Snake bite is a common medical emergency and an occupational hazard, more so in tropical India, where farming is a major source of employment.
Over 2,000 species of snakes are known worldwide, of which around 400 are poisonous. These snakes belong to the families Elapidae, Viperidae, Hydrophiidae and Colubridae [1]. Viper bites are more common than other poisonous snakebites in human beings [2,3]. Of the different varieties of vipers, the Russell’s viper (Vipera russelli) commonly inhabits the Southern Asian countries, and the Russell’s viper’s bite is regarded as an occupational hazard for the farming community.
Every year, 50,000 Indians die in 2, 50,000 incidents of snake bite, despite the fact that India is not home for the largest number of venomous snakes in the world, nor is there a shortage of anti –snake venom in the country [4].
The main cause of this “unacceptable incidence” of snake bite fatalities is that people try out all kinds of “bizarre remedies” initially, instead of going to the nearest hospital. The available data on the epidemiology of snakebite from the Indian subcontinent are sparse, because most of the snake bites occur in illiterate, rural people who use witchcraft and traditional healers. Only the cases of snakebite with severe envenomation reach the healthcare centres.
This study was carried out to describe the epidemiology, arrival delays, clinical features, complications, and the outcome of snakebites which were seen in a tertiary care hospital of Southern India.
MATERIALS AND METHODS
This record based, retrospective, descriptive study was carried out at the Sri Chamarajendra District Hospital which was attached to the Hassan Institute of Medical Sciences, Hassan, Karnataka, India. This institute is a referral government hospital in Southern Karnataka, India, where patients come from the districts of Hassan, Coorg, and Chikkamangaluru.
The records of the snakebite victims who attended the hospital from January 2010 to December 2011 were obtained from the medical records department. This department uses the ICD-10 system for the classification of diseases.
The data on the demographic factors, clinical features and complications, details of the treatment which was received and the outcome of the snake bite victims were recorded. The mortality was defined at necropsy and on the basis of the death certificates. The statistical analysis was conducted by using the Statistical Package for the Social Sciences, version 11.0 (SPSS Inc, Chicago, IL, USA).
RESULTS
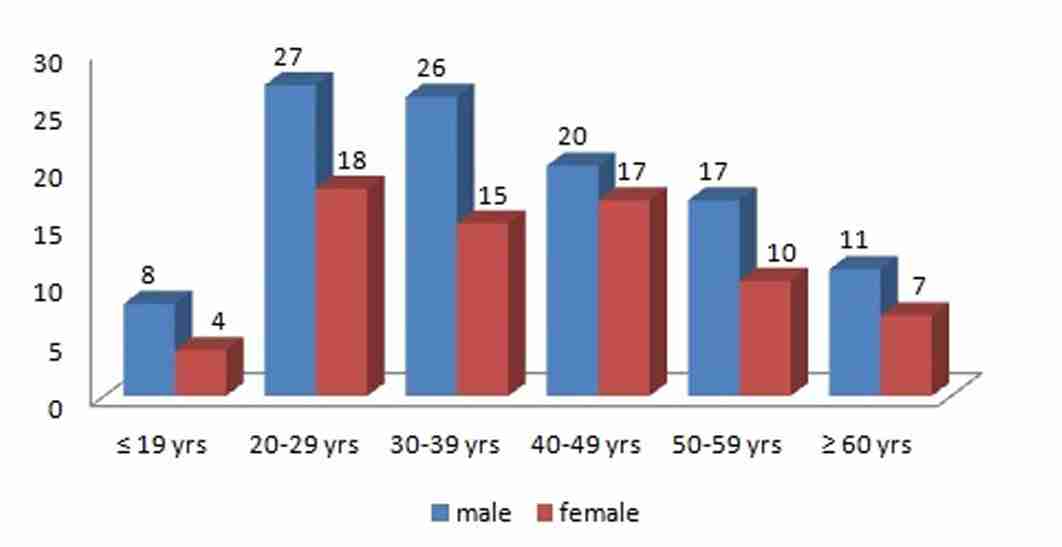
A total of 180 cases of venomous snakebite cases were included in this study, who had reported to the hospital from January 2010 to December 2011. In this study sample, a majority of snake bite victims were aged between 20-40 years. The decade wise distribution of the male and the female snake bite cases has been shown in [Table/Fig-1]. The mean age of the male victims was 36.6 years (range 15-68 years) and that of the female victims was 44.2 years (range 17-62 years).
Graph shows age distribution of snake bite victims.
