Patients approach doctors with complaints and with the belief that they would be relieved of all their problems. It is a doctor’s responsibility to hear all the complaints patiently, to examine the patients, to diagnose the causes of their problems, to formulate treatment goals and to decide as to which drugs should be used, before writing any prescription. Communicating with the patients is an art and writing a prescription is a science. Many factors may affect the prescribing practice, which may lead to an irrational drug use like-pressure from the patients [1], pressure from the pharmaceutical industry [2], knowledge of the doctor, availability of unbiased information [3], etc. The impact of the irrational drug use is manyfold- it reduces the quality of the care and it increases the risk of the adverse drug effects, in addition to the waste of resources.
The World Health Organization (WHO) has formulated core drug use indicators to broadly measure the drug use in health facilities, that would describe the drug use pattern and the prescribing behaviour of the health care providers. In addition to the core indicators, a set of complimentary indicators have been defined. One of the complimentary indicators which can be used for Pharmacology Section Shirish Gajanan Beri, Vijaya Anil Pandit, Kapil Shatrughn Khade, Kushal Dilip Sardameasuring the quality of care is “Prescription in accordance with the treatment guidelines” [4]. Though its use is difficult, it is very important for measuring the irrational use of drugs.
Many studies have been carried out to measure the pattern of drug use in specified health facilities, e.g. govt. dispensaries, primary health centres, tertiary health care centres, etc. Not many studies have been carried out to measure the drug use pattern in the general practice. Most of the common ailments are managed by General Practitioners (GPs). The GPs prescribe a major bulk of the drugs which are sold in the market. Naturally, an irrational use of drugs at this level could lead to disastrous consequences.
Very few studies have been carried out to investigate the pattern of drug use in specific clinical conditions [5]. Fever is the most common complaint with which patients present to the general practitioners. It is an elevation of the body temperature that exceeds the daily variation. It is one of the most common symptoms of many illnesses. The patients who suffer from acute fever i.e. fever of less than 2 weeks duration, are usually treated by General Practitioners (GPs). The routine use of antipyretics which are given automatically in all cases of fever, not only masks the fever but also other important clinical indicators, giving a lead to the diagnosis. Therefore, too much aggressive treatment of acute fever leads to misuse of antipyretics. The story of the use of antibiotics, antimalarials, etc is similar.
The GPs in Pune city have Bachelor of Medicine and Bachelor of Surgery (MBBS), Bachelor of Ayurvedic Medicine and Surgery (BAMS), Bachelor of Homeopathic Medicine and Surgery (BHMS) and other qualifications, but MBBS and BAMS dominate the scene. So, the present work was undertaken to study the pattern of drug use and the appropriateness of the treatment in cases of acute fever by the GPs in Pune city, India who had MBBS and BAMS qualifications.
To describe the pattern of drug use in acute fever by the allopathic and ayurvedic general practitioners of the private sector dispensaries in Pune city.
MATERIAL AND METHODS
This was a prospective, cross-sectional and a comparative study which was done to evaluate the WHO Prescribing Core Drug Use (PCDU) indicators and the complimentary drug use indicators among the GPs of the private sector dispensaries in Pune city.
Selection of the Practitioners
A list of the GPs in Pune city, who were registered with the Indian Medical Association, Pune Branch, was obtained. MBBS and BAMS graduates compose more than 80% of the GPs in Pune city. So, the doctors of these two specialties were selected.
Pune city was divided into five zones – north, south, east, west and central zone. The MBBS and the BAMS practitioners were divided zone wise. Two practitioners of both the specialties from each zone were selected randomly. This gave us ten MBBS and ten BAMS practitioners who were spread over Pune city.
Informed Consent: The selected GPs were approached and they were explained in detail about the purpose of the study, the method of conduct and the analysis of the study. They were explained that their identities would not be revealed and that the data would be used for research purposes only. As a proof of their willingness to participate in the study, an informed consent was obtained from them. If any practitioner refused to participate, another one was selected randomly from the practitioners list.
