Role of Trans Vaginal Ultrasound and Doppler in Diagnosis of Pelvic Congestion Syndrome
Kaveri Sharma1, Manash Kumar Bora2, Jessy Varghese3, Gaurav Malik4, Robin Kuruvilla5
1Assistant Professor, Department of Obstetrics & Gynaecology, AVMCH,Puducherry, India.
2Associate Professor, Department of Radiology, AVMCH,Puducherry, India.
3Assistant Professor, Department of Obstetrics & Gynaecology, AVMCH,Puducherry, India.
4Post Graduate Student, Radiogiagnosis, Department of Radiology, AVMCH,Puducherry, India.
5Post Graduate Student, Radiogiagnosis, Department of Radiology, AVMCH,Puducherry, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Manash Kumar Bora, Second Floor, Vishram Apatment, Door No.4, S.V. Patel Salai, Puducherry-605001, India.
Phone: 978730091,
E-mail: drmanashbora@yahoo.com
Pelvic congestion syndrome (PCS) is a cause of chronic pelvic pain in women and is defined as pelvic pain lasting for more than six months.The diagnosis of PCS is a challenging task for the gynaecologist. It can be due to many varied causes like endometriosis, adhesions, chronic pelvic inflammatory disease (PID), ovarian cyst, fibroids, pelvic varicosities. Radiology plays an important role in the diagnosis and management of PCS. Pelvic UltraSonography (PUS),transvaginal sonography (TVS) with doppler, Magnetic resonance imaging (MRI), computed tomography (CT) and ovarian venography are usually used in the diagnosis of this condition.
We report a case of a 35-year-old multiparous patient with history of pain in lower abdomen, vaginal discharge and general lethargy for past three years who was diagnosed as a case of PCS based on typical TVS and Doppler findings.
Doppler, Management, Pelvic congestion syndrome, Transvaginal sonography
Case Report
A 35-year-old woman presented with dull aching lower abdominal pain for past three years. She had aggravation of the same during every menstrual cycle and during intercourse. She said the severity of the pain was more by afternoon and localized to supra pubic area and both the iliac fossa. Her menarche was at age of 14 years and menstrual periods were regular at 28 days with flow lasting for three days. Flow was average. She also gave history of increased vaginal discharge which was clear mucoid and without any itching or abnormal smell. Multiple regimes of treatment were given for pelvic inflammatory disease (PID) and dysmenorrhea at different places without any benefit to the patient. At the present visit, she was normotensive with blood pressure of 130/80 mmHg with pulse rate of 72 times/minute.
On inspection,vulva and vagina were normal but per-speculum examination showed a significantly congested and oedematous cervix with visibly congested blood vessels. Increased clear mucoid discharge was noticed. Significant forniceal, uterine and cervical motion tenderness were found on bimanual examination. Laboratory investigations were normal. Based on her symptoms she was sent for ultrasound examination.
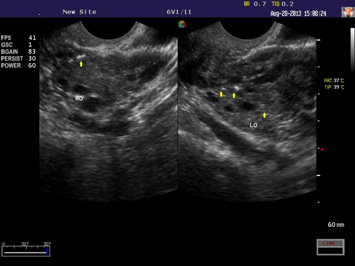
Transvaginal ultrasound with colour doppler showed a normal size of the uterus with endometrial thickness of 8mm. There was gross heterogenicity of the myometrial echotexture having intervening long and tubular anechogenic areas suggestive of blood vessels [Table/Fig-1].
Both the ovaries were normal. Multiple linear and tubular anechogenic areas were noted in both the adnexa and around the ovaries [Table/Fig-2].
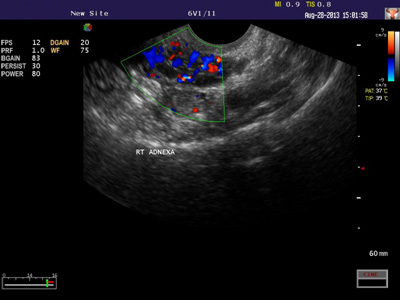
Colour flow doppler study (CFDS) showed multiple dilated veins in both adnexa and ovaries ,average measuring 5 to 6 mm in diameter with slow venous flow of less than 3 cm / second in spectral doppler [Table/Fig-3,4,5,6].
