Pyogenic granuloma is thought to represent an exuberant tissue response to a local irritation or trauma. It is a reactional response to constant minor trauma and it might be related to hormonal changes. Clinically, these lesions usually present as single nodules or sessile papules with smooth or lobulated surfaces. These may be seen in any size, from a few millimetres to several centimetres. Pyogenic granuloma of the oral cavity is known to involve the gingiva more commonly (75% of all the cases). An extragingival occurrence of pyogenic granuloma is rare. This paper has described an extragingival pyogenic granuloma which occurred on the upper labial mucosa in a 30 years old female patient.
Pyogenic granuloma, Granuloma pyogenicum, Hyperplasia, Clinical feature
INTRODUCTION
Pyogenic Granuloma (PG) is a benign, non-neoplastic, mucocutaneous lesion [1]. The name, ‘pyogenic granuloma’ is a misnomer, since this condition is not associated with pus and as it does not represent a granuloma histologically. PG is thought to represent an exuberant tissue response to a local irritation or trauma. Some authors use the term, ‘lobular capillary hemangioma’ for this lesion or the terms, ‘vascular epulis’, ‘benign vascular tumour’, ‘hemangiomatous granuloma’ and ‘pregnancy tumour’ when it occurs in pregnant women. Occasionally, a nonspecific granulation tissue may proliferate from a recent extraction socket and it may resembles a PG. Such lesions are called as “epulis granulomatosum” [2–4].
CASE REPORT
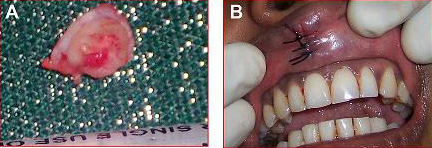
A 30 years old female patient reported to our department with the chief complaint of a growth on the upper lip, which had a history of one year’s duration. The patient had noticed a small growth on the upper labial mucosa one year back, which had gradually increased to the present size and it was associated with bleeding on chewing. The patient did not have any systemic disease. Her medical, dental and drug histories were non-contributory. On physical examination, she appeared to be healthy and of normal size and weight. The rest of the general physical examinations were within normal limits. The clinical examination [Table/Fig-1] revealed an exophytic, pedunculated lesion that measured 0.8 cm in diameter, and its surface covered was with pseudo-membrane, with some areas of erythema.
Extra oral view showing the pedenculated growth on the upper labial mucosa

An intra oral examination revealed [Table/Fig-2] a solitary exophytic growth on the upper labial mucosa, which measured 0.8 cm in diameter, with an erythematous area which was surrounded by a grayish white border. According to the patient, the lesion had existed from past one year and it had gradually increased to the present size. It caused bleeding on chewing The surface of the lesion appeared to be lobulated and the swelling was pedunculated. The lesion was firm in consistency and non tender, with minimal bleeding. When the patient closed her mouth, the swelling touched the sharp incisal edges of the right upper central and the lateral incisors [Table/Fig-3]. The patient also had poor oral hygiene. Depending on the history and the clinical examination, we arrived at a provisional diagnosis of a pyogenic granuloma with a differential diagnosis of a traumatic fibroma. Due to the relatively small size of the lesion, an excisional biopsy, along with a histopathologic evaluation was recommended as the diagnostic approach [Table/Fig-4].
Averted upper lip showing pedenculated growth with areas of ulceration and keratinization

Photograph showing pedenculated lesion in open mouth position

Photograph showing gross specimen of the lesion (A) and intra oral view after surgical excision (B)
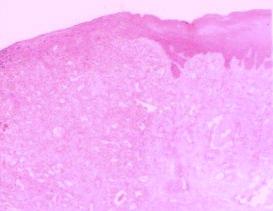
The histopathologic examination [Table/Fig-5] revealed granulation tissue with a non neoplastic proliferation of the endothelial cells, with blood cell formation and infiltration of the acute and the chronic inflammatory cells in a collagenous matrix. The surface of the lesion was consistent, with a hyperplastic parakeratinized stratified squamous epithelium, with areas of atrophy and ulcer and a fibrinoleukocytic membrane. These findings were consistent with the histopathological diagnosis of a pyogenic granuloma.
