INTRODUCTION
Myoepitheliomas of the salivary glands were first described by Sheldon WH et al., in 1943 and they were considered as a variant of pleomorphic adenoma [1]. The World Health Organisation’s definition in 1991 [2] distinguished a myoepithelioma from a pleomorphic adenoma, classifying it as an independent entity. These tumours exhibit an admixture of four cellular morphologies, but the salivary gland tumours in which the ducts comprise less than 5% of the sections are classified as myoepitheliomas [3]. Also, in contrast to a pleomorphic adenoma, a myoepithelioma does not present a chondroid or an osteoid formation.
Myoepitheliomas represent less than 1% of all the salivary gland tumours [4]. Approximately, 50% of the salivary gland myoepitheliomas involve the parotid gland, 33% arise from the sublingual glands, and 13% affect the submandibular gland [5]. They present as asymptomatic, slowly growing masses in the patients with an average age of 40 years [6].
Embryologic and morphologic similarities such as the presence of regular myoepithelial cells, exist between the sweat glands, salivary glands, and the mammary glands, including their neoplasms [7]. We are reporting here, a case of a parotid gland myoepithelioma which was associated with a retroauricular subcutaneous mass that had been treated a few years earlier, on the presumption of an underlying diagnosis of a cutaneous myoepithelioma.
CASE
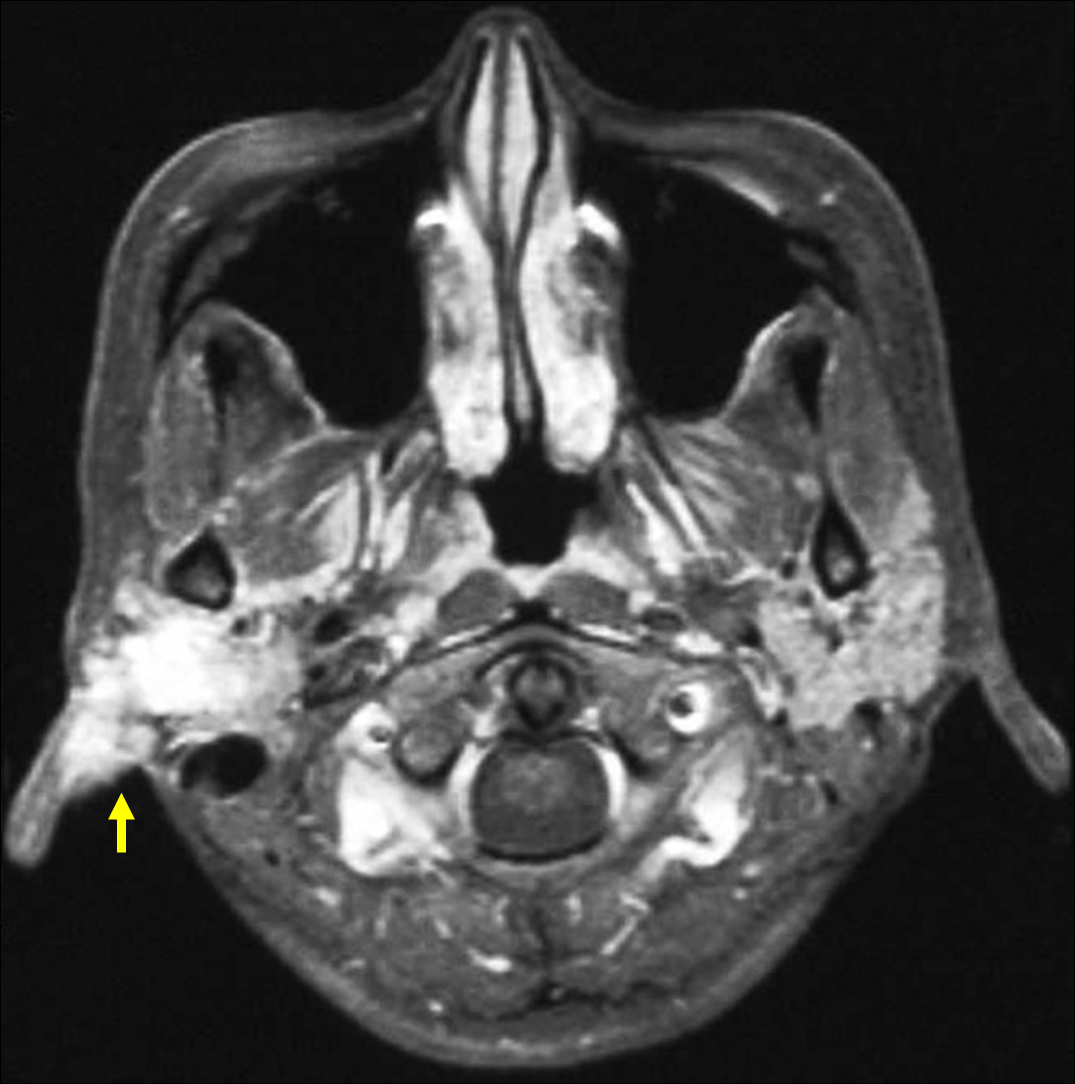
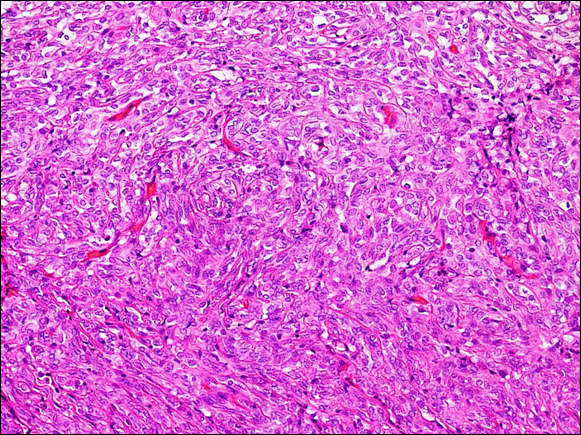
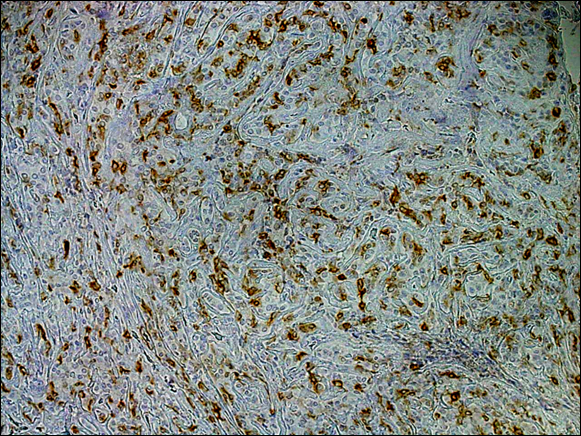
A female who was in her 40s was referred to our hospital with a right parotid gland tumour. She reported that she had undergone the resection of a painless, walnut-sized tumour in the right auricular region at a hospital’s Dermatology Department when she was in her 20s, and that she was told that the final diagnosis was a benign parotid gland tumour. Two years before presenting to us, a subcutaneous mass