Comparative Evaluation of Serum Vitamin D and IL-1β in Patients with Oral Lichen Planus and Healthy Subjects: A Research Protocol
Hrishika Jawaharlal Chhattani1, Aarti Panchbhai2
1 Postgraduate Student, Department of Oral Medicine and Radiology, Sharad Pawar Dental College, Datta Meghe Institute of Higher Education and Research, Wardha, Maharashtra, India.
2 Professor, Department of Oral Medicine and Radiology, Sharad Pawar Dental College, Datta Meghe Institute of Higher Education and Research, Wardha, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Hrishika Jawaharlal Chhattani, Postgraduate Student, Department of Oral Medicine and Radiology, Sharad Pawar Dental College, Datta Meghe Institute of Higher Education and Research, Wardha-442107, Maharashtra, India.
E-mail: chhattanihrishika@gmail.com
Introduction
Oral Lichen Planus (OLP) is a chronic mucocutaneous immune-mediated disease that has been classified as a Potentially Malignant Disorder (PMD). The aetiology of OLP needs further exploration. Research indicates that the immune system plays a pivotal role in the progression of OLP.
Need of the study
Vitamin D regulates the suppression of Interferon-Gamma (IFN-γ) and Interleukin-1 beta (IL-1β) production within the epithelium and its insufficiency may play a role in the development of OLP.
Aim
To evaluate and compare the serum concentrations of IL-1β and Vitamin D in patients affected by OLP and in healthy subjects.
Materials and Methods
A case-control study will be conducted in the Department of Oral Medicine and Radiology at Sharad Pawar Dental College, Datta Meghe Institute of Higher Education and Research, located in Maharashtra, India, from August 2024 to August 2026. Patients who present to the Department of Oral Medicine and Radiology and express willingness to participate will be enrolled in the study. Each patient will undergo a comprehensive clinical examination and provide written consent after being informed about the study. A thorough intraoral clinical assessment of the lesions will be conducted. Once a patient is clinically diagnosed with OLP, serum sample collection will be performed. Similarly, healthy subjects who are willing to participate in the study will also undergo sample collection. The median cubital vein will be punctured to obtain 2.5 mL of blood under aseptic conditions. The electrochemiluminescence-binding assay will then be conducted to quantify the total amounts of 25-hydroxy vitamin D and Interleukin-1 beta. After sample collection, patients with OLP will be educated and counseled regarding the treatment of OLP and habit cessation. Statistical analysis will be performed using an unpaired t-test, with a p-value considered significant at a 5% level of significance.
25-hydroxy vitamin D, Interleukin-1 beta, Mucocutaneous lesion, Serum biomarkers
Introduction
The Latin term planus, meaning flat and the Greek word lichen, which means tree moss, are the origins of the name LP. In 1869, Wilson E introduced LP as a chronic condition that affects the skin, scalp, nails and mucous membranes, with the potential for occasional advancement towards malignancy [1]. OLP is a chronic mucocutaneous immune-mediated disease that has been classified as a PMD [2].
The OLP is most commonly found in middle-aged individuals and is typically diagnosed in patients in their mid-fifties. The occurrence is more common in females compared to males, with a ratio of one male for every three females [2]. The clinical appearance of OLP can vary throughout life, with more severe variants observed as age progresses [3]. Globally, the prevalence of OLP among the general adult population is estimated to range from 0.5% to 2% [4].
The aetiology of OLP is still under investigation. Research over the years has indicated that the immune system plays a significant role in the development of OLP. This hypothesis is supported by histopathological findings such as liquefactive degeneration, T-lymphocytes infiltration into the sub-epithelial band and basal cell obliteration. These features can be understood as the emergence of immune system cell-mediated pathways, which play a role in the pathogenesis of OLP through the direct toxicity of T-lymphocytes in response to antigens exposed by the basal cell layer [5].
