Introduction
Acid etch technique was introduced by Buonocore in 1955 herald a new era in adhesive dentistry. In orthodontic treatment, various attachments are bonded on the tooth surface in order to move the teeth. Direct bonding of orthodontic appliances to enamel with composite resin was first introduced by Newmanand it is most accepted and widely all over world. The objective of debonding is to remove these attachments from the tooth surface and restore the tooth surface as closely as possible to its pre-treatment condition without any iatrogenic damage. To obtain these objectives, a correct technique is of fundamental importance because debonding is time consuming and damaging to the enamel if performed with improper technique or in an unskillful manner [1,2].
During the early 1970s, composite brackets were marketed as the esthetic alternative to metal brackets. Such composite brackets may be useful in minimal force situations and for treatment of short duration, particularly in adults. These brackets quickly lost favour because of fracture, deformation, discoloration, slot distortion caused by water absorption and lower torque expressions[3].
In the mid-1980s, the first brackets made of monocrystalline sapphire and polycrystalline ceramic materials became widely available. Ceramic brackets, unlike composite brackets, resist staining and slot distortion and are chemically inert to fluids that are likely to be ingested. But, ceramic brackets also have various disadvantages like inability to form chemical bonds with adhesives without a coupling agent, a low fracture toughness, that is, brittleness that can cause the bracket to fracture while debonding, and an increased frictional resistance between metal arch wires and ceramic brackets [4].
Because of the inert composition of the aluminum oxide from which the ceramic brackets are made, chemical cohesion between the ceramic base and the adhesive resin is not possible. Consequently, the early ceramic brackets used a silane coupler to act as a chemical mediator between the ceramic bracket base and the diacrylic or acrylic adhesive resin. Chemical retention resulted in an extremely strong bond that caused the enamel-adhesive interface to be stressed during debonding [5,6].
Debonding of metallic brackets is easy but as discussed above when composite and ceramic brackets were introduced, debonding of these brackets became difficult. So, to reduce the irreversible enamel surface damage, several methods of debonding ceramic brackets have been suggested. These methods include the conventional methods that use pliers or wrenches, an ultrasonic method that uses special tips, and electrothermal devices that transmit heat to the adhesive through the bracket, air pressure impulse devices which is common for crown removal in prosthodontics, diamond burs to grind the brackets off the tooth surface, and lasers [7,8].
Although all methods have been used successfully to debond brackets, using pliers to apply a shear or tensile force to the bracket is the most clinically convenient method. The removal of most composite and ceramic brackets is accomplished by specially designed pliers that apply some form of tensile or shear force to the tooth surface[6].
In orthodontic literature, one of the most popular mechanical debonding techniques involves application of a slow, squeezing force to the bracket, with the blades of the debonding pliers at the enamel surface and within the adhesive. The debonding pliers are unique because the force is applied at the bracket-adhesive interface on both sides of the bracket base simultaneously. Several studies have reported no enamel damage when debonding ceramic brackets with the appropriate pliers [9,10].
In an effort to reduce the forces placed on the enamel surface and decrease the likelihood of enamel damage, various debonding techniques using conventional pliers have been tested. More recently, a manufacturer introduced a new “Debonding Instrument” to be used specifically for ceramic brackets, being a relatively new product, a little information is available on the efficacy and debonding characteristics of this new instrument.
The present study has been conducted to evaluate and compare the debonding characteristics between the conventional debonding pliers (Jaypee General Agencies) and the new debonding instrument (Unitek 3M,Monrovia, CA) on debonding of ceramic, composite and metallic brackets.
Materials and Methods
A total of 138 freshly extracted human maxillary premolar teeth were collected and were stored in 0.2% (wt/vol) thymol. Only those teeth were selected which were free of caries, had intact buccal enamel and had not been pretreated with chemical agents (eg, H2O2). The teeth were embedded in dental stone (Kalstone, Kalabhai) poured in plastic moulds.