in the right retroauricular area was also resected at a hospital’s Dermatology Department. A month before visiting our hospital, she suffered from swelling and pain in the parotid gland area. A skin examination revealed a firm and a slightly movable, elastic, multinodular and a subcutaneous mass, which measured 2.2 × 1.8 cm. No evidence of facial nerve palsy or cervical lymphadenopathy was observed. Magnetic resonance imaging (MRI) revealed a multinodular mass (2.5 cm in large axis) in the parotid gland region, with a hypointensity being seen on the fat-saturated T1-weighted images and with a mid-hyperintensity being seen on the fat-saturated T2-weighted images. The bulk of the mass was just beneath the retroauricular skin [Table/Fig-1]. 18F-FDG positron emission tomography (PET) showed an area of high tracer uptake in the same region. No other high-uptake lesions were detected on a whole body scan. We suspected a malignant neoplasm of the parotid gland from the radiological appearance and a total parotidectomy was performed. The scar and the suture mark from the previous surgery were found. The mass was well encapsulated and it was dissected from the surrounding tissue. It was free of the facial nerve branches, which could be preserved. Grossly, the tumour had a lobular appearance with a multinodular architecture. Histologically, the tumour exhibited a sheet-like pattern of a monomorphous proliferation. The tumour cells had abundant eosinophilic cytoplasm. No cellular atypia, coagulative necrosis, or readily identifiable mitotic figures were observed [Table/Fig-2]. Immunohistochemically, the tumour cells showed a strong cytoplasmic immunoexpression of vimentin, CK (AE 1/AE3), S-100 protein, and smooth-muscle actin [Table/Fig-3]. A focal expression of p63 was observed in the nuclei of the tumour cells. A final diagnosis of a salivary gland myoepithelioma was made. The patient remained tumour-free at 1-year of the follow-up.