Low power photomicrograph (H & E stained) showing hyperplastic parakeratinized epithelium, endothelium lined channels and inflammatory cell
DISCUSSION
Jafarzadeh et al., [5] defined PG as an inflammatory overgrowth of the oral mucosa which was caused by minor trauma or irritation. According to Neville et al., [6] these injuries may be caused in the mouth by a gingival inflammation which was caused due to a poor oral hygiene, trauma or a local infection. The pathogenesis of PG at the molecular level may be considered as the imbalance of the angiogenesis enhancers and inhibitors. There is over production of VEGF-the vascular endothelial growth factor; bFGF-the basic fibroblast growth factor and decreased amounts of angiostatin, thrombopsondin-1, and the oestrogen receptors lead to the formation of PG [7]. The increased incidence of these lesions during pregnancy may be related to the increasing levels of estrogen and progesterone [1]. The purpose of publishing this article is to report an unusual case of an extragingival pyogenic granuloma which occurred on the upper labial mucosa.
The incidence of PG has been described to be between 26.8 and 32% of all the reactive lesions. Clinically, these lesions usually present as single nodules or sessile papules with smooth or lobulated surfaces. These may be seen in any size, from a few millimetres to several centimetres. As the lesions mature, the vascularity decreases and the clinical appearance is more collagenous and pink. Ulcerations are usually present in the areas where the tumour is subjected to trauma, like chewing, biting or prosthetic appliances. Rarely, does PG exceed 2.5 cm in size and it usually reaches its full size within weeks or months, remaining indefinite thereafter. The young PGs are highly vascular in appearance because they are composed predominantly of hyperplastic granulation tissue in which the capillaries are prominent. Thus, a minor trauma to the lesion may cause considerable bleeding, due to its pronounced vascularity. The clinical development of the lesion is slow, asymptomatic, and painless, but it may also grow rapidly [1, 5, 6, 8].
A higher frequency of PG is observed in the second decade of life, with a peak prevalence in teenagers and young adults, especially among women, probably because of the vascular effects of the female hormones [1, 2]. But in our case, the cause may be the continuous irritation and trauma which were caused by the right upper central and the lateral incisors and it was not related to the hormonal discrepancy.
The lesions are more common on the maxillary than on the mandible, and the anterior areas are more frequently affected than the posterior ones. The facial aspect is more commonly affected than the lingual or the palatal aspects. PG of the oral cavity is known to involve the gingiva commonly (75% of all the cases), although the occurrence of these lesions on the lips, tongue, oral mucosa, palate and he fingers has also been reported. PGs which affect the labial mucosa are rare. The gingival irritation and the inflammation that result from a poor oral hygiene, a dental plaque and a calculus or over-hanging restorations, may be the precipitating factors in many cases. PGs of the head and neck are uncommonly seen. Extragingivaly, PG occurs in the areas of frequent trauma such as the lower lip, tongue, palate and the buccal mucosa [4, 6, 9]. In the present case, the constant trauma which was inflicted by the sharp incisal edges of the right central and the lateral incisors could have been the etiology behind the growth on the upper labial mucosa and it was not related to a hormonal discrepancy.
The differential diagnosis of PG includes irritation fibroma, hemangioma, benign salivary gland tumours and metastatic tumours of the oral soft tissues, Kaposi’s sarcoma and leiomyoma. Although PG can be diagnosed clinically with considerable accuracy, radiographic and histopathological investigations aid in confirming the diagnosis and the treatment. Radiographs are advised to rule out a bony destruction which is suggestive of a malignancy or to identify a foreign body. A definitive diagnosis of PG can only be made by histopathologic examination of the biopsied tissue. PG histologically shows a highly vascular proliferation that resembles granulation tissue. Numerous small and larger endothelium-lined channels are formed, that are engorged with red blood cells. These vessels are sometimes organized in lobular aggregates and some pathologists look for this lobular arrangement to make a diagnosis (lobular capillary hemangioma). The surface that is usually ulcerated replaces the thick fibrinopurulent membrane. A mixed inflammatory cell infiltrate of neutrophils, plasma cells, and lymphocytes is evident. Neutrophils are more prevalent near the ulcerated surface; chronic inflammatory cells are found deeper in the specimen. The older lesions may have areas with a more fibrous appearance. Many gingival fibromas probably represent PGs that have undergone a fibrous maturation [1, 4, 5].
