Aim: To study the etiology of rhegmatogenous retinal detachment and visual outcome after retinal detachment surgery.
Materials and Methods: Retrospective study conducted at the tertiary eye care hospital over a period of one year. Thirty eyes of 30 patients were included after fulfilling the inclusion criteria. Complete ocular examination details of each patient such as visual acuity for distant vision (checked with Snellen’s acuity chart),slit lamp examination, fundus examination (done with +90D lens) and binocular indirect ophthalmoscopy. In addition the following were noted: extent of the detachment present, position and number of breaks, status of the macula, presence of PVR, mobility of retina and presence of any peripheral retinal degenerations, and fundus photographs of the patient (before and after surgery).
Results: Risk factors for retinal detachment included myopia in 7 eyes (23.3%), prior cataract surgery in 10 eyes (33.3%), peripheral retinal degeneration in 3 eyes (10%) and traction with new vessels in 1 eye (3.3%). Eighteen eyes (60%) presented with macula off while 12 eyes (40%) presented with macula partly or completely attached. Visual acuity at presentation was <3/60 in 16 eyes. Following surgery, retina was attached in 28 eyes (93.3%) and remained detached in 2 eyes (6.7%). Visual acuity after surgery was <3/60 in 12 eyes.Visual acuity improved in 13 eyes (43.3%), remained the same in 16 eyes (53.3%) and worsened in 1 eye (3.3%).
Conclusion: Myopia and prior cataract surgery are important risk factors for Rhegmatogenous Retinal Detachment. Majority of patients in this setting presented late with Rhegmatogenous Retinal Detachment and this was responsible for relatively poor visual outcomes despite good anatomical results after surgery. Proper screening of eyes at risk and education of patients is important for preventing visual loss due to retinal detachment.
Introduction
The retina is the layer of nerve tissue at the back of the eye, on the inner wall. Retinal detachment is a separation of the neurosensory retina from the underlying retinal pigmented epithelium with accumulation of fluid in the potential space between the two layers. If this happens, vision is affected because the retina is unable to function properly. The types of retinal detachment include rhegmatogenous, tractional and exudative.
Rhegmatogenous retinal detachment (RRD) typically has a corrugated appearance caused by intra-retinal edema. Obviously, they are associated with a retinal break. The main predisposing factors of rhegmatogenous retinal detachments are myopia, previous cataract surgery and lattice degeneration. Currently, approximately half of all primary rhegmatogenous retinal detachments occur in patients with a history of cataract surgery.
Rhegmatogenous retinal detachment occurs when retinal breaks develop at sites of firm vitreoretinal adherence. Following cataract surgery, studies have shown the incidence of RRD to range between 0.6 and 1.7% in the first postoperative year, with an overall incidence of 0.7% [1-4].
Compared with rates of RRD in the general population of 0.0065– 0.01,79% cataract surgery increases the risk of RRD at least four fold [5-6]. Incidence of RRD after ND YAG laser capsulotomy for posterior capsular opacification has been found to be 1.9% world wide [5].
Genetic factors have been cited to influence incidence of RRD. Some studies have shown a relatively high incidence of familial retinal detachment among first relatives [7]. Though rare, Pilocarpine has also been implicated as a cause of retinal detachment especially where other risk factors pre-exist.
Myopia has been shown to be a risk factor for retinal detachment. This risk increases with higher degrees of myopia. Studies have shown PVD occurs early, lattice degeneration is more common, and retina is thinner in myopic patients, making breaks and RRD more frequent and bilateral [8,9].
Trauma has been implicated as a cause of 15% of all retinal detachments with most occurring in young individuals, there is often a latent period between the time of trauma and development of retinal RRD. Studies on location of traumatic retinal breaks revealed 60% are located at the ora, with a similar rate of non-traumatic tears found to be equatorial. The frequent occurrence of retinal breaks, the most important being retinal dialysis, in ocular contusion injury has been documented repeatedly [10].
Options for the treatment are pars plana vitrectomy [11,12], sclera buckling [13], pneumatic retinopexy [14,15] and laser photocoagulation and cryotherapy.
Aim of the Study
To study the etiology of rhegmatogenous retinal detachment and visual outcome after retinal detachment surgery.
