Case Report : Hermansky Pudlak Syndrome (Presenting as late onset heavy Menstrual Bleeding)
Amita Ray1, Sujoy Ray2, Jose John Matthew3
1 Assistant Professor, Department of Obstetrics and Gynaecology, Father Muller Medical College, Kankanady, Mangalore-575002 Karnataka, India.
2 Intern (MBBS), Department of Medicine, Kasturba Medical College Manipal, Karnataka-576104, India.
3 Intern (MBBS), Department of Obstetrics and Gynaecology, Father Muller Medical College, Kankanady, Mangalore-575002 Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Amita Ray, Assistant Professor, Department of Obstetrics and Gynaecology, Father Muller Medical College, Kankanady, Mangalore–575002, India.
Phone: 91-9916934563,
E-mail: amitarays@gmail.com
Inherited bleeding disorders contribute significantly to the incidence and prevalence of Heavy Menstrual Bleeding (HMB), and contrary to popular belief can present any time during the reproductive years of a woman’s life. The following case exemplifies this and is being presented as part of a rare syndrome. The incidence of this syndrome in the general population ranges from 1:500,000 to 1:1000, 000. Besides being rare the presentation was quite uncommon as majority of these cases present with pulmonary fibrosis.
Hermansky–Pudlak syndrome (HPS), Heavy menstrual bleeding
Case Report
A 42-year-old nulliparous woman presented to our OBG OPD with chief complaints of a prolonged and excessive bleeding during menses, with passage of clots which she had seen since past 7 months. She gave a history of easy bruising, but of no other major episode of bleeding . She did not have any previous history of surgery or trauma. She gave a history of dyspnoea upon exertion which was there since the past 2 months. There was no other history of chronic illnesses. Her parents has a consanguineous marriage and both her siblings had occulocutaneous albinism. Her Physical examination revealed oculocutaneous albinism [Table/Fig-1] and nystagmus. There were maculopapular erythematous lesions all over sun-exposed areas [Table/Fig-2]. Her Chest examination did not reveal any finding. Rest of the her systemic examination was normal. An Ophthalmic examination revealed a visual acuity of 6\60.
Photograph of case with oculocutaneous albinism

Photograph of arm with maculo-papular erythematous patches

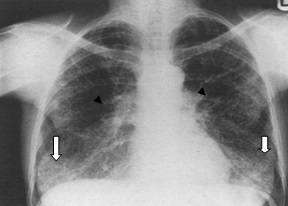
Haemoglobin was 7.4 mg/dL. The platelet count was normal (285 × 103/μL). The bleeding time was prolonged (>15 minutes; normal 2–9 minutes). The APTT was mildly prolonged, 38.7s (normal, 25.2–36.0). Serum anti–cardiolipin levels were increased for IgA (17.8 APL; normal < 13). IgG and IgM levels were normal. Serum IgE was elevated 546.9IU/ml (normal up to 100 IU/ml) Chest X–ray revealed Prominent bronchovascular marking and little reticular opacity bilaterally in the lower zones. No hilar or mediastinal lesion was seen. Cardiac silhouette was within normal limits [Table/Fig-3].
Chest X-Ray showing prominent broncho-vascular markings (black arrows) and bilateral reticular opacity (white arrows) in both lower zones
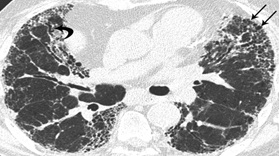
High Resolution CT of the lungs revealed diffuse areas of sub pleural reticulation bilaterally, with no specific predilection for any zone. Patchy areas of ground glass attenuation were noted throughout both the lungs. No evidence of traction bronchiectasis or subpleural cyst formation was seen. These features were suggestive of early (Grade1) pulmonary fibrosis [Table/Fig-4].
CT Lung showing features suggestive of Grade 1 Pulmonary Fibrosis(black arrows)
Spirometry was within normal limits, which was seen as FEV1/FVC% Pred >95 and FVC % Pred >80.
Echocardiography showed normal valves and chambers with normal LV systolic and diastolic functions.
An abdominopelvic ultrasound revealed a normal uterus and adnexa, with an endometrial thickness of 7mm.
She was given blood transfusion and was started on oral contraceptive pills for the management of heavy menstrual bleeding. She was given the option of antifibrinolytics and Desmopressin use during her menstrual cycle. She was counselled as regards the benefits of insertion of a progesterone containing device for the management of heavy menstrual bleeding. As she was nulliparous and anxious to have a child, she was also counselled as regards the possibility of her having a child with albinism and HPS.
The patient was advised regular follow up to check for her lung functions and was asked to avoid any factors which would enhance pulmonary fibrosis e.g. smoking. As by far, pulmonary fibrosis has been found to be the most important cause of morbidity and mortality in HPS.
Discussion
Hermansky-Pudlak syndrome (HPS) was first documented in 1959 by two Czechoslovakian physicians, who described two albino adults who were in their fourth decades, who had with severe bleeding and prolonged bleeding times [1]. It is an autosomal recessive disorder which is characterized by prolonged bleeding with occulocutaneous albinism, pulmonary fibrosis and, platelet dysfunction and in some cases as by granulomatous colitis. It is extremely rare in the general population. Across the globe, the incidence of HPS is between 1 in 500,000 to 1 in 1,000,000. This is a conservative estimation as the disorder is frequently undiagnosed [2]. The prevalence of HPS is highest in the north-western quarter of the island of Puerto Rico, which affects approximately 1 in 1,800 persons, and approximately 1 in 22 persons are carriers of the gene [3].The diagnosis of Hermansky-Pudlak syndrome (HPS) is established by clinical findings of oculocutaneous albinism, in combination with a bleeding diathesis of variable severity [4].