The teeth were randomly assigned to 1 of two Groups, namely, Group A and Group B having 69 teeth each based on type of debonding pliers to be used: Conventional Debonding Pliers (Jaypee General Agencies) [Table/Fig-1] and New Debonding Instrument (Unitek 3M,Monrovia, CA)[Table/Fig-2] respectively. Groups A and B were further divided into 3 subGroups (23 teeth each) namely A1, A2, A3 and B1, B2, B3 according to the types of brackets to be bonded. In subGroup A1 and B1, stainless steel pre-coated maxillary premolar brackets (APC Plus Victory series, Unitek 3M, Monrovia, CA) were used. In subGroup A2 and B2, ceramic pre-coated maxillary premolar brackets (APC Plus Clarity Series, Unitek 3M,Monrovia, CA) were used. In subGroup A3 and B3, composite pre coated maxillary premolar brackets (APC Captain Ortho, Liberal) were used.
Bonding Procedure
After mounting, the teeth were cleaned and polished with pumice (Neelkanth Minechem) and rubber prophylactic cups for 10 seconds. All the teeth were acid etched using 37% phosphoric acid (Unitek 3M,Monrovia, CA) for 15 seconds. After acid etching, the teeth were washed with water spray for 10 seconds and then air dried with oil free air spray. Single coat of Transbond XT bonding agent (Unitek 3M,Monrovia, CA) was applied on the enamel surface. The bonding agent was then lightly sprayed using compressed air for 1-2 seconds and was then light cured by using LED light curing unit (Coltolux® LED). Each pre-coated bracket was placed on the tooth and a 300 g force was applied by using dontrixguage (Orthocraft) for 10 seconds. The force gauge was used to help ensure a uniform adhesive thickness between the bracket and enamel. The bracket was then light cured using a LED light curing unit (Coltolux® LED) for 20 seconds (10 seconds from each proximal side). Types of brackets bonded on teeth in each subGroup are as the following:
After bonding, all teeth were stored in distilled water for 1 week before debonding. After the brackets were debonded, the enamel surface of each tooth was examined under 10x magnification. An adhesive remnant index (ARI) will be used to quantify the amount of remaining adhesive on each tooth.
Group A1
The stainless steel brackets were debonded according to the manufacturer’s directions using the conventional debonding pliers(Jaypee General Agencies). The tips of the pliers were placed over the mesial and distal ends of the metal-lined arch wire slot. The tie wings were then squeezed gently until the bracket collapsed and separated. It is critical that the tips of the pliers be placed over the ends of the metal slot and not over the bracket base.
Group A2
The ceramic brackets were debonded with the conventional debonding pliers using the same procedure as in Group A1.
Group A3
The composite brackets were debonded with the conventional debonding pliers using the same procedure as in Group A1.
Group B1
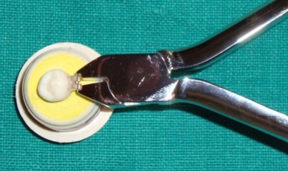
The stainless steel brackets were debonded according to the manufacturer’s directions using New Debonding Instrument (Unitek 3M,Monrovia, CA). The instrument was positioned symmetrically against the mesial and distal sides of the bracket and in contact with the labial surface of the bracket to optimize the contact area. The instrument was squeezed until the bracket collapsed, and then gently rocked in the mesial and distal directions until the bracket was separated from the enamel.
Group B2
The ceramic brackets were debonded with the New Debonding Instrument using the same procedure as in Group B1.
Group B3
The composite brackets were debonded with the New Debonding Instrument using the same procedure as in Group B1.
Modified Adhesive Remnant Index [Table/Fig-5].
After the brackets were debonded, the enamel surface of each tooth was examined under 10 magnification stereo microscope (Lynx, Lawrence and Mayo). A modifiedadhesive remnant index (ARI) was used to quantify the amount of remaining adhesive on each tooth using the following scale: 1: all the adhesive remained on the tooth; 2: more than 90% of the adhesive remained on the tooth; 3: between 10% and 90% of the adhesive remained on the tooth; 4: less than 10% of the adhesive remained on the tooth; and 5: no adhesive remained on the tooth.
Statistical Analysis
The data obtained was subjected to statistical analysis with the consult of a statistician. The data so obtained was compiled systematically. A master table was prepared and the total data was subdivided and distributed meaningfully and presented as individual tables along with graphs. Statistical tests employed for the obtained data in the present study was Chi-Square (c2) test.
Statistical procedures were carried out in 2 steps:
Data compilation and presentation
Statistical analysis
Statistical analysis was done using Statistical Package of Social Science (SPSS Version 15; Chicago Inc., USA). Data comparison was done by applying specific statistical tests to find out the statistical significance of the comparisons. Quantitative variables were compared using mean values and qualitative variables using proportions. Significance level was fixed at p < 0.05.