The detailed demographic profiles of the snake bite victims have been presented in [Table/Fig-2]. Most of the cases were males (60.55%) and the male to female ratio was 1.5:1. A majority of the patients were farmers (54.4%) and plantation workers (30.5%). In our study, 41 patients (27.22%) were illiterates. The biting species was identified only in 98 cases and the commonest species was Russell’s viper (58 cases), followed by cobra (25 cases) and common Krait (15 cases).
Demographic factors of snake bite victims
| Factors | Number of patients (%) |
| Gender distribution |
| Male | 109 (60.55%) |
| Female | 71 (39.45%) |
| Occupation |
| Farmers | 98(54.44%) |
| Plantation workers | 55(30.55%) |
| House wife | 08(4.44%) |
| Others | 19(10.55%) |
| Educational Status |
| Illiterate | 41(27.22%) |
| 1-4 th standard | 74(41.11%) |
| 5-10th standard | 27(15%) |
| >10th standard | 38(21.11%) |
| Type of snake identified |
| Unidentified | 82 |
| Russell viper | 58 |
| Cobra | 25 |
| Common krait | 15 |
| Location at time of bite |
| Outdoor | 149(82.77%) |
| Indoor | 31(17.22%) |
| Diurnal variation |
| Day | 127(70.55%) |
| Night | 53(29.45%) |
| Seasonal variation |
| March-June | 34(18.88%) |
| July-September | 97(53.88%) |
| October-December | 48(26.6%) |
| Site of bite |
| Lower extremity | 121(67.22%) |
| Upper extremity | 43(23.88%) |
| Head and face | 04(2.22%) |
| Trunk | 05(2.7%) |
| Multiple sites | 07(3.88%) |
| Place of bite |
| Rural | 146(81.11%) |
| Urban | 34(18.88%) |
| Fang marks |
| Single | 32(17.77%) |
| Double1 | 22(67.77%) |
| >2 | 16(8.88%) |
| Scratches | 10(5.5%) |
The peak incidence in the snake bite cases occurred during the months of July to September. Most of the victims in our study were bitten outdoors (n=149, 82.7%), mostly in the field during the day time (70.5%). The most frequently bitten site was the lower extremity (67.22%). A majority of the snake bite victims were from the rural areas, with a rural to urban ratio of 4.2:1.
Definitive fang marks were seen in 94.5% of the cases, double punctured fang marks were observed in a majority of the cases (67.7%) and in 10 cases, scratch marks were present at the site of the bite. Only 17.2% of the snake bite victims could come to the hospital within one hour of the bite [Table/Fig-3].
Time delay between snake bite and hospital admission
| Time of delay |
| <1 hour | 31(17.22%) |
| 1-6 hour | 79(43.88%) |
| 6-24 hour | 49(27.22%) |
| 1-3 days | 13(7.22%) |
| >3days | 08(4.44%) |
| Cause of delay in patients arrived > 6 |
| hrs of bite(n=70) |
| Poor transportation facility | 30 |
| Traditional healer | 18 |
| No sense of danger | 14 |
| Patients ignorance | 08 |
First aid measures were employed in a majority of the patients (n=150, 83.4%), while the other 30 victims did not receive any first aid treatment [Table/Fig-4].
First aid received prior to hospitalization
| Tourniquet | 91(50.55%) |
| Incision | 24(13.33%) |
| Application of herbal medicine | 19(10.55%) |
| Suction of the venom from the bite site | 08(4.44%) |
| Application of snake stone | 08(4.44%) |
| No first aid | 30(16.66%) |
Neuroparalytic features which are a hallmark of cobra and krait bites, were seen in 72 cases (40%) and the haematotoxic manifestations were attributable to viper bites in 108 cases (60%) [Table/ Fig-5]. At our hospital, all the venomous snake bite victims received the equine polyvalent Anti-Snake Venom (ASV). The mean dose of ASV which was given for the neuroparalytic snake bites was 16.2 vials (range 10-32 vials) and 21 vials (range 10-40) were given for the viper bites.
Clinical features of snake bite victims
| Local manifestations of snake bites. |
| Pain and tenderness | 106 |
| Swelling | 106 |
| Local rise of temperature | 106 |
| Blisters | 32 |
| Local lymphadenopathy | 24 |
| Discoloration | 18 |
| Ulceration | 12 |
| Haematotoxic manifestations in 108 cases of viper bite. |
| Bleeding from the Site of the bite | 71(65.7%) |
| cellulitis | 64(59.2%) |
| Haematuria | 34 (31.4%) |
| Ecchymosis | 31(28.7%) |
| Epistaxis | 18(16.6%) |
| Gastrointestinal bleeding | 16(14.8%) |
| Haemoptysis | 12(11.1%) |
| Intracranial bleeding | 02(1.8%) |
| Clinical features of neuroparalytic snake bites in 72 cases. |
| Ptosis | 70(97.2%) |
| Ophthalmoplegia | 54(75.0%) |
| Bulbar weakness | 40(55.5%) |
| Respiratory paralysis | 28(38.8%) |
| Paralysis of limbs | 14(19.4%) |
| Loss of consciousness | 12(16.6%) |
Allergic reactions to ASV were noted in 23 (12.7%) cases (anaphylaxis in 4 cases, pyrexial reaction in10 cases, and urticarial reactions in 9 cases). A supportive treatment with the blood component therapy was given in 26 cases.