Gadolinium-enhanced T1-weighted magnetic resonance image showing a 2.5 cm heterogeneous hyperintense lesion in the parotideal region, just beneath the retroauricular skin
Photographs of hematoxylin-eosin (H-E) stainings of the surgical specimen. The tumor exhibited a sheet-like pattern of monomorphous proliferation. Monomorphous tumor cells with oval to round nuclear proliferation within a fibrotic or mucinous stroma (H-E staining, original magnification 400×)
Photographs of immunohistochemical stainings of the surgical specimen. The tumor cells showed strong cytoplasmic immunoexpression of smooth muscle actin (original magnification 400×)
DISCUSSION
A common stem cell in the developing glands is considered to have the capacity for a bidirectional differentiation into either epithelial or myoepithelial cells.
The main hypothesis is that the constituent tumour cells of the myoepitheliomas represent the features of each step of the myoepithelial cells’ differentiation from a stem cell, which may have the potential to differentiate into epithelial cells [8]. Extrasalivary examples of myoepitheliomas have been described, such as those in the breast, the larynx, and the skin. The myoepitheliomas of the skin and soft tissues exhibit morphology and immunohistochemical profiles which are similar to those of the salivary gland [7].
The criteria for the distinction of the benign and malignant myoepitheliomas on histological grounds are the cytological features which include pleomorphism, cellular atypia, an increased mitotic rate, necrosis and an invasive growth pattern [9–11]. These criteria were not met in our case.
An awareness on the wide morphologic range of the myoepitheliomas is necessary, in order to perform confirmatory immunohistochemical stains to make the correct diagnosis. The myoepitheliomas invariably express CK and hence, its absence would militate against this diagnosis [12,13]. Vimentin and S-100 protein, which usually are not present in the normal myoepithelial cells, are very sensitive markers of a neoplastic myoepithelium [12,13]. Because a neoplastic transformation causes the myoepithelium to lose or modify its smooth-muscle phenotype, immunohistochemical studies which demonstrate the smooth-muscle differentiation in these cells have been less useful. Sheldon AT et al.,[13] detected smooth-muscle actin and a muscle-specific action in 50 and 31% of the tumours, respectively. It was also suggested that the tumour cells in the myoepitheliomas are positive for the glial fibrillary acid protein andcalponin [12,13].
A search of the literature revealed one report of a myoepithelioma that was presurgically diagnosed as a cutaneous tumour, which was finally diagnosed as a tumour which originated from an accessory parotid gland [5]. The tumour in that case was found above the platysma and it was not palpable in the oral cavity, but in the cheek skin as a subcutaneous nodule and it was separately placed from the parotid gland [Table/Fig-4]. Microscopy revealed that the tumour was localized beneath the platysma and that it had pushed up the platysma and the subcutaneous tissues as it grew. The excretory ducts of the parotid gland were found in the deepest part of the tumour. On the basis of these findings, the tumour was finally diagnosed as an accessory parotid gland myoepithelioma [5].
The photograph of subcutaneous nodule in the retroauricular region taken 2 years before the first visiting to our department (yellow arrow)