Results
In the present study, by using modified ARI, debonding characteristics of conventional and new Debonding Pliers, their discrete effectiveness, for brackets too, were evaluated and compared.
[Table/Fig-6,7] described overall results, the ascending order of the debonding efficiency of the New Debonding Instrument (Unitek 3M, Monrovia, CA) with ceramic, metal and composite brackets, being most efficient debonding of composite brackets and least for ceramic brackets.
[Table/Fig-8] Elaborated results of the New Debonding Instrument for debonding of metal brackets were statistically significantly different (p = 0.04) from the results of Conventional Debonding Pliers. The modifiedARI scores suggested that New Debonding Instrument was better than Conventional Debonding Pliers for the debonding of metal brackets.
[Table/Fig-9]illustrated results of the New Debonding Instrument for debonding of ceramic brackets were statistically significantly different (p = 0.05) from the results of Conventional Debonding Pliers. The modifiedARI scores were suggestive that New Debonding Instrument was better than Conventional Debonding Pliers for the use of ceramic brackets.
[Table/Fig-10] depicts results of the New Debonding Instrumentfor bracketdebonding of composite brackets were statistically significantly different (p = 0.02) from the results of Conventional Debonding Pliers. The modifiedARI scores inferred that New Debonding Instrument was better than Conventional Debonding Pliers for the debonding of composite brackets.
Debonding by Conventional Debonding Plier (Jaypee General Agencies) (occlusal view).

Debonding by New Debonding Instrument (3M, Unitek) (occlusal view)
View of bracket after debonding with Conventional Debonding Pliers (Jaypee General Agencies): (a) metal bracket, (b) ceramic bracket, (c) composite

View of bracket after debonding with New Debonding Instrument (3M Unitek): (a) metal bracket, (b) ceramic bracket, (c) composite bracketdebonding

View of adhesive remnant under stereomicrocope (10X magnification)

Frequency distribution of the modified ARI scores for the debonding of metal, ceramic and composite brackets using Conventional Debonding Pliers (Jaypee General Agencies)
| Suitable title | χ2 | p-value |
| 0 | 1 | 5 | 7 | 20 | 21 |
| Groupsn (%) | Metalic brackets (A1) | 3 | 0 | 1 | 0 | 0 | 1 | 7.286 | 0.05* |
| Ceramic brackets (A2) | 2 | 1 | 0 | 1 | 1 | 0 |
| Composite brackets (A3) | 2 | 1 | 1 | 0 | 0 | 1 |
Test applied- chi-square test; *statistically significant
Frequency distribution of the modified ARI scores for the debonding of metal, ceramic and composite brackets using New Debonding Instrument (Unitek 3M, Monrovia, CA)
| Suitable title | χ2 | p-value |
| 0 | 1 | 2 | 3 | 5 | 8 | 10 | 11 | 21 |
| Groupsn (%) | Metallic brackets (B1) | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 15.500 | 0.001* |
| Ceramic brackets (B2) | 2 | 1 | 0 | 1 | 0 | 0 | 0 | 1 |
| Composite brackets (B3) | 1 | 0 | 2 | 0 | 0 | 0 | 1 | 1 | 0 |
Test applied- chi-square test; *statistically significant
Frequency distribution of the modified ARI scores forthe debonding of metal brackets using New Debonding Instrument (Unitek 3M, Monrovia, CA) and Conventional Debonding Pliers (Jaypee General Agencies)
| Groups n (%) | Adhesive Remnant Index (ARI ) scores |
| 0 | 2 | 5 | 8 | 10 | 21 | Total | p value |
| utility | 3 (30) | 0 | 1 (10) | 0 | 0 | 1 (10) | 5 (50) | 0.04* |
| 3M | 1(10) | 1(10) | 1(10) | 1(10) | 1(10) | 0 | 5 (50) |
| Total | 4 (40) | 1 (10) | 2 (20) | 1 (10) | 1 (10) | 1 (10) | 10 (100) |
Test applied- chi-square test (χ2=4); *statistically significant
Frequency distribution of the modified ARI scores and debonding of ceramic brackets using New Debonding Instrument (Unitek 3M, Monrovia, CA) and Conventional Debonding Pliers (Jaypee General Agencies)
| Groups n (%) | Adhesive Remnant Index (ARI ) scores |
| 0 | 1 | 3 | 7 | 20 | 21 | Total | p value |
| utility | 2 (20) | 1 (10) | 0 | 1 (10) | 1 (10) | 0 | 5 (50) | 0.05* |
| 3M | 2 (20) | 1(10) | 1(10) | 0 | 0 | 1 (10) | 5 (50) |
| Total | 4 (40) | 2 (20) | 1 (10) | 1 (10) | 1 (10) | 1 (10) | 10 (100) |