Vitamin D has been observed to regulate the activity of T-lymphocytes. By directly influencing CD4 cells, it inhibits the growth of Th1 cells and accelerates the generation of T helper 2 (Th2) cells [2]. In the initial progression of OLP, T-lymphocytes may play an important role as these cells are often unable to differentiate between the body’s innate molecules and foreign antigens. Autoimmune T cell activation is a process that may transmit from the mucous membrane of the oral cavity to other areas of the body and might occur simultaneously with the initiation of mucosal lesions [5]. Evidence suggests that a lack of vitamin D may contribute to the development of OLP by limiting the production of IFN-γ and IL-1β within the epithelium [6].
The study aims to evaluate and compare the serum concentrations of Vitamin D and IL-1β, in patients with OLP and healthy subjects.
Primary objectives:
To evaluate the concentration of serum Vitamin D and serum interleukin-1 beta in OLP patients with OLP.
To evaluate the concentration of serum Vitamin D and serum interleukin-1 beta levels in healthy subjects.
Secondary objectives:
To compare the concentrations of serum interleukin-1 beta and Vitamin D in both study groups.
To find the association between serum levels of serum Vitamin D and interleukin-1 beta in patients with OLP.
Null hypothesis: There will be no significant difference in the levels of serum Vitamin D and IL-1 beta between patients with OLP and healthy subjects.
Alternate hypothesis: There will be a significant difference in the levels of serum Vitamin D and IL-1 beta between patients with OLP and healthy subjects.
Review of Literature
In recent times, a significant amount of research investigating the role of vitamin D in the prevention of OLP has been conducted [2,5,6]. According to a study by Pawar V et al., vitamin D3 deficiency was found to be more prevalent in OLP cases than in the control group [2]. Bahramian A et al., conducted a comparative study to evaluate serum vitamin D levels in patients with OLP and healthy subjects, concluding that the serum vitamin D levels in patients with OLP were comparatively lower than those in healthy subjects [5]. Similarly, Gupta A et al., estimated serum vitamin D levels in OLP patients in the North Indian population and found that the mean difference in serum vitamin D levels between affected cases and the control group was statistically significant [7].
In a systematic review on the role of vitamin D and its receptor in OLP, it was determined that a lack of vitamin D could be linked to a heightened susceptibility to OLP lesions [6]. In another systematic review and meta-analysis on serum vitamin D levels in patients with OLP conducted by Sakthivel S et al., it was concluded that the meta-analysis showed numerically lower vitamin D levels in OLP patients, although this finding was statistically non significant [8]. Eslami H et al., conducted a study to investigate the relationship between Interleukin-8 (IL-8) and Interleukin-1β (IL-1β) levels and disease activity in patients suffering from OLP, observing high levels of IL-1β and IL-8 in OLP patients [9].
Materials and Methods
A case-control study will be conducted in the Department of Oral Medicine and Radiology at Sharad Pawar Dental College, Datta Meghe Institute of Higher Education and Research, Maharashtra, India, from August 2024 to August 2026. The study will be conducted after obtaining informed consent from the participants. Institutional Ethical Clearance (IEC) has been obtained prior to the study (DMIHER(DU)/IEC/2024/223).
Inclusion criteria:
The patient reporting to the Department of Oral Medicine and Radiology, and willing to participate in the study will be included in the study.
Subjects above 21 years of age who are affected with OLP and healthy controls who are willing to participate in the study.
Exclusion criteria:
Patients on Vitamin D supplements;
Patients with lichenoid lesions, due to the usage of any drug;
Patients with fibro-osseous disorders;
Patients with disorders of bone metabolism or if patients are a known cases of any systemic disorders.
