levels increased from before the application of SDF to one hour after the application. Males exhibited higher mean pH levels than females. The study also found that as the level of caries increased, the pH rose at both the immediate and post-application stages of SDF, making the pH alkaline and reducing caries incidence. Thus, SDF can be used as an effective treatment for raising pH and lowering caries activity, and it can both assess and reduce the risk of caries prevalence.
*Statistically significant
*Statistically significant