Test applied- chi-square test (χ2=4); *statistically significant
Frequency distribution of the modified ARI scores and debonding of composite brackets using New Debonding Instrument (Unitek 3M, Monrovia, CA) and Conventional Debonding Pliers(Jaypee General Agencies)
| Groups n (%) | Adhesive Remnant Index (ARI ) scores |
| 0 | 1 | 2 | 5 | 10 | 11 | 21 | Total | p value |
| utility | 2 (20) | 1 (10) | 0 | 1 (10) | 0 | 0 | 1 (10) | 5 (50) | 0.02* |
| 3M | 1(10) | 0 | 2 (20) | 0 | 1 (10) | 1 (10) | 0 | 5 (50) |
| Total | 3 (30) | 1(10) | 2 (20) | 1 (10) | 1 (10) | 1 (10) | 1 (10) | 10 (100) |
Test applied- chi-square test (χ2=7.33 ); *statistically significant
Discussion
Introduction of ceramic brackets has created two new clinical challenges for the orthodontist. First, the adhesion between the resin and the ceramic bracket bases has increased to a point where the most common site of bond failure during debonding has shifted from the bracket base-adhesive interface to the enamel adhesive 55interface. This shift has led to an increase in the incidence of bond failures within the enamel surface. Secondly, ceramic brackets are extremely rigid and brittle, so less energy is necessary to cause a fracture of the bracket as compared with that of stainless steel [4,11].
The potential for enamel fractures, cracks and bracket fracture following debonding raises questions about the safety of the procedures used to remove ceramic and composite brackets. Techniques used during debonding of conventional stainless steel orthodontic attachments may be inappropriate for removal of ceramic and composite brackets because the properties of these brackets differ greatly from those of the conventional metal orthodontic brackets. So, there is a need for a safer and more reliable method of debonding thesebrackets [4].
So, several methods of debonding ceramic and composite brackets have been suggested. These methods include the conventional methods that use pliers or wrenches, an ultrasonic method that uses special tips, electrothermal devices that transmit heat to the adhesive through the bracket, air pressure impulse devices which is common for crown removal in prosthodontics, diamond burs to grind the brackets off the tooth surface, and lasers [11].
The ultrasonic debonding technique, which was originally developed for removing cast metal, bridge retainers, has also been found to be useful in removing metal and ceramic orthodontic brackets. It minimizes the potential for bracket failure as well as the trauma to the enamel surface during debonding. Studies have reported no bracket breakage when using the ultrasonic instrument to remove them, whereas 10% to 35% broke when using pliers or torsional wrenches. However, the time required to remove brackets with the ultrasonic instrument is long, 38 to 50 seconds, compared with that required with pliers, one second and some amount of scratches were reported on enamel in some studies [12,13].
Electrothermal debonding (ETD) is one of the method of bracket removal that has been developed to overcome the problems of bracket failure, enamel damage and high forces when debonding orthodontic brackets. The electrothermal debracketing instrument transfers heat through the bracket, allowing bond failure at the bracket-adhesive interface as the heat deforms the adhesive. Marissa Louise stated that ETD techniques have not been found to be totally safe. Problems include risks of injury to the pulp. However, the potential for pulpal damage using ETD on ceramic brackets still needs assessment [14].
Air pressure impulse debonding provides a good alternative to conventional debonding methods as the adhesion is usually separated at the bracket-adhesive interface, thereby avoiding enamel damage, independent of the adhesive used. Michael Kno¨sel stated that all brackets removed with the impulse device are reusable, that is, intact according to the evaluation criterion, as compared to almost 46% of the brackets removed with the removal pliers are not. However, some proportions of enamel damage were seen for impulse debracketing also [7].
