Replacement of missing teeth with a fixed partial denture has remained a viable alternative for over centuries. However, the success of the fixed partial denture depends on a large number of factors. Though it is often considered as a permanent restoration, often, the fixed partial denture is vulnerable to dislodgement when it is called to function in an environment which is constantly bothered by saliva and torque caused by masticatory forces.
Though control of taper has been researched to be primary factors, the clinician often ends up preparing a taper of 140 to 200. Hence, the retention of the fixed partial denture, often, is left to the retention which is provided by the cement alone [1].
Luting is the main function of the traditional luting cements. It fills the interfacial space between a fixed prosthesis and the prepared tooth. It locks the restoration in place by flowing into the surface irregularities of both the tooth and the crowns [2]. Zinc phosphate cement has been the most popular luting material for more than 90 years. Despite its high solubility and lack of adhesion, its excellent clinical performance, which can be attributed to its high fatigue strength, has been reported for fixed partial dentures which are cemented with zinc phosphate cement [3]. However, the mechanical properties of the cement can influence stress distribution within the interposed cement layer, the bonding efficacy of cement to both surfaces, and durability of cement, including the long term resistance to mechanical deterioration [4].
The bonding of the casting to the tooth surface topography may be altered due to application of desensitizing agent which is often recommended after tooth preparation, to eliminate sensitivity which arises due to exposure of dentinal tubules which are primarily and secondarily caused by pH of unreacted acid, which prevents unset luting cement [5].
Brannstorm’s hydrodynamic theory speculated that any stimulus to dentin can be transmitted back to nerve receptors. He also postulated that this occurred as a result of fluid movement in the dentinal tubules, with stimulation of the odontoblast, which elicited a response by nerve fibres and resulted in pain [6].
Several agents have been advocated for sealing dentin before cementation, to decrease the post-cementation sensitivity. Sealing of the dentinal tubules with polymeric resin reduced sensitivity and possibly the ingress of bacteria [6].
Given the concern, the present study was conducted to analyze the effects of resin based sealers on retention of casting cemented by using three different luting cements – Zinc Phosphate cement, Glass ionomer cement and Resin modified glass ionomer cement.
Materials and Methods
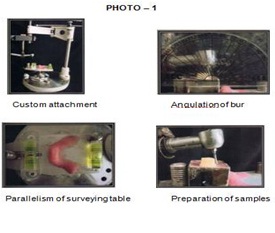
For the present study, 60 recently extracted, non carious and non restored molars were selected from Department of Oral and Maxillofacial Surgery, K.M.Shah Dental College and Hospital and they were stored in a liquid steriliant, i.e 0.5% Sodium hypochlorite solution, in compliance with Centres for Disease Control recommendations [7]. Teeth were cleaned of any debris with an ultrasonic scaler and they were then stored in water at room temperature. The roots of the extracted tooth were roughned and embedded in a stainless steel mould by using autopolymerizing resin (Rapid Repair, Pyrax). The teeth were positioned in such a way, so that the cementoenamel junction remained 1mm above the top of the stainless steel mould. The occlusal surface of the teeth were sectioned flat 5mm above the top of the steel mould by using a dough nut bur. A custom made metal attachment was fabricated, which was designed to fit in the Surveyor (Marathon – 103, Saeyang company). A high speed contrange hand piece (NSK, Naknishi Inc.) was secured in the custom made attachment, so that a diamond bur was oriented at an angle of 10 degrees to the vertical axis to create a convergence angle of 20 degrees. The mounted teeth were secured vertically on the cast holder, which was made parallel to the level of group by using a bubble gauge.
A parallel sided, straight fissure diamond bur was used to prepare axial surface and a shoulder finish line was established in each specimen. The axial surface was reduced to a depth of 1mm and an axial length of 4mm by using a new diamond bur for each specimen under a water jet, to dissipate any heat which was formed [Table/Fig-1]. All specimens were finally finished with finishing bur and care was taken to maintain the angle of convergence [Table/Fig-2].
Custom attachment, Angulation of Bur, Parallelism of surveying Table, Preparation of samples
Prepared samples, Die & wax pattern, Sprue tree, Castings

Impressions of the prepared teeth were made in a custom made autopolymerizing resin tray by using dual impression technique with an addition silicon impression material (Aquasil, DENTSPLY). The impressions were poured with Type – IV gypsum (KALROCK, Kalabhai) and they were reinforced by adding a die hardner (Prime dent, India Ltd). Three even coats of die relief (Prime dent, India Ltd) were applied to each master die in a controlled fashion, with time being provided for the previous layer to dry. Die lubricant (Wax Separator, Han Dae Chemical Co. Ltd) was painted on the master die, and excess lubricant was removed with a gentle stream of air. The die was subsequently dipped twice in molten pattern wax (Bego, Bremer GmBh and Co. KG, Germany) to achieve a consistent thickness of 1mm. A wax loop was then fabricated and added to the centre of the wax pattern.