TVS in gray scale imaging shows normal size of uterus and endometrial thickness. Gross heterogenicity of the myometrial echo texture with multiple dilated intra myometrial veins seen

Both the ovaries normal in size and echo texture. Multiple dilated and varicosed veins noted in both the adnexa and around the ovaries
Colour flow doppler study (CFDS) showed multiple dilated veins in right adnexa and right ovary average measuring 5 mm in diameter with slow venous flow
CFDS showed similar finding in left adnexa and left ovary, with further increase in diameter of veins in valsalva menouvere

The uterus revealed multiple dilated intramyometrial veins up to 6 mm in diameter with slow venous flow

Transverse image of uterus and both adnexa together showed multiple dilated and varicosed veins around both ovaries and multiple dilated intra myometrial veins

Discussion
The entity PCS was first introduced by Taylor [1] . PCS is characterized by chronic pelvic pain that gets aggravated on prolonged standing, postural changes, premenstrually and after intercourse [2] . Its etiology remains obscure lacking definitive criteria for diagnosis. PCS is often associated with the presence of ovarian and pelvic varicosed veins [3] . Up to 15 percent of women, usually between the ages of 20 and 50 years, have varicose veins in the pelvis, although not all are symptomatic [4] .
Clinically, such women usually presents with dull aching pelvic pain for more than six months which may have first manifested in pregnancy or postpartum. Bimanual examination may elicit ovarian tenderness along with cervical motion and uterine tenderness. Gluteal, vulvar and thigh varices may also be noted [5] .
PCS occurs when the valves of the ovarian veins become weak and do not close properly. This results in backflow and pooling of blood, causing bulging of veins and pain. It can affect uterus, ovaries or vulva. It has been seen that up to 15% of women between the ages of 20–50 years have varicose veins in the pelvis, although not all are symptomatic [6].
Risk factors associated with PCS are multiparity, associated varices in legs, polycystic ovaries and hormonal dysfunction. Apart from chronic pelvic pain the patient usually complains of menorrhagia, dysmenorrhoea, dyspareunia, increased vaginal discharge and increased urinary frequency and constipation [6,7] . Although there is no definite cause for PCS, it is seen mostly in premenopausal and multiparous women suggesting the possibility of a hormonal aetiology which is further supported by the observation that symptoms are ameliorated with medical ovarian suppression [5] .
As PCS is a diagnosis by exclusion, any other pelvic pathology pertaining to surgical, urology, musculoskeletal or other gynaecological causes needs to be ruled out.
Imaging plays an important role in exclusion of other disorders. PUS and/or CT scan are usually the first imaging modalities in the evaluation of patients with chronic pelvic pain . Both provide excellent resolution of the uterus. Although a CT scan has greater sensitivity for showing varicosities throughout the lower pelvis, PUS and / or TVS with doppler examination provides dynamic information about visualized venous blood flow . It also does not carry any radiation issues. Criteria for the sonographic diagnosis of varices includes (1 ) the visualization of dilated ovarian veins greater than 4 mm in diameter , (2 ) dilated tortuous arcuate veins in the myometrium that communicate with bilateral pelvic varicose veins, (3) slow blood flow (less than 3 cm /s), and reversed caudal or retrograde venous blood flow particularly in the left ovarian vein [8] . All these classical findings were noted in our case.
In PUS, one can observe dilated ovarian veins, regurgitation of venous blood flow, existence of varicosed veins in both adnexa, dilation of spiral vein that passes through uterine myometrium and ovarian polycystic change [9] . In CT examination, delayed and persistent enhancement of the dilated and tortuous adnexal veins are seen. Retrograde venography is often used for PCS diagnosis [6] . PCS is suspected when the ovarian veins are dilated over 10 mm in diameter, there is congestion of uterine veins and ovarian plexus, and the contrast enhances the associated femoral varicosed veins. To increase pressure in patients’ abdomens, retrograde venography is performed under half-standing up posture or valsalva maneuver [6] .