Another method is grinding the brackets off the tooth surface by using diamond burs. The gross removal of residual composite left on the enamel surface after grinding of bracket is thought to be best accomplished with a tungsten carbide bur. Çaöry ulusoyl and Sacha Ryf,stated that this method using different rotary finishing instruments is laborious and is associated with subsequent enamel damage and a loss of up to 19.2 mm of enamel [12,13].
Orthodontists have found various uses for lasers, including the debonding of brackets. Laser energy degrades the adhesive resin used to bond brackets by thermally softening it. Consequently, lower forces can be used than when mechanical debonding is performed, reducing the risk of enamal damage. Ezz Azzeh, Ezz Azzehand Mehmet Oguz stated that the conversion of laser light to heat can also threaten the vitality of the debonded teeth by damaging the tooth pulp. Selecting the appropriate laser, resin, and bracket combination can minimize risks and make debonding more efficient.Pilot studies and computer modeling suggest that for commonly used polycrystalline brackets debonded with the carbon dioxide laser, some form of mechanical assistance is needed during the lasing process to keep the intrapulpal temperature below the 5.5° C safety threshold [8,15,16].
Although all these methods can be used successfully to debond brackets, the use of pliers to apply a shear or tensile force on the bracket is perhaps the most convenient and continues to be the most popular method used for debonding brackets [4,6].
Swartz recommended that ceramic brackets should be debonded with a sharp edged instrument placed at the enamel-adhesive interface and a “slow gradual squeezing” force should be applied until bracket failure occurs. As Swartz explained, “ The pliers work either through the deformation of the bracket breaking the bond at the bracket-adhesive interface or by stressing the adhesive to its ultimate strength causing cohesive failure within the composite resin [4].
For debonding ceramic brackets, the use of pliers with narrow blades created sufficient debonding strength and led to reduced force levels on the enamel surface. Bishara et al., reported that debonding polycrystalline ceramic brackets with sharp-edged debonding pliers that apply a bilateral shearing force does not produce any gross enamel damage. Forces applied at the interface rather than the bracket itself may prevent breakages on debonding[6,11,17].
While some studies have reported no enamel damage when debonding ceramic brackets with the appropriate pliers, other researchers have reported an increase in enamel cracks or crack length following debonding [9-11].
In an effort to reduce the forces placed on the enamel surface and decrease the likelihood of enamel damage, various debonding techniques using conventional pliers have been tested. More recently, a manufacturer has introduced a new “Debonding Instrument” to be used specifically for ceramic brackets. It is designed to engage the tie wings of ceramic brackets. Being a relatively new product, a little information is available on the efficacy and debonding characteristics of this new instrument. In the present study, this new debonding instrument and conventional debonding pliers were used to debond the ceramic, composite and metallic brackets so that their debonding efficiency could be evaluated and compared with each other for the debonding of all the three types of brackets.
In this study, the results showed that the debonding efficiency of the new debonding instrument was better than that of the conventional debonding pliers for ceramic, composite and metallic brackets. Similar results were obtained by Adam Ostby for debonding of ceramic brackets. On the contrary, he found that the new pliers did not offer a significant advantage when used to debond metal brackets [4].
In our study, modified ARI was used to evaluate the debonding characteristics of both the pliers. Many studies have used this method, current to the time, for measuring residual adhesive resin after removal of orthodontic attachments. It is a reliable method. Quantitative measurements of the adhesive remnant after debonding can be can be performed by various methods like inspecting with eyes, scanning the cast, judging the photographs and visualising with stereo microscope. A quantitative measurement of adhesive remnant by visualising with stereo microscope is the most reliable method. So this method had been used in our study [18].
In this study, when the debonding was done using Conventional Debonding Pliers (Jaypee General Agencies), the results indicated that the distribution of modified ARI scores ranged between 4 and 5 for metallic, ceramic and composite brackets. But when the debonding was done using New Debonding Instrument (Unitek 3M, Monrovia, CA) the results indicate that the distribution of modified ARI scores ranged between 1 and 3 for metallic, ceramic and composite brackets. This indicate that the failure occurs mostly at or just close to the adhesive enamel interface when the debonding is done with Conventional Debonding Pliers (Jaypee General Agencies) whereas in case of debonding with New Debonding Instrument (Unitek 3M, Monrovia, CA), the failure occurs mostly within the adhesive or at the adhesive bracket base interface. Therefore, the debonding efficiency of New Debonding Instrument (Unitek 3M