Data Collection
A questionnaire was designed to collect the data of the drug use in acute fever. This was similar to a case sheet [6]. It also included a detailed indicators encounter form which was developed by WHO (Ref- How to investigate drug use). The case sheet included the patient’s demographic details (the name of the patient was optional), the presenting complaints of the patient, the findings on examination and the provisional diagnosis. (Annexure I). The details of the drug which was prescribed and dispensed on the first visit- was obtained.
Patient Selection
Inclusion criteria-
The patients of either sex, of any age, with fever of less than 2 weeks duration.
Exclusion criteria
A history of recurrent attacks of acute fever
The patients with a history of Human Immunodeficiency Virus infection (HIV)/ Acquired Immunodeficiency Syndrome (AIDS) and the use of drugs- corticosteroids or anticancer agents.
The Number of Patients
The data was collected from 20 patients per prescriber. So, the data of 400 encounters was collected.
The indicators which were studied:
1. The WHO Core drug use indicators – Prescribing indicators
The average number of drugs per encounter.
The percentage of the drugs which were prescribed by their generic names.
The percentage of the encounters with an antibiotic which was prescribed.
The percentage of the encounters with an injection which was prescribed.
The percentage of the drugs from an Essential Drug List (EDL) or a Formulary
For the Generics and Essential drug list, the WHO’s and the Indian Essential Drug List were considered as the standards.
2. The complimentary drug use indicators-
Prescription in accordance with the treatment guidelines
For the appropriateness of the treatment- The guidelines which were laid down in the Current Medical Diagnosis and Treatment (CMDT) and the Principles of Internal Medicine by Harrison, were considered as the standard.
Ethics: This study was approved by the Institutional Ethics Committee (IEC)
Statistical Analysis: The data was entered on an Excel sheet. Separate sheets were prepared for the MBBS and the BAMS practitioners.
The patients of the individual practitioners were grouped and arranged serially. All the drugs and their details like their doses and durations of use were coded and entered. The details of each patient were entered in one row and the columns indicated the diagnosis and the details of all the drugs which were prescribed.
The data was analyzed in detail about the use of various Antimicrobial Agents (AMAs), Nonsteroidal Anti-inflammatory Drugs (NSAIDs), gastric acid reducing agents, antihistaminics, etc by using the Statistical Package for the Social Sciences (SPSS), version 10. The drug use of the MBBS and the BAMS practitioners was compared.
RESULTS
The distribution of the encounters, age wise as well as sex wise, from both the groups of the GPs was comparable. Viral fevers and respiratory infections were the most common infections in the general practice. Then, Urinary Tract Infection (UTI) and gastroenteritis each contributed to only 5% of the infections. Skin and Soft Tissue Infections (SSTI) in the form of boils and cellulitis were seen by the MBBS GPs only. The other infections included malaria, chickenpox and mumps.
The WHO Core Drug use Prescribing Indicators
The average no. of drugs which was prescribed was 2.45 per patient for the MBBS GPs and it 4.5 per patient for the BAMS GPs. The difference was highly significant.
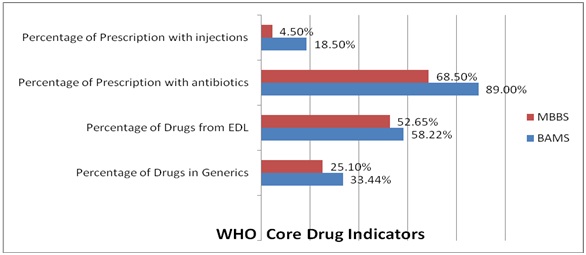
The core drug indicators of the MBBS and the BAMS GPs [Table/Fig-1] were compared. A highly significant difference was observed in the percentage of the prescriptions with AMAs and in the percentage of the prescriptions with injections (p=0). The other parameters i.e. the percentage of drugs in generics and from EDL were comparable among both the practitioners i.e. the difference was not statistically significant.