Materials and Methods
Retrospective study conducted at the tertiary eye care hospital, Institute of ophthalmology, Joseph eye hospital, Trichy, India over a period of one year, 2012-2013. The protocol of this study was approved by the institutional ethics committee prior to reviewing the patient’s medical records. Informed consents were taken from all the patients prior to the study. Sample size was 30 eyes of 30 patients. The statistical significance was calculated by the Student t-test using SPSS software package for Windows (Version 16.0; SPSS Inc., Chicago, IL, USA). The statistical significance were also calculated by the Student `t’ test Values were considered statistically significant when p < 0.05.
Inclusion Criteria
1. Patients with Rhegmatogenous Retinal Detachment undergoing retinal detachment surgery
2. Patients with at least 2 months follow-up
Detailed information about the history and complaints of the patients were taken. This included the type of visual problems, duration of symptoms and any history of predisposing factors like refractive status, trauma, cataract surgery etc.
Pre operative data includes patient’s demographic details (age, sex,), type of retinal detachment, duration of symptoms, associated risk factors, prior history of surgery and visual acuity at presentation were collected.
Complete ocular examination including details of each patient such as visual acuity for distant vision (checked with Snellen’s acuity chart). Slit lamp examination, fundus examination (done with +90D lens) and binocular indirect ophthalmoscopy. Data regarding surgery performed and any intraoperative complications were also noted. Post operative data included visual acuity, retinal status (whether ‘on’ or ‘off’) and complications following surgery.