Margination of each wax pattern was completed with sculpting wax before investing. The wax patterns were spruced and invested with phosphate bonded investment (Virovest, Bego) by following manufacturer’s directions. The test crowns were casted by using Ni-Cr alloy (CB 80, DENTSPLY) [Table/Fig-2]. Minor adjustments which were necessary to seat the casting on the dies were completed by using a small round bur which was mounted in a laboratory hand piece. The fit of the completed restoration was again verified on preparation, prior to cementation. The internal surfaces of all castings were cleaned by using a steam cleanser (Vilman, India Ltd) to remove the remaining debris. The internal surfaces of all castings were air abraded with 50 micron alumina particles in a sandblaster (Rancon, model RF – 4) at 60 psi and a distance of 6mm from the nozzle tip. Prior to cementation, a replica of the occlusal surface of each prepared tooth was digitized. A thin replica of the occlusal surface was formed by placing autopolymerizing resin. The perimeter of the replica was highlightened with a black marker. The entire occlusal replica, along with a circle of known dimension, was digitized on a flat-bed scanner. By using digitized images of the standard and occlusal surfaces, scion image analyzer software was used to determine the length of the perimeter. The dimension of the tooth was multiplied by the axial length, to arrive at the axial surface area of each preparation. Only those specimens with surface areas which were in the range of 108 – 118 sqmm were included in the study.
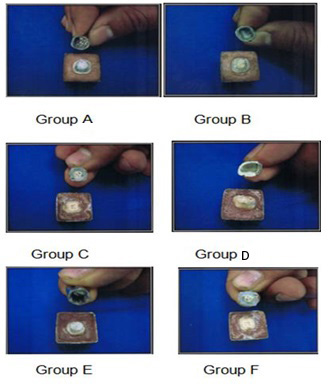
All the specimens were then randomly divided into 6 groups, so that each group contained 10 specimens with approximately equal mean axial surface areas. These groups were named A, B, C, D, E, F). Three of the six groups were control groups for Zinc phosphate, glass ionomer and resin modified glass ionomer (A,B, C). The remaining three groups were for 3 cements which were to be treated with resin based sealer and they were cemented with three luting cement (D, E, F).
Cementation of casting for Group A (Zinc phosphate cement)
In order to achieve a homogeneous consistency, 1.5g of powder and 1.0gm of liquid were taken. A clean dry glass plate and a metal spatula were taken. The measured quantity of powder was divided into four portions (1/2, 1/4, 1/8, 1/8). Beginning with the smallest quantity, the powder was mixed with the measured liquid within 90 seconds. When the peak which was formed on lifting slowly fell back into the paste, the mix was ready to use.
Cementation of castings for Group B (Glass ionomer cement)
The standard powder to liquid ratio (1.8/1g) i.e. one level scoop of powder to 2 drops of liquid was taken. The powder and liquid were dispensed onto the mixing pad by using a plastic spatula. All the powder was added to the liquid and it was mixed rapidly for 20 seconds.
Cementation of castings for Group C (Modified glass ionomer cement)
The cement consisted of a base and a catalyst paste which were packaged in 3M ESPE clickerTM dispensing system. The clicked was fully depressed to dispense “One click” of cement onto the mixing pad. The paste was automatically dispensed in equal volume. By using a plastic or metal cement spatula, the pastes were mixed together for 20 seconds until a uniform colour was achieved.
A thin layer of cement was applied to the inside surface of castings and the castings were initially seated with a strong finger pressure for Groups A, B and C.
Application of resin sealer prior to cementation of Group D, E, and F
Dentin was etched for 15 seconds with 32% phosphoric acid which contained bezoylalkonium chloride. Thereafter, the preparation was rinsed for 20 seconds, and moisture was removed, so that the dentin remained visibly moist. Two coats of the resin sealer were applied, they were thoroughly dried with air, and light polymerized for 10 seconds, with light held at the surface with 400mW/cm2 intensity. For group F, the internal surface of a clean received 1 coat of the 2 – step single bottle adhesive, after which it was dried and light polymerized.