Treatment options include physiotherapy, medical therapy with progestogens, ovarian vessel embolization (OVE), or hysterectomy with or without salpingo-oophorectomy [10] . OVE is indicated for treatment of PCS when she has had a definite diagnosis made at laparoscopy and has failed a trial of appropriate medical therapy. OVE is a minimally invasive alternative treatment for PCS. The technique, usually performed by an interventional radiologist, involves passing a catheter through the groin to the ovarian veins. A clot is formed, which subsequently blocks the accumulation of blood in the varices [11] . Careful selection of patients and use of appropriate angiographic and technical skills by the interventional radiologist are prerequisite for success. Although embolization therapy has low occurrence of complications (less than 4%), still there are ovarian thrombo-vasculitis, varix recurence, transfer of embolic material and radiation exposure of ovaries. However, according to one study, there was no negative influence on menstrual period or fertility [12] .
Conclusion
Although a final radiological diagnosis of PCS is usually done with MRI and ovarian venography, PUS and TVS with Doppler is usually the first modality of examination for its evaluation. The diagnosis of PCS can be made effectively with its typical sonographic and Doppler findings. We conclude that awareness of this disease entity and appreciation of typical sonographic and Doppler findings can lead to an early and accurate diagnosis of the same, thereby potentially reducing the delay in getting the definitive treatment.
[1]. HC Taylor, Jr. Vascular congestion and hyperemia; their effect on function and structure in the female reproductive organs; the clinical aspects of the congestion-fibrosis syndromeAm J Obstet Gynecol 1949 57(4):637-53. [Google Scholar]
[2]. JT Hobbs, The pelvic congestion syndromeBr J Hosp Med 1990 43(3):200-06. [Google Scholar]
[3]. AC Venbrux, DL Lambert, Embolization of the ovarian veins as a treatment for patients with chronic pelvic pain caused by pelvic venous incompetence (pelvic congestion syndrome).Curr Opin Obstet Gynecol 1999 11:395-99. [Google Scholar]
[4]. The International Pelvic Pain Society 2002 [Google Scholar]
[5]. RW Beard, PW Reginald, J Wadsworth, Clinical features of women with chronic lower abdominal pain and pelvic congestionBr J Obstet Gynaecol 1988 95(2):153-61. [Google Scholar]
[6]. AM Rozenblit, ZJ Ricci, J Tuvia, ES Amis, Incompetent and dilated ovarian veins: a common CT finding in asymptomatic parous womenAm J Roentgenol 2001 176:119-22. [Google Scholar]
[7]. A Kennedy, Hemingway A. Radiology of ovarian varicesBr J Hosp Med 1990 44(1):38-43. [Google Scholar]
[8]. FV Coakley, L Varghese S, H Hricak, CT and MRI of pelvic varices in womenJ Com put Assist Tom ogr 1999 23:429-34.[PubMed] [Google Scholar]
[9]. SJ Park, JW Lim, YT Ko, DH Lee, Y Yoon, JH Oh, Diagnosis of pelvic congestion syndrome using trans abdominal and trans vaginal sonographyAJRAm J Roentgenol 2004 182(3):683-88. [Google Scholar]
[10]. MH Chung, CY Huh, Comparison of treatment of pelvic congestion syndromeTohoku J Exp Med 2003 201:131-38. [Google Scholar]
[11]. P Capasso, C Simons, G Trotteur, RF Dondelinger, D Henroteaux, U Gaspard, Treatment of symptomatic pelvic varices by ovarian vein embolisation.Cardiovasc Intervent Radiol 1997 20:107-11. [Google Scholar]
[12]. HS Kim, AD Malhotra, PC Rowe, JM Lee, AC Venbrux, Embolotherapy for pelvic congestion syndrome: long term resultsJ Vasc Interv Radiol 2006 17(17(2 Pt1)):289-97. [Google Scholar]