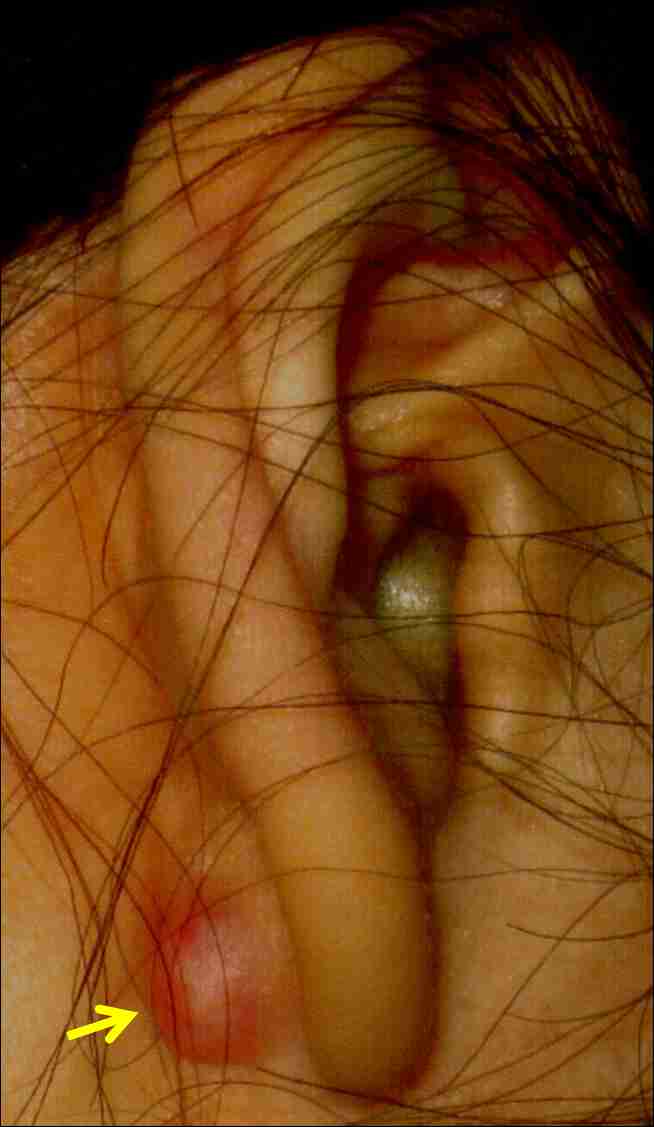
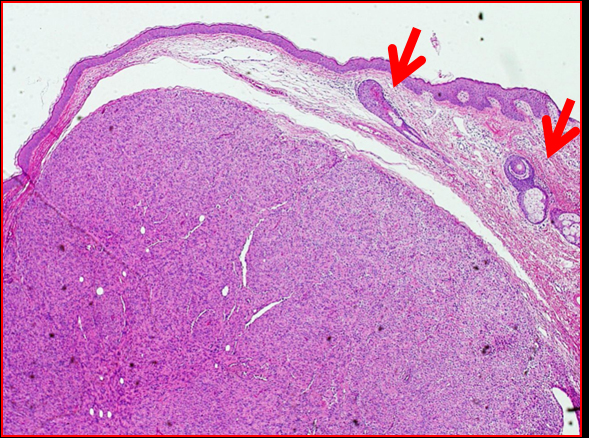
In our case, the tumour was well circumscribed and encapsulated, and the capsule was above the dermis, that had been excised by the dermatologist 2 years earlier, which had been diagnosed as a cutaneous myoepithelioma which had originated from the myoepithelial cells of the dermal sweat glands. The tumour included no parotid gland structures [Table/Fig-5]. Microscopy revealed that the tumour exhibited epithelial structures such as hair follicles and apocrine glands [Table/Fig-6].
Photographs of H-E stainings of the retroauricular subcutaneous tumor that had been excised by the dermatologist 2 years earlier. The tumor was encapsulated, and the capsule was above the dermis (original magnification 50×)

Photographs of H-E stainings of the retroauricular subcutaneous tumor that had been excised by the dermatologist 2 years earlier. The tumor was encapsulated, and the capsule was above the dermis (original magnification 50×)
The problem with the presented case is that the primary tumour was in the parotid gland 20 years ago and that there was almost no information on it, such as the histology, the resection margins or the technique of the treatments at that time or the radiological examinations. The tumour had recurred above the playsma. However, it was considered as a cutaneous myoepithelioma,2 years before the patient’s visit to our department, because the histopathological epithelial structures such as the hair follicles and the apocrine glands were without the parotid gland structures. It was considered that the histopathological diagnosis of the parotid gland which was resected 20 years ago was a myoepithelioma and that the tumour cells had scattered from the parotid gland to the dermis through the incision site and had slowly grown to present eventually as a retroauricular cutanous nodule beneath the platysma.
There are some reports of lesions which were clinically suspected to be cutaneous myoepitheliomas, that were finally confirmed to be of parotid gland origin [5,7]. If cutaneous nodules are found in the auricular or the buccal regions, the physicians should be cognizant of the possibility that the nodules are associated with parotid gland tumours, especially if the patient had a history of a surgical treatment for parotid gland tumours.
In our case, the pre-surgical radiological image which suggested the possibility of the tumour cells being dispersed from the parotid gland to the adjacent soft tissues, could have a differential clinical diagnosis as a malignant, invasive parotid gland tumour. To avoid such a possibility, the relationship of the cutaneous mass between the salivary gland and the adjacent structures, such as the muscles and the soft tissues, including the skin, should be examined prior to the surgery by CT or MRI [12]. In our case, although on the basis of the radiographical findings, the tumour was suspected to be malignant, a presurgical evidence of a preserved facial nerve function contributed to its consideration, with a strong possibility, a benign tumour. The clinical findings of facial nerve palsy could, therefore, be evidences of a malignancy.
The treatment of myoepitheliomas should be designed as for any benign salivary gland tumour. The first choice is surgery. The mass should be totally removed with a margin of normal gland tissue [12] and the tumour origin, whether it is the parotid gland or otherwise, must be detected in the surgical specimen [12].