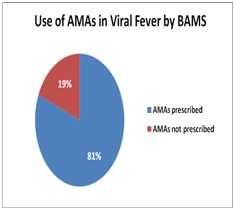
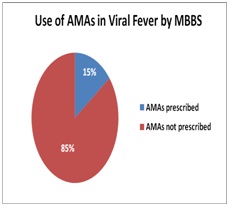
As can be seen from the above figures [Table/Fig-2 and 3], for treating viral fevers, the BAMS doctors used AMAs in 81% patients and only about 19% of the patients were not given any AMAs. More than 85% of the patients with viral fever were treated without prescribing AMAs, by the MBBS GPs. This difference was highly significant (p<0).
Use of AMAs in viral fever by BAMS
Use of AMAs in viral fever by MBBS
Antimicrobial agents (AMAs)
The β-lactam antibiotics, quinolones and macrolides were the important groups of AMAs which were used in the treatment of fever. From [Table/-Fig-4 and 5], it is evident that amongst the β-lactams, penicillins were used mostly by the MBBS GPs, as against cephalosporins which were more frequently used by the BAMS GPs. This difference was highly significant statistically (p<0.008 and p=0 respectively). The use of macrolides and fluoroquinolones was comparable in both the groups. The other AMAs included tetracyclines, antivirals, aminoglycosides, etc.
Use of AMAs Diagnosis wise by BAMS doctors
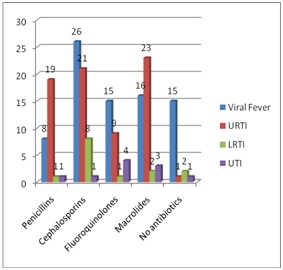
Use of AMAs Diagnosis wise by MBBS doctors

Inappropriate use of AMAs
The inappropriateness of the use of AMAs was decided as per the following criteria
Improper selection of the AMAs
Wrong dose
Wrong duration
By applying the above criteria, the inappropriateness of the AMAs was studied [75.7% of the BAMS prescriptions and 32.14% of the MBBS prescriptions were inappropriate for AMAs].
Injectable Antimicrobial Agents
All the prescriptions which were made by the BAMS GPs on injectable AMAs were inappropriate for their doses, as against only 33% of the injectable AMAs which were prescribed by the MBBS GPs. The fact was that only a single injectable AMA was given, which was not followed later. The whole issue of the injectable AMAs, especially in the outdoor practice, is irrational.
About 25% of the BAMS and the MBBS GPs had prescribed Paracetamol alone [Table/Fig-6]. Nimesulide and Paracetamol was the favoured combination of the BAMS GPS as compared to that of the MBBS GPs and the difference was highly significant (p=0). The MBBS GPs preferred the Ibuprofen and paracetamol combination. No NSAIDs were significantly used in 17 and 6 patients by the MBBS and the BAMS GPs respectively (p< 0.05).
Use of Non steroidal anti-inflammatory drugs in patients of acute fever
NS-Not significant HS-Highly significant S-Significant
| Drugs | BAMS | MBBS | z-value | p-value | Significance |
|---|
| Paracetamol | 46 | 52 | 0.69 | 0.24 | NS |
| Nimesulide | 3 | 7 | 1.28 | 0.09 | NS |
| Nimesulide + Paracetamol | 48 | 19 | 3.95 | 0 | HS |
| Ibuprofen | 5 | 1 | 1.65 | 0.04 | S |
| Paracetamol + Ibuprofen | 30 | 41 | 1.44 | 0.07 | NS |
| No NSAIDs | 6 | 17 | 2.15 | 0.05 | S |
The first generation antihistaminics, diphenhydramine and chlorpheniramine were used more by the BAMS GPs (p< 0.001), whereas the second generation antihistaminics, cetirizine and levocetirizine were used more by the MBBS GPs (p< 0.0001) [Table/Fig-7]. The BAMS doctors used antihistaminics mainly for viral fevers and Upper Respiratory Tract Infections (URTIs), whereas the MBBS doctors used them mainly for URTIs and for a few patients of viral fever. No antihistaminic was used by more number of MBBS than the BAMS practitioners and the difference was highly significant (p=0).