All the castings for each group, i.e. A, B, C, D, E and F were assembled with prepared teeth and they were placed in a loading device and subjected to an axial force of 20 kg for 10 minutes. The excess cement was removed from the margin. Margins of the specimens were protected with petroleum jelly. After complete setting of the cements (24 hours), the specimens were placed in water at room temperature. They were then subjected to thermocycling for 1 month in a thermocycling unit at 5 to 55 degrees Celsius for 500 cycles, with a dwell time of 30 seconds. Crowns were subjected to an axial dislodgement force until failure on a Universal Testing Machine (Instron) at a cross head speed of 0.5 mm/min [Table/Fig-3]. The force at dislodgement and nature of debonding were recorded. Immediately following casting dislodgement, the casting and tooth were examined to arrive at the type of failure modes. The data which was thus obtained was tabulated and subjected to statistical evaluation by using t-test for controls and non controls. Data which was hence obtained was analyzed by using one way ANOVA for dislodgement stress [Table/Fig-4].
Crowns subjected to an axial dislodgement force until failure on a Universal Testing Machine (Instron) at a cross head speed of 0.5 mm/min

Comparatives values for all groups by ANOVA One way
| n | Mean | Std. Deviation | Std. Error | 95% Confidence Interval for Mean | Minimum | Maximum |
|---|
| Lower Bound | Upper Bound |
|---|
| A | 10 | 24.5540 | 3.37229 | 1.06641 | 22.1416 | 26.9664 | 19.77 | 29.42 |
| B | 10 | 32.0220 | 3.43265 | 1.08550 | 29.5664 | 34.4776 | 26.62 | 37.32 |
| C | 10 | 41.8950 | 3.89493 | 1.23168 | 39.1087 | 44.6813 | 36.68 | 48.65 |
| D | 10 | 14.6510 | 2.70221 | .85451 | 12.7180 | 16.5840 | 9.35 | 18.26 |
| E | 10 | 37.9090 | 6.70707 | 2.12096 | 33.1111 | 42.7069 | 28.26 | 47.65 |
| F | 10 | 57.2390 | 6.97908 | 2.20721 | 52.2460 | 62.2320 | 43.81 | 67.22 |
| Total | 60 | 34.7117 | 14.30624 | 1.84693 | 31.0160 | 38.4074 | 9.35 | 67.22 |
Discussion
The replacement of missing and/or lost teeth by fixed partial dentures has definite advantage over removable partial dentures. Fixed prosthodontics has attracted a lot of research work in recent times [8]. Crown retention is one of the basic criteria for successful fixed prosthodontics. The quality of a preparation that prevents the restoration from becoming dislodged by such forces, which is parallel to the path of withdrawal, is known as retention. In fixed prosthodontics, luting agents hold the crown on the tooth structure and they partly determine its life. An array of cements have been introduced to dentistry over years, with constant improvization being the motivating factor. But these agents have their own advantages and disadvantages. To overcome these disadvantages, solutions also arise by time, which is also an area of research work of intrest [8]. The purpose of this study was to evaluate this effect of resin based sealers on crown retentions for most commonly used cements, which are zinc phosphate, glass ionomer and modified resin cement. The selection of the natural human molars was done, in order to stimulate the oral enviornment, as these exhibit decreased crown lengths with high carious indices and as the stress concentrations of occlusal forces were more. They were stored in a liquid sterilant to maintain good oral hygiene which was in compliance with Centres for Disease control recommendations [7].
Theoretically, maximum retention is obtained if a tooth preparation has parallel walls. However, it is impossible to prepare a tooth this way by using current techniques and instrumentations. Slight undercuts are created, that prevent the restoration from seating. So, a slight convergence or taper is necessary in completed preparations [9]. The recommended convergence between opposing walls is 6 degrees [10]. When convergence angle is increased, the effect of taper on crown retention is decreased and effect of luting agent on crown retention is magnified. In most clinical situations, studies have demonstrated that the degree of convergence which was found clinically was approximately 20 degrees [11]. For this reason, in present study, a convergence angle of 20 degrees was chosen. When a retentive failure occurred, cement often adhered to both the tooth preparation and the fitting surfaces of the restoration. In these cases, cohesive failures occurred through the cement layers, because the strength of the cement was less than the induced stress. A computerized analysis of these stresses revealed that they were not uniform throughout the cement, but were concentrated around the junction of the axial and occlusal surfaces [12]. Changes in the geometry of the preparation (e.g. rounding the internal line angle) may reduce stress concentrations and thus increase the retention of the restoration [13,14]. Impressions and dies of the tooth preparation were made. Die spacer was applied to provide space for the cement. The space was standardized to three coats, to provide space of 25 microns. Also, as was shown by Rosensteil and Gegauff [15] the castings made from dies which were painted with three coats of die spacer showed no effect on retention of the casting to the tooth. A dipping technique was used to make the wax patterns of thickness 1mm in lines, as per the method which was advocated by Johnson et al., [16]. When the internal surface of a restoration was very smooth, retention failure occurred, not through the cement, but at the cement restoration interface. Under these circumstances; retention will be increased if the restoration is roughned or grooved [13,14,17]. The cements which were used in the present study were Zinc phosphate cement (Harvard), Glass ionomer cement (GC, lining and luting cement), Modified glass ionomer (RelyXTm Luting 2,3M ESPE).