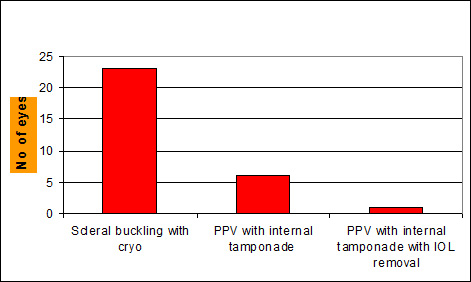
Surgical procedure performed
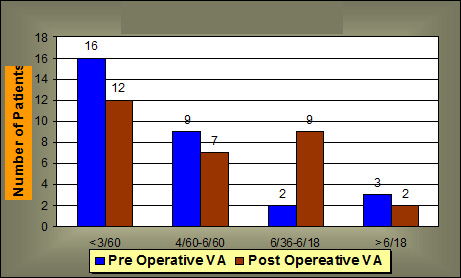
Comparison of VA pre and post opereative
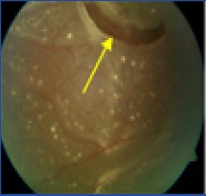
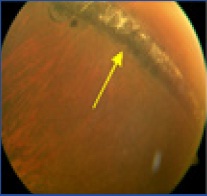
Retinal tear with retinal detachment
Retinal tear after cryopexy
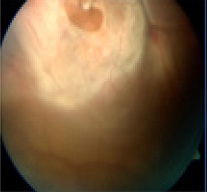
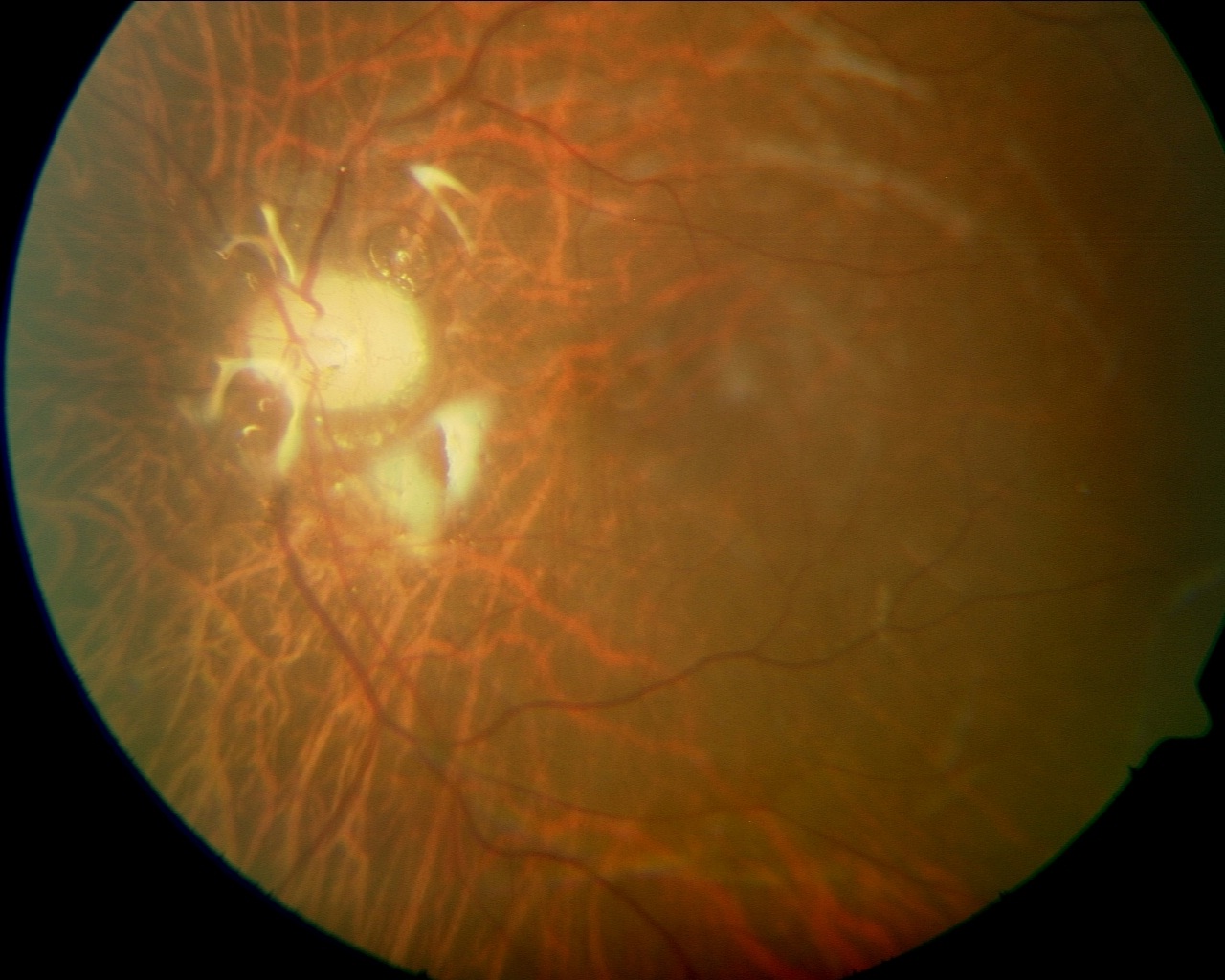
Post-operative silicon oil
Results
Thirty eyes of 30 patients with Retinal Detachment underwent retinal 2detachment surgery were included in the study of this 60% were males, male:female ratio 1.5:1 and 40% females with the range of 12 to 79.
Risk factors for retinal detachment included myopia in 7 eyes (23.3%), prior cataract surgery in 10 eyes (33.3%), peripheral retinal degeneration in 3 eyes (10%) and traction with new vessels in 1 eye (3.3%). Remaining 9 patients has no risk factor of retinal detachment .
Eighteen eyes (60%) presented with macula off while 12 eyes (40%) presented with macula partly or completely attached. Retinal tear was present in 27 eyes (90%) while atrophic holes were present in 3 eyes (10%).
Duration of symptoms was less than 1 week in 4 eyes (13.3%), 1 week to 1 month in 7 eyes (23.3%) and over 1 month in 19 eyes (63.3%). Proliferative vitreoretinopathy (PVR) changes prior to surgery were present in 6 eyes (20%).
Associated findings were vitreous hemorrhage in 2 eyes, choroidal detachment in 1 eye and dislocated IOL in 1 eye. Visual acuity at presentation was <3/60 in 16 eyes, 3/60 to 6/60 in 9 eyes, 6/60 to 6/18 in 2 eyes and 6/12 or better in 3 eyes.