PG is a benign lesion; therefore, a surgical excision is the treatment of choice. The other conventional surgical modality which has been reported for the treatment of PG is cryosurgery in the form of either a liquid nitrogen spray or a cryoprobe, which has been used for the eradication of the lesion. It is a safe, easy, and an inexpensive technique which is suited for an out patients clinic setting. Nd: YAG and CO2, and flash lamp pulsed dye lasers have also been used for the treatment of PG. Lasers have proved to be a successful option for the excision of PG, with the advantages of minimal pain and invasiveness and the lack of a need of suturing or packing. There is a relatively high rate of recurrence (about 16%) after a simple excision. Recurrences after surgeries of the extragingival pyogenic granuloma are however uncommon [2, 6, 8–10].
CONCLUSION
The diagnosis of the oral lesions is complex and it leads the dentist to consider the distinct lesions with different diagnostic methods. The clinical features of pyogenic granulomas of the oral cavity, although they are helpful in making a differential diagnosis, are inadequate for a definite diagnosis in a given case. Further, their clinical resemblances to other inflammatory tumours, as well as to some true neoplasms of the oral cavity, necessitate an appropriate microscopic examination of the biopsy specimens, before the final diagnosis is made and adequate treatment is instituted.
[1]. Ramirez K, Bruce G, Carpenter W, Pyogenic granuloma: case report in a 9-year-old girlGeneral Dentistry 2002 50(3):280-81. [Google Scholar]
[2]. Karthikeya P, Mahima VG, Lahari K, Exragingival pyogenic granulomaIndian J Dent Res 2006 17(4):199-202. [Google Scholar]
[3]. Akyol MU, Yalciner EG, Dolan AI, Pyogenic granuloma (lobular capillary hemangioma) of the tongueInt J Pediatr Otorhinolaryngol 2001 58(3):239-41. [Google Scholar]
[4]. Graham RM, Pyogenic granuloma: an unusual presentationDent Update 1996 23:240-41. [Google Scholar]
[5]. Jafarzadeh H, Sanatkhani M, Mohtasham N, Oral pyogenic granuloma: a reviewJ Oral Sci 2006 48:167-75. [Google Scholar]
[6]. Nevile BW, Damm DD, Allen CM, Bouquot JE, Oral and Maxillofacial Pathology 2004 Second editionW.B. Saunders Co:444-49. [Google Scholar]
[7]. Yaun K, Jin YT, Lin MT, Expression of Tie 2, angiopoietin-1. angiopoietin-2. ephrin 62 and EphB4 in pyogenic granuloma of the human gingiva implicates their role in inflammatory angiogenesisJ Periodontal Res 2000 35:165-71. [Google Scholar]
[8]. Gordon-Nunez MA, De Vasconcelos CM, Benevenuto TG, Lopes MF, Silva LM, Galvao HC, Oral pyogenic granuloma: a retrospective analysis of 293 cases in a Brazilian populationJ Oral Maxillofac Surg 2010 68(9):2185-88. [Google Scholar]
[9]. Damm DD, Fantasia JE, Elevated and ulcerated nodule of lip. Pyogenic granulomaGen Dent 2002 50:466-68. [Google Scholar]
[10]. Gonçales ES, Damante JH, Rubira CMF, de Assis Taveira LA, Pyogenic granuloma on the upper lip: an unusual locationJ. Appl. Oral Sci 2010 18(5):538-41. [Google Scholar]