Patients with HPS usually present in early childhood with easy bruising of soft tissues, epistaxis and prolonged bleeding after a dental extraction or surgery [3]. Women may present with a medically significant menstrual bleeding. Oculocutaneous albinism is a defining aspect of thise disorder, but it varies widely in the degree of hypo pigmentation as well as in correlation between retinal pigmentation and hair/skin pigmentation [3,4].
Pulmonary fibrosis is a serious complication of this syndrome, which usually presents in the fourth or fifth decade of life and it contributes to significant morbidity [5]. The only known treatment for pulmonary fibrosis is lung transplantation, though an antifibrotic agent, Perifenidione, has been shown to slow the progression [6,7].
Besides the above, a bleeding granulomatous colitis which resemblesing Crohn’s disease may also be a complication of the HPS [4]. The colitis in some cases may be so severe and it may as to require colectomy. Although the colon is primarily involved in HPS, any part of the alimentary tract, including the gingiva, can be affected [8]. Cardiomyopathy and renal failure have also been reported in HPS [9].
Menorrhagia, as a manifestation of HPS, has been recorded in literature and should be suspected in patients with oculocutaneous albinism and bleeding disorders [10,11]. Certain cases have proved to be refractory to the above mentioned therapies and they have had to be controlled by using recombinant factor VIIa (rFVIIa) [10]. Other cases have responded well to Levonorgestrel containing intrauterine devices [12].
Inherited bleeding disorders are found in a substantial proportion of women with menorrhagia and a normal pelvis examinations. [13]. These might not manifest at menarche. They presentation may manifest later on in life. While encountering such cases are encountered, rare genetic disorders should be also kept in mind, especially when other clinical (like oculo–cutaneous albinism) or diagnostic criteria are satisfied, as in the above case.
Conclusion
The presentation of this case as late onset heavy menstrual bleeding was the unique feature. The Hermansky–Pudlak syndrome has an incidence of only 1 in 500,000 across the globe. When it does present, it is much earlier in life and with symptoms arising due to pulmonary fibrosis or bleeding disorders. This case however, did not report heavy menstrual bleeding, since menarche rather came as late onset heavy menstrual bleeding, which is more common in acquired bleeding disorders rather than in inherited ones.
[1]. Hermansky F, Pudlak P, Albinism associated with hemorrhagic diathesis and unusual pigmented reticular cells in the bone marrow: report of two cases with histochemical studiesBlood 1959 14:162-69. [Google Scholar]
[2]. Gahl WA, Huizing M, Hermansky-Pudlak Syndrome. In: Pagon RA, Bird TD, Dolan CR, et al., editorsGeneReviews™ 2000 Jul 24 Seattle (WA)University of Washington, Seattle:1993[Updated 2012 Oct 11]. [Internet] Available from: http://www.ncbi.nlm.nih.gov/books/NBK1287/ [Google Scholar]
[3]. Witkop CJ, Nuñez Babcock M, Rao GH, Gaudier F, Summers CG, Shanahan F, Albinism and Hermansky-Pudlak syndrome in Puerto RicoBol Asoc Med P R 1990 Aug 82(8):333-9. [Google Scholar]
[4]. Gahl WA, Brantly M, Kaiser-Kupfer MI, Iwata F, Hazelwood S, Shotelersuk V, Genetic defects and clinical characteristics of patients with a form of oculocutaneous albinism (Hermansky-Pudlak syndrome)N Engl J Med 1998 338:1258-64. [Google Scholar]
[5]. Wei ML, Hermanksy-Pudlak syndrome: a disease of protein trafficking and organelle functionPigment Cell Res 2006 19:19-42. [Google Scholar]
[6]. Lederer DJ, Kawut SM, Sonett JR, Vakiani E, Seward SL, White JG, Successful bilateral lung transplantation for pulmonary fibrosis associated with Hermansky-Pudlak syndromeJ Heart Lung Transplant 2005 24:1697-1699. [Google Scholar]
[7]. Gahl WA, Brantly M, Troendle J, Avila NA, Padua A, Montalvo C, Effect of pirfenidone on the pulmonary fibrosis of Hermansky-Pudlak syndromeMol Genet Metab 2002 76:234-742. [Google Scholar]
[8]. Hussain N, Quezado M, Huizing M, Geho D, White JG, Gahl W, Intestinal disease in Hermansky-Pudlak syndrome: occurrence of colitis and relation to genotypeClin Gastroenterol Hepatol 2006 4:73-80. [Google Scholar]
[9]. Witkop CJ, Quevedo WC, Fitzpatrick TB, King RA, Albinism. In: Scriver CR, Beaudet AL, Sly WS, Valle DL editorsThe Metabolic and Molecular Basis of Inherited Disease 2000 Vol26 edNew YorkMcGraw-Hill:2905-47. [Google Scholar]
[10]. Lohse J, Gehrisch S, Tauer JT, Knöfler R, Therapy refractory menorrhagia as first manifestation of Hermansky-Pudlak syndromeHamostaseologie 2011 31(Suppl 1):S61-3. [Google Scholar]
[11]. Harrison C, Khair K, Baxter B, Hermansky–Pudlak syndrome: infrequent bleeding and first report of Turkish and Pakistani kindredsArch dis Child 2002 86:297-301. [Google Scholar]
[12]. Kingman C.E.C., Kadir R.A., Lee C.A., The use of levonorgestrel releasing intrauterine system for treatment of menorrhagia in women with inherited bleeding disordersBJOG 2004 111:1425-28. [Google Scholar]
[13]. Kadir RA, Economides DL, Sabin CA, Owens D, Lee CA, Frequency of inherited bleeding disorders in women with menorrhagiaLancet 1998 Feb 14 351(9101):485-9. [Google Scholar]