Surgeries performed included Scleral buckling with cryopexy in 23 eyes (76.7%) and pars plana vitrectomy with belt buckling, endolaser and internal tamponade in 7 eyes (23.3%). In 1 eye, this was combined with removal of dislocated IOL and in 2 eyes with lens extraction [Table/Fig-1].
Following surgery, retina was attached in 28 eyes (93.3%) and remained detached in 2 eyes (6.7%).
Visual acuity after surgery was <3/60 in 12 eyes, 3/60 to 6/60 in 7 eyes, 6/60 to 6/18 in 9 eyes and 6/12 or better in 2 eyes. Visual acuity improved in 13 eyes (43.3%), remained the same in 16 eyes (53.3%) and worsened in 1 eye (3.3%) [Table/Fig-2].
Post-operative complications included transient choroidal detachment in 6 eyes, vitreous hemorrhage in 1 eye, fresh break in 1 eye, severe PVR in 2 eyes, transient elevation in IOP in 2 eyes, cataract in 1 eye and epiretinal membrane in 1 eye.
Discussion
This is a retrospective analysis of clinical data of patients underwent RD surgery to find out the predominant etiology of retinal detachment and possible visual outcome after retinal detachment surgery. Medical records of 30 eyes of 30 patients with retinal detachment were analysed. The results reveals that the most common risk factors for RD were myopia and prior cataract surgery, both of which are well-known as risk factors for RD [16,17]. (Ross, Schepens).
Myopia has been shown to be a risk factor for retinal detachment. This risk increases with higher degrees of myopia. Studies have shown PVD occurs early, lattice degeneration is more common, and retina is thinner in myopic patients, making breaks and RRD more frequent and bilateral [8,9].
Myopia has been shown to be a risk factor for retinal detachment. This risk increases with higher degrees of myopia. Studies have shown PVD occurs early, lattice degeneration is more common, and retina is thinner in myopic patients, making breaks and RRD more frequent and bilateral [9,10].
Trauma has been implicated as a cause of 15% of all retinal detachments with most occurring in young individuals, there is often a latent period between the time of trauma and development of retinal RRD. Studies on location of traumatic retinal breaks revealed 60% are located at the ora, with a similar rate of non-traumatic tears found to be equatorial. The frequent occurrence of retinal breaks, the most important being retinal dialysis, in ocular contusion injury has been documented repeatedly [10]. Byer studied retinal breaks associated with peripheral cystic retinal tufts may account for up to 10% of rhegmatogenous detachments [16-19,8]. In our study, peripheral degeneration was present in 10% of eyes with RD. Schepens and Marden reported patients with myopia are at a much higher risk of experiencing rhegmatogenous retinal detachment [18,19] In the present study, myopia accounted for 23.3% of eyes with RD.Haimann et al., reported up to 40 % of retinal detachment occurs in aphakic and pseudophakic eyes [20,7]. Olsen and Olson reported the incidence of retinal detachment is 2 to 5 % after intracapsular cataract extraction, 0 to 3.6 % after extracapsular cataract extraction, and 0.8 to 1.2 % after phacoemulsification. In our study, 33.3% of eyes with RD had prior cataract surgery [21].
Majority of patients presented late (>1 month after onset of symptoms) and had macula off at presentation [Table/Fig-3,4] Late presentation of patients with retinal detachment is one of the important factors responsible for poor visual outcome following retinal detachment surgery [21,22]. PVR changes prior to surgery were present in 20% of eyes and reflect the longstanding nature of the RD in these eyes [16]. Scleral buckling with cryopexy was the most commonly performed surgery for the patients included in the present study [Table/Fig-5,6] . Scleral buckling is relatively inexpensive and is often the surgery of choice for management of retinal detachment in countries such as India where resources are limited. In eyes with PVR, hazy media or posterior breaks, pars plana vitrectomy is the only option available [Table/Fig-7] . Retinal attachment achieved with 1 or more procedures in over 97% of eyes in this. However, visual results were more modest with around 40% of eyes having visual improvement after surgery. One possible reason for this could be late presentation with macula being detached responsible for this limited visual recovery.