Use of Antihistaminics in patients of acute fever
| H1 antihistaminics | BAMS | MBBS | z-value | p-value | Significance |
|---|
| Diphenhydramine | 8 | 0 | 2.88 | 0.001 | HS |
| Chlorpheniramine maleate | 66 | 12 | 7.42 | 0 | HS |
| Cetirizine | 6 | 25 | 3.61 | 0.0001 | HS |
| Levocetirizine | 7 | 13 | 1.37 | 0.08 | NS |
| No | 88 | 148 | 6.4 | 0 | HS |
Acid Reducing agents
The H2 antihistaminics and the Proton Pump Inhibitors (PPIs) were prescribed in large numbers. These were probably prescribed prophylactically to reduce the gastric irritation which was caused by the NSAIDs and the AMAs.
DISCUSSION
The present study was a prospective, cross sectional and a comparative study which was done to evaluate the WHO drug use indicators among the GPs of the private sector dispensaries in Pune city. More than 60% of the drug use studies were carried out in the public sector [5]. Very few studies were carried out among the primary care providers in the private sector. Studies have been carried out to investigate the drug use in acute gastroenteritis [7], acute respiratory infections, etc. [8] The most common presenting complaint in the general practice is fever. So, the present study was carried out to investigate the drug use and the appropriateness of the treatment in cases of acute fever among the GPs in Pune city.
Core Drug use Indicators
The average number of drugs per encounter: In Indian studies, the average number of drugs per prescription was reported to be 2.8 by Khirsagar et al., [9] and Mhetre et al., [10] In the present study, for the MBBS practitioners it was 2.5, whereas for the BAMS practitioners, it was 4.5. The difference was statistically highly significant (p= 0). More number of drugs in the prescription lead not only to adverse effects of that particular drug, but it also increases the incidence of the drug interactions and the cost of the therapy, thus making it absolutely an irrational practice [11]. This is one of the important basic indicators of an irrational drug use.
The percentage of the encounters with an antibiotic which has been prescribed: The antibiotic use by both types of practitioners was on the higher side, particularly so with the BAMS doctors. The antimicrobial agents need not be prescribed to patients of viral fever, viral URTIs, malaria, chicken pox, etc. A large number of patients who suffered from viral fever also received AMAs in the present study. An excessive use of antibiotics will increase the cost, the adverse effects and also the development of resistance [12]. As per the WHO [13] the percentage of the encounters with an antibiotic which has been prescribed ranges between 40-50% and it is showing a little upward trend.
The percentage of the encounters with an injection which has been prescribed: Only 4.5% of the MBBS and 18.5% of the BAMS practitioners had injections in their prescription. All the injectables were AMAs only. All the prescriptions of the BAMS GPs had injectable AMAs which were inappropriate for their doses, as against only 33% which were prescribed by the MBBS GPs. An important finding was that only a single injectable AMA was given in all these cases, which was not followed later. The whole issue of the injectable AMAs, especially in the outdoor practice, is irrational. Apart from the increase in the cost and the development of local pain and tenderness, the transmission of diseases like AIDS can occur with injections [14].
The percentage of the drugs which were prescribed by their generic names: The WHO results showed that the percentage of the drugs which was prescribed in generics was 60% [13]. The essential drugs lists which were published by the WHO [15] and the Government of India [16] were considered as the standard to determine the drugs in the generics and EDL. It was observed that the BAMS practitioners used generic drugs for dispensing rather than for prescribing. The generic drugs are made available, mainly to reduce the extra costs which are levied by various companies and also to ensure a uniform effectiveness and safety. By dispensing the drugs in generics, it appeared that the doctors and not the patients got the benefit of the low cost of such medications. The patients get the prescriptions in the trade name, the cost of which is always on the higher side.