One of the most common disadvantages of these luting agents was the post cementation sensitivity. This was caused by acid content of these agents. To reduce this sensitivity, many agents such as resin primers, Gluma desensitizers, Gluteraldehyde based desensitizers and varnishes are applied on the tooth preparation, prior to cementation of crown. The agent might affect the bonding of cement to prepared dentin and interact with retentive properties of the luting agents. The sealer which was used in this study was 2 step, single-bottle multipurpose bonding system (One step, Bisco Inc, Schaumburg, III). Two coats of the sealer were applied to the teeth preparations according to manufacturer’s instructions. Castings were now cemented as the group by using a load of 20 kg on the Instron (Universal Testing Machine). When the teeth were in occlusion, the stress concentration was estimated to be in between 10 kg and 22 kg. Cemented specimens were subjected to thermocycling cycles, to duplicate the process of subjecting a restoration and tooth to temperature extremes, that conformed to those which were found in oral cavity.
Thermocycled specimens were loaded for retention test on the universal testing machine till a failure occurred. These values were statistically analyzed to compare the significant differences between them. Group A and Group D, after t-test, showed a value of p=0.001, which indicated that there was a significant difference between their means. Group B and E, after t-test, showed a value of p=0.85, which indicated that there was no significant difference in between their means. Groups C and F, after t-test, showed a value of p= 0.001, which indicated that there was a significant difference in between their means [Table/Fig-5]. The research hypothesis, that application of a resin sealer to dentin would decrease casting retention for zinc phosphate and not affect glass ionomer, was only partially correct. The resin sealer reduced casting retention significantly (46%) for zinc phosphate cement, but it contributed to a 60% increase in retention for glass ionomer cement. Swift EJ et al., [18] conducted a study that employed the same 2-step single bottle adhesive system as a sealer, which did not demonstrate any effect of the adhesive sealer on casting retention when it was cemented with zinc phosphate, glass ionomer or resin modified glass ionomer cement. The effects may have been present, but a very low degree of taper was used.
Mean values of all control and non control groups
| (I) Force_Group | (J) Force_Group | Mean Difference (I-J) | Std. Error | Sig. |
|---|
| A | B | -7.46800(*) | 2.15507 | .013 |
| C | -17.34100(*) | 2.15507 | .000 |
| D | 9.90300(*) | 2.15507 | .000 |
| E | -13.35500(*) | 2.15507 | .000 |
| B | F | -32.68500(*) | 2.15507 | .013 |
| A | 7.46800(*) | 2.15507 | .013 |
| C | -9.87300(*) | 2.15507 | .000 |
| C | D | 17.37100(*) | 2.15507 | .000 |
| E | -5.88700 | 2.15507 | .085 |
| F | -25.21700(*) | 2.15507 | .000 |
| A | 17.34100(*) | 2.15507 | .000 |
| D | B | 9.87300(*) | 2.15507 | .000 |
| D | 27.24400(*) | 2.15507 | .000 |
| E | 3.98600(*) | 2.15507 | .444 |
| F | -15.34400(*) | 2.15507 | .000 |
| A | -9.90300(*) | 2.15507 | .001 |
| E | B | -17.37100(*) | 2.15507 | .013 |
| C | -27.24400(*) | 2.15507 | .001 |
| E | -23.25800(*) | 2.15507 | .000 |
| F | -42.58800(*) | 2.15507 | .000 |
| A | 13.35500(*) | 2.15507 | .000 |
| F | B | 5.88700(*) | 2.15507 | .085 |
| C | -3.98600(*) | 2.15507 | .444 |
| D | 23.25800(*) | 2.15507 | .000 |
| F | -19.33000(*) | 2.15507 | .000 |
| A | 32.68500(*) | 2.15507 | .000 |
| B | 25.21700(*) | 2.15507 | .000 |
| C | 15.34400(*) | 2.15507 | .000 |
| D | 42.58800(*) | 2.15507 | .000 |
| E | 19.33000(*) | 2.15507 | .000 |
(p-value up to third decimal space)
Mausner et al., [6], after examining the effect of a 3-step, 2-bottle multipurpose adhesive system, reported that casting retention decreased when resin sealer was used with zinc phosphate, but a similar effect for glass ionomer was not shown. A later study [19] which was done, produced similar results. The results obtained with zinc phosphate were consistant with those of the present study, but the results with glass ionomer were not consistent. It is possible that this 2-bottle bonding system does not demonstrate the beneficial adhesive affect with glass ionomer cement, that isfound with the single-bottle system.