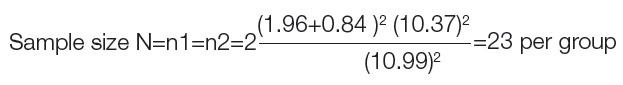
Sample size calculation: Formula using Mean Difference:

Zα=1.96 considering CI at 95%,
Zβ=0.84=Power at 80%,
Primary variable: Vitamin D level, Vitamin D level OLP group=15.11±2.45, Vitamin D level control group=26.1±18.29 [2], Mean difference δ=10.99, Pooled std dev=10.37
Minimum sample size required;
Study Procedure
Once every patient has given their informed written consent, their demographic information (age, sex, address, occupation) will be recorded and a comprehensive clinical examination, along with a detailed medical history, will be conducted for each individual. A thorough intraoral examination of the lesion will be performed. Once the patient is clinically diagnosed with OLP, the patient will undergo serum sample collection. Similarly, healthy subjects willing to participate in the study will also have their samples collected. The median cubital vein will be venipunctured to obtain 2.5 mL of blood under aseptic conditions. The blood sample will then be centrifuged to separate the serum. Following this, an electrochemiluminescence-binding assay will be conducted to quantify the total amounts of 25-hydroxy vitamin D and interleukin-1 beta. After sample collection, patients with OLP will be educated and counseled regarding the treatment of OLP and the importance of habit cessation.
Outcomes: Estimation of the concentration of serum vitamin D and interleukin-1 beta using the electrochemiluminescence technique.
Statistical Analysis
Statistical Package for the Social Sciences (SPSS) software version 27.0 will be used for statistical analysis. This case-control study will analyse the association between Vitamin D (deficiency or sufficiency) and IL-1β (normal or excess) among cases (patients with OLP) using Chi-square analysis. The quantitative assessment of Vitamin D (ng/mL) and IL-1β (pg/mL) levels will be analysed using an unpaired t-test. The level of significance will be set at 5% (p≤0.05).
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: May 20, 2024
Manual Googling: Jun 26, 2024
iThenticate Software: Aug 16, 2024 (19%)
[1]. Wilson E, On lichen planusJ Cutan Med Dis Skin 1869 3:117-32. [Google Scholar]
[2]. Pawar V, Krishna S, Deepak T, Prarthana G, Vyavahare S, Jujare R, Association of vitamin D serum concentration and oral lichen planus: A randomized controlled clinical trialJ Indian Acad Oral Med Radiol 2022 34(4):414-17. [Google Scholar]
[3]. Manandhar S, Prasanth T, Satisha TS, Gupta N, Kumar P, Comparative evaluation of the management of oral lichen planus using three different modalities: A clinical studyIJPI 2022 7(3):113-21. [Google Scholar]
[4]. Li C, Tang X, Zheng X, Ge S, Wen H, Lin X, Global prevalence and incidence estimates of oral lichen planus: A systematic review and meta-analysisJAMA Dermatol 2020 156(2):172-81.PMCID: PMC699067010.1001/jamadermatol.2019.379731895418 [Google Scholar] [CrossRef] [PubMed]
[5]. Bahramian A, Bahramian M, Mehdipour M, Falsafi P, Khodadadi S, Dabaghi Tabriz F, Comparing Vitamin D serum levels in patients with oral lichen planus and healthy subjectsJ Dent (Shiraz) 2018 19(3):212-16. [Google Scholar]
[6]. Motahari P, Pournaghi Azar F, Rasi A, Role of Vitamin D and Vitamin D receptor in oral lichen planus: A systematic reviewEthiop J Health Sci 2020 30(4):615-22.10.4314/ejhs.v30i4.17 [Google Scholar] [CrossRef]
[7]. Gupta A, Sasankoti Mohan RP, Kamarthi N, Malik S, Goel S, Gupta S, Serum Vitamin D level in oral lichen planus patients of North India- A case-control studyJournal of Dermatologic Research and Therapy 2017 1(2):19-35. [Google Scholar]
[8]. Sakthivel S, Gunasekaran S, Castelino RL, Babu GS, Ajila V, Buch SA, Serum vitamin D levels in patients with oral lichen planus: A systematic review and meta-analysisGulhane Med J 2021 63(4):267-73. [Google Scholar]
[9]. Eslami H, Pakdel F, Babaloo Z, Pouralibaba F, Falsafi P, Neghad SK, Evaluation of serum IL-1B and IL-8 in patients with Oral Lichen PlanusInt J Clin Dent 2016 9(4):241-45. [Google Scholar]