The percentage of the drugs which were prescribed from the essential drug list: The WHO has defined the essential drugs as “those that satisfy the priority health care needs of the population”. They are selected with due regards to their public health relevance, the evidence on their efficacy and safety and their comparative cost effectiveness” [17]. Prescribing from the essential drugs list ensures that the prescribers do not jump on the use of new but costly medications, with minimal data on their clinical utility [18]. According to the WHO, the percentage of drugs from the Essential Drugs List (EDL) is 70-90%. In our study, 52% of the drugs which were prescribed by the MBBS GPs and 58% of drugs which were prescribed by the BAMS GPs were from the Essential Drug List (EDL). These values are less than those of the WHO results.
All the core prescribing indicators of the BAMS practitioners were significantly abnormal. The antibiotic use was on the higher side in case of the MBBS practitioners, along with less number of drugs which were prescribed in their generic names and from the essential drugs list.
Evaluation of the appropriateness of the treatment: This indicator can also be used to evaluate the rational use of drugs. The Rational use of Medicines (RUM) requires that “patients receive medications which are appropriate to their clinical needs, in doses that meet their own individual requirements, for an adequate period of time and at the lowest cost to them and their community” [19]. So, RUM includes the proper selection, proper dose, proper duration and low cost of the pharmaceuticals. In the present study, efforts were made to compare the given treatment with the standard treatment guidelines (CMDT) [20] and also to verify the appropriateness of the dose and the duration of use of all the drugs.
The treatment of fever can be broadly divided into – A) Specific treatment and B) Symptomatic treatment.
A) Specific treatment: Antibiotics (AMAs) - The overall use of AMAs was on the higher side among both the GPs, especially the BAMS GPs. The use of AMAs in viral fevers and the routine use of Artemisinin in the combination therapy in malaria is irrational. The excessive use of AMAs can lead to more costs for the patient and also to the chances of development of resistance.
B) Symptomatic treatment:
a) Non steroidal anti-inflammatory drugs (NSAIDs): The BAMS GPs were found to prefer the Nimesulide and Paracetamol combination for any case of fever. The safety of Nimesulide is highly questionable. In the absence of monitoring, it is difficult to comment on whether Nimesulide should be used.
In patients of fever, Paracetamol is specifically effective. It may be required in higher doses if the 500mg dose does not work. Most of the patients who were put on NSAIDs which were other than Paracetamol, received treatment to prevent gastritis. In some prescriptions, antiemetics were also added. So, in the treatment of fever, the administration of NSAIDs which are other than Paracetamol, should ideally be avoided. We considered the excessive use of NSAIDs to be inappropriate.
b) Antihistaminics: were mainly used for viral and respiratory infections. The prescriptions which contained a wrong dose or two antihistaminic preparations were considered to be inappropriate.
c) Oral Rehydration Solution (ORS): Out of 14 patients with gastroenteritis, none were prescribed ORS. Therefore, all the prescriptions were considered to be inappropriate.
d) Antiemetics and Antimotility agents: No patients with gastro- enteritis received antiemetics or antimotility agents.
e) Acid Reducing agents: H2 antihistaminics and Proton Pump Inhibitors (PPIs) were prescribed in large numbers. These were probably prescribed prophylactically to reduce the gastric irritation which was caused by NSAIDs and AMAs. So, the acid reducing agents, though they were not components of the standard treatment guidelines, were not considered as inappropriate.
Only a wrong dose, duration of use or combination of antiemetics was considered as inappropriate.
f) Steroids-the use of any steroid preparation in case of acute fever was considered as inappropriate.
CONCLUSION
In the present study, the BAMS GPs had significantly abnormal WHO prescribing core drug use indicators and their percentage of inappropriate prescriptions was also alarmingly high (92%), With the MBBS GPs, it was observed that there was more use of antimicrobials, but the proportion of the inappropriate prescriptions was less (42%).