Complications of snake bite were shown in [Table/Fig-6].
Complications observed following hospitalization
| Respiratory failure | 28(15.5%) |
| Acute renal failure | 26(14.4%) |
| Gangrene at the bite area | 06(3.3%) |
| DIC | 04(2.2%) |
| ARDS | 03(1.6%) |
| Intracerebral haemorrhage | 02(1.1%) |
Among the 72 cases with neuroparalysis, 28 cases developed respiratory failure and they required assisted ventilation. With the ASV and ventilator support, all the patients recovered completely without any fatal outcome. Of the 108 cases with viper bites, 26 patients developed acute renal failure and of these, 15 patients required dialysis.
The mean duration of the hospital stay was 6 days (range 1-23 days). The incidence of the complications like acute renal failure, gangrene at the bite area, DIC and ARDS were more in the subgroup of patients who presented to the hospital after a delay of > 6 hours. No fatal outcome was reported in the victims who were admitted within 24 hours of the snake bite, thus suggesting the importance of an early specific treatment.
Seven patients died, due to acute respiratory distress syndrome (ARDS-3 cases), disseminated intravascular coagulation (DIC-2 cases), and intracerebral haemorrhage (2 cases), thus giving a mortality rate of 3.8%.
DISCUSSION
In India, the poisonous snakes belong to the elapid family of the cobra and krait and to the viper family of the Russell’s viper and the saw scaled viper. The envenomation which is attributable to the elapid bites causes paralysis of the ocular, bulbar, and the limb girdle muscles. The viper bites mainly cause bleeding from the mucocutaneous sites, haemolysis, acute renal failure, and occasionally, shock [5]. With regards to the viper bites which were reported in our study, our findings support the view that saw-scaled vipers do not seem to inhabit the Southern part of India [6].
Males are affected more often than the females, as they constitute the working majority who are actively engaged in farming and other outdoor activities. Our findings concurred with those of earlier studies [2,3,7,8]. In India, men are the dominant earning members of the family, working outdoors and sleeping in the farmyards during harvesting. This could probably be the main cause of the male preponderance which was seen in our study.
In our study, predominantly the younger population was involved (20-40 years of age), probably due to their more ambulant nature . A majority of the victims were from the rural areas (81.1%) and our findings concurred with those of earlier studies [6,9–12].
Snake bite may be termed as an occupational disease, as farmers, plantation workers, herdsmen, hunters or workers on the development sites are mostly affected [13]. Farmers are more prone to accidental contacts with snakes while they work in the field barefooted [6,14].
Most of the human snakebites occur during the monsoon season, because of the flooding of the habitats of the snakes and their prey. It is the life cycle of the natural prey of these reptiles that govern their contact with humans. The breeding habits of frogs closely follow the monsoons and rats and mice are always in close proximity to human dwellings. In our study, there was a higher incidence of snakebites during the monsoon season (July to September). In another Southern Indian study, snakebites were found to abound during the months from May to July (67%) and from October to December (33%) [15].
In our study, most of the victims were bitten outdoors (82.7%), mostly in the fields during the day time (70.5%) and on the lower limbs (67.2%). A similar observation was reported in other studies also [3,14,15].
We noticed that 27.2% of the snake bite victims were illiterates and that 47.1% were educated below the primary school, which was comparable to the findings of a study which was done in Nepal [16]. The morbidity and the mortality were more in illiterates because of their ignorance regarding the importance of an early medical attention and wasting precious time by consulting traditional healers.
We noticed that 38.8% of the patients had reached hospital after a delay of 6 hours. This delay in their arrival could be attributed to the poor transportation facility, lack of awareness of the hazards of snakebite, an unrelenting belief in the traditional system of medicines and the patients’ ignorance, which had contributed to a substantial increase in the morbidity and the mortality.
In our study, 83.4% of the patients had received first aid treatment for the bitten site that is, tourniquet, incision and drainage, suction, and indigenous herbal medicines. These practices are not currently recommended in the treatment of snake envenomations, as they do more harm than good and as they delay the transport of the victims to a medical facility [17]. The use of tourniquets, which can increase the local complications by increasing the tissue anoxia and by triggering severe systemic envenoming right after their removal, has currently been strongly discouraged by most of the experts.