A review of the literature, which included case reports, suggested a minimal tendency for a recurrence, at a similar rate as that for pleomorphic adenomas [14], which was reported to be around 10% or more [15]. The prognosis of benign myoepitheliomas is quite good [11].
Given the findings in our case, myoepitheliomas do indeed seem to replicate slowly, for decades, and they carry the possibility of the scattered tumour cells growing alongside the incision area in the adjacent tissues, after a parotid surgery. Thus, a long-term continuous follow-up is needed in such cases, for preventing a wider surgical intervention, because it can cause a delay in the diagnosis of the existing the parotid gland myoepitheliomas. Also, it is necessary to inform the patients that myoepitheliomas can recur even many years later and that the patients themselves can be on the alert, to check for new tumours. Our patient continues to undergo follow-up examinations to rule out a local recurrence.
CONCLUSION
Myoepitheliomas grow slowly, for decades, and they carry the possibility of the tumour cells that were scattered, growing in the adjacent tissues, after a parotid surgery. The relationship between the cutaneous mass and the salivary gland should be closely examined preoperatively and a long-term, continuous follow-up is necessary for preventing a wider surgical intervention, because it can cause a delay in the diagnosis.
Competing interests: The authors declare that they have no competing interests.
[1]. Sheldon WH, Heyman A, So-called mixed tumors of the salivary glandsArch Pathol 1946 35:1-20. [Google Scholar]
[2]. Seifert G, Brocheriou C, Cardesa A, Eveson JW, WHO International Histological Classification of Tumours Tentative Histological Classification of Salivary Gland TumoursPathol Res Pract 1990 186:555-81. [Google Scholar]
[3]. Ellis G, Anclair P, Benign epithelial neoplasms; in Ellis G, Anclair P eds.: Tumors of Salivary Glands, ed 3AFIP Atlas of Tumor Pathology 2002 Washington D. C.Mosby:57-68. [Google Scholar]
[4]. Nagao T, Sugano I, Ishida Y, Tajima Y, Matsuzaki O, Konno A, Kondo Y, Nagao K, Salivary gland malignant myoepithelioma: a clinicopathologic and immunohistochemical study of ten casesCancer 1998 83:1292-99. [Google Scholar]
[5]. Isogai R, Kawada A, Ueno K, Aragane Y, Tezuka T, Myoepithelioma possibly originating from the accessory parotid glandDermatology 2004 208:74-78. [Google Scholar]
[6]. Dardick I, Van Nostrand AW, Myoepithelial cells in salivary gland tumors--revisitedHead Neck Surg 1985 7:395-408. [Google Scholar]
[7]. Kutzner H, Mentzel T, Kaddu S, Soares LM, Sangueza OP, Requena L, Cutaneous myoepithelioma: an under-recognized cutaneous neoplasm composed of myoepithelial cellsAm J Surg Pathol 2001 25:348-55. [Google Scholar]
[8]. Da Silveira EJ, Pereira AL, Fontora MC, de Souza LB, de Almeida Freitas R, Myoepithelioma of minor salivary gland--an immunohistochemical analysis of four casesBraz J Otorhinolaryngol 2006 72:528-32. [Google Scholar]
[9]. Di Palma S, Guzzo M, Malignant myoepithelioma of salivary glands: clinicopathological features of ten casesVirchows Arch A Pathol Anat Histopathol 1993 423:389-96. [Google Scholar]
[10]. Chhieng DC, Paulino AF, Cytology of myoepithelial carcinoma of the salivary glandCancer 2002 96:32-36. [Google Scholar]
[11]. Karli R, Myoepitheliomas are rare tumors of the parotid gland: a case report and review of the literatureUnivers J Med Dent 2012 1:1-4. [Google Scholar]
[12]. Lee M, Nam S, Choi H, Choi JH, Moon KC, Koh JK, Myoepithelioma of parotid gland presenting as infra-auricular subcutaneous massJ Cutan Pathol 2005 32:240-44. [Google Scholar]
[13]. Savera AT, Sloman A, Huvos AG, Klimstra DS, Myoepithelial carcinoma of the salivary glands: a clinicopathologic study of 25 patientsAm J Surg Pathol 2000 24:761-74. [Google Scholar]
[14]. Sciubba JJ, Brannon RB, Myoepithelioma of salivary glands: report of 23 casesCancer 1982 49:562-72. [Google Scholar]
[15]. Machtens E, Salivary gland diseases in GermanyMund Kiefer Gesichtschir 2000 4(Suppl 1):S401-S13. [Google Scholar]