Conclusion
It can be concluded from the study that myopia and prior cataract surgery are important risk factors for Rhegmatogenous Retinal Detachment. Majority of patients in this setting presented late with Rhegmatogenous Retinal Detachment and this was responsible for relatively poor visual outcomes despite good anatomical results after surgery. Proper screening of eyes at risk and education of patients is important for preventing visual loss due to retinal detachment.
[1]. MC Kraff, DR Sanders, Incidence of retinal detachment following posterior chamber intraocular lens surgery.J Cataract Refract Surg. 1990 16:477-80. [Google Scholar]
[2]. N Lois, D Wong, Pseudophakic retinal detachment.Surv Ophthalmol. 2003 48:467-87. [Google Scholar]
[3]. JC Erie, ME Raecker, KH Baratz, Risk of retinal detachment after cataract extraction, 1980–2004: a population-based study. Trans Am Ophthalmol Soc. 2006 104:167-75. [Google Scholar]
[4]. SJ Tuft, D Minassian, P Sullivan, Risk factors for retinal detachment after cataract surgery: a case-control study.Ophthalmology. 2006 113:650-56. [Google Scholar]
[5]. L Laatikainen, EM Toippanen, H Harju, Epidemiology of rhegmatogenous retinal detachment in a Finnish population.Acta Ophthalmol (Copenh). 1985 63:59-64. [Google Scholar]
[6]. PV Algvere, P Johnberg, O Textorius, The Swedish Retinal Detachment Register. I: a database for epidemiological and clinical studies.Graefes Arch Clin Exp Ophthalmol. 1999 237:137-44. [Google Scholar]
[7]. MH Haiman, TC Burton, Epidemiology of retinal detachment.Arch Ophthalmology. 1982 100:289 [Google Scholar]
[8]. J Yonemoto, H Ideta, The age of onset of posterior vitreous detachment.Graefes Arch Clin Exp Ophthalmology. 1994 67:232 [Google Scholar]
[9]. J Kaluzny, Myopia and retinal detachment. Pol Med J. 1970 9:1544-49. [Google Scholar]
[10]. GEM Kirker, DJ McDonald, Peripheral retinal degeneration in high myopia.Canada. J Ophthal. 1971 6:58-61. [Google Scholar]
[11]. MS Cox, CL Schepens, HM Freeman, Retinal detachment due to ocular contusion.Arch Ophthalmol. 1966 76:678-85. [Google Scholar]
[12]. JK Gitau, Review of vitreoretinal surgeries done at Kenyatta national hospital. 2009 [Google Scholar]
[13]. C Haritoglou, U Brandlhuber, A Kampic, SG Priglinger, Anatomic success of scleral buckling for rhegmatogenous retinal detachment.Ophthalmologica. 2010 224(5):312-18. [Google Scholar]
[14]. P Girard, I Karpouzas, Visual acuity after scleral buckling surgery.Ophthalmologica. 1995 209(6):323-28. [Google Scholar]
[15]. AA Zaidi, R Alvarado, A Irvine, Pneumatic retinopexy: success rate and complications.Br J Ophthalmol. 2006 90(4):427-28. [Google Scholar]
[16]. WH Ross, Traumatic retinal dialyses.Arch Ophthalmology. 1981 99:1371 [Google Scholar]
[17]. CL Schepens, Retinal detachment and aphakia.Arch Ophthalmology. 1951 1:45 [Google Scholar]
[18]. CL Schepens, D Marden, Data on the natural history of retinal detachment. Further characterization of certain unilateral nontraumatic cases.Am J Ophthalmol. 1966 61:213 [Google Scholar]
[19]. BR Straastma, RY Foos, Typical and reticular degenerative retinoschisis.Am J Ophthalmol. 1973 75:551 [Google Scholar]
[20]. MD Heller, BR Straatsma, RY Foos, Detachment of the posterior vitreous in phakic and aphakic eyes.Mod Probl Ophthalmol. 1972 10:23 [Google Scholar]
[21]. GM Olsen, RJ Olson, Cataract surgery, capsulotomy, and retinal detachment: A prospective study.J cataract Refract surgery. 1995 21:136 [Google Scholar]
[22]. RT Oyakawa, AP SChachat, RG Michels, Complications of vitreous surgery for diabetic retinopathy. Intraoperative complications.Ophthalmology. 1983 90:517 [Google Scholar]