Most of the snakebites in our study were haematotoxic (60%), followed by neuroparalytic (40%) ones. Among the haematotoxic snake bites, bleeding from the site of the bite was the main manifestation, followed by cellulitis, haematuria and ecchymosis, which were similar to that which were observed in studies which were done in Maharashtra [14]. However, the studies which were conducted in Jammu [7] and Orissa [18] found haematuria to be the most common manifestation. This difference in the haemorrhagic manifestations in the different studies is attributed to the subtle differences among the venoms of the viperine subspecies in different regions [19].
The neuroparalytic symptoms which were seen, in the descending order, were ptosis, ophthalmoplegia, bulbar weakness, respiratory muscle involvement, and limb weakness. The reported incidences of the neurological symptoms in 2 Sri Lankan studies on neuroparalytic snakebites were ,ptosis in 70%–85% cases, respiratory muscle weakness in 18%–45% cases, ophthalmoplegia in 53%-75% cases, and limb weakness in 27%–54% cases respectively [20,21].
In our study, the most common complication was respiratory paralysis, followed by acute renal failure, gangrene at the bite area and DIC. We noticed that 14.4% of the patients had developed ARF, whereas Saini et al., [22] had reported that only 4% of the cases in their study (adults with snake bites) had developed it.
ASV is the only effective and specific treatment which is available for snakebite envenomation. The anti-snake venoms may be species specific (monovalent/monospecific) or they may be effective against several species (polyvalent/polyspecific). As per the recommendations of the WHO, the most effective treatment for snake bite is the administration of monospecific ASV; however , this therapy is not always available for the snakebite victims because of its high cost, the frequent lack of its availability, and the difficulty in correctly identifying the snake. As snakes inject the same amount of venom into children and adults, children should also receive the same dose of antivenom as the adults [23].
A proportion of the patients, usually more than 10%, develop a reaction either early (within a few hours) or late (five days or more) after being given the antivenom. The risk of the reactions is doserelated, except in rare cases in which there had been sensitization (IgE-mediated Type I hypersensitivity) by a previous exposure to the animal serum, for example, to the equine antivenom, the tetanus-immune globulin or the rabies-immune globulin. In our study, we noticed that 12.7% of the patients had developed allergic reactions to ASV. The incorrect assessment of the risk versus benefit can lead to the unnecessary use of antivenom in patients with milder or even no envenoming, and in those who are bitten by snakes, whose venoms are not neutralized by the available antivenoms [24].
The mortality rate in our study was 3.8%. A 3%–10% variation in the mortality rates which were caused by snakebites was reported in various studies which were conducted by Kulkarni ML, Sharma SK, Suchitra N, Ahmed SM [25], IF Inamdar [26] and Hati AK [Table/Fig-7]. The high mortality rate in India has been attributed to the geographical factors and a predominantly rural population that was dependent on agriculture as an occupation.
Comparison of mortality rate in various studies.
| Serial Number | Author | Year Published | Number of Cases | Died Number | Mortality Rate |
| 1 | Ahmed SM 25 | 2012 | 59 | 03 | 5.1% |
| 2 | I F Inamdar 26 | 2010 | 5 639 | 307 | 5.44% |
| 3 | Suchitra N 12 | 2008 | 200 | 06 | 3% |
| 4 | Punde DP 6 | 2005 | 427 | 20 | 4.7 % |
| 5 | Sharma SK 11 | 2004 | 66 | 02 | 3% |
| 6 | Kulkarni ML15 | 1994 | 633 | 33 | 5.2% |
| 7 | Hati AK 9 | 1992 | 307 | 31 | 10.1% |
STUDY LIMITATIONS
a) A retrospective analysis was one of the limitations of this study, since some of the important data were incomplete or insufficient and they may not reflect the exact statistics.
b) In the developing countries, most of the patients consult a traditional healer first instead of seeking treatment at the health centers. Many snakebite cases are treated at the primary healthcare centers and they were not referred to the higher centers, thus leading to an underestimation of the morbidity status in the studies which were done at the tertiary healthcare centers.
CONCLUSION
Snake bite in the tropics is a rural and an occupational hazard of farmers, plantation workers, herders and hunters. The available data on the epidemiology of snake bite in the Indian subcontinent are sparse.
Most of the traditional methods for the first aid treatment of snake bite have been found to result in more harm than good. The immobilization and the prompt transport of the snake bite victims to the hospital, along with the prompt administration of ASV, remains the mainstay to reduce the morbidity and the mortality which are associated with snake bites.
There is an urgent need to educate the rural population about the hazards and the treatment of snake bite.