The present study demonstrated an adverse effect when the single-bottle resin primer which was tested was used to seal dentin before cementing it with zinc phosphate, but a very beneficial effect was seen when glass ionomer cement was used. Zinc phosphate attains its retentive qualities by filling irregularities in the prepared dentin and the internal surface of the casting [20]. In 8 out of 10 specimens, the cement resided on the casting when a sealer was used with zinc phosphate. If teeth are prepared in the ideal 6-degree convergence angle, the resistance to crown removal will increase significantly for any cement [21]. The objective of this study was to assess the effect of the sealer on casting retention and to not confound the results by minimizing preparation draw. Thus, a 20-degree angle of convergence was chosen. Of interest from a clinical standpoint was that retentive stress increased significantly for castings which were cemented with glass ionomer after the dentin sealer was used. It has long been postulated that glass ionomer gains a degree of adhesion from ionic interaction of carboxyl ions in tooth structure [22].
Different modes of failure were obtained at different levels, depending upon the type of cement and the bonding between the tooth and the cement and/or between cement and castings [Table/Fig-6]. Group A showed that debonding between cement and castings was about 50%, whereas Group D debonding had reduced to about 46%. Group B showed a mixed mode of failure, where debonding occurred partially between tooth and cement and casting. Group E showed cement which was left principally to tooth surface (about 60%), However, groups C and F showed highest retention among all groups. In 80% of the cases, the crown fractured, which confirmed the best bonding among all other cements [Table/Fig-7].
Different mode of failures for A, B, C, D, E, F
| Failure Mode |
|---|
| 1 | 2 | 3 | 4 |
|---|
| Zinc Phosphate | No. of specimen Percentage | 4 | 3 | 3 | 1 |
| 31.2 | 31.7 | 27.2 | 10 |
| Zinc Phosphate with sealer | No. of specimen Percentage | 1 | 2 | 7 | 0 |
| 11.1 | 12.2 | 76.7 | 0 |
| Glass ionomer | No. of specimen Percentage | 5 | 2 | 1 | 2 |
| 54 | 20 | 11 | 15 |
| Glass ionomer with sealer | No. of specimen Percentage | 6 | 1 | 1 | 2 |
| 62.2 | 4 | 7.6 | 26.2 |
| Modified glass ionomer | No. of specimen Percentage | 0 | 1 | 2 | 7 |
| 0 | 8.1 | 22.8 | 69.1 |
| Modified glass ionomer with sealer | No. of specimen Percentage | 0 | 0 | 2 | 8 |
| 0 | 0 | 20.6 | 79.4 |
Evaluation of the results suggested that the best retention was obtained when castings are cemented by using modified resin cement with or without a sealer. The use of zinc phosphate without a sealer yielded an acceptable retention as strength varied. However, this can lead to post cementation sensitivity. Hence, the use of zinc phosphate luting cement may be restricted to cementation of crowns over endodontically treated teeth. Glass ionomer cement with or without a resin sealer yeilds good retentive bond strength. However, the use of glass ionomer cement in the absence of a sealer may contribute post cementation sensitivity.
Conclusion
On the basis of data and results which were obtained, following conclusions can be drawn from present study. Use of resin based sealers as a desensitizing treatment for tooth preparations reduced crown retention, which was 46% for castings which were cemented with zinc phosphate cement. It is not recommended to use resin based sealers with zinc phosphate cement. Glass ionomer cement without a sealer is less or equivalently retentive than zinc phosphate cement without a sealer. Use of a resin based sealer as a desensitizing agent for tooth preparations, increased crown retention for castings which were cemented with glass ionomer cement, which was nearly equivalent to that of zinc phosphate cement alone. It is advantageous to use resin based sealers when castings are cemented with glass ionomer and modified resin cement, as compared to zinc phosphate and glass ionomer cements, The modified resin cement produced a significantly greater mean of dislodgement stress, which generally exceeding the strength of tooth. Therefore, modified resin cement was the most retentive cement than any other cement which was used in this study. So, this cement is suggested in clinical cases where the tooth is compromised in retention.
(p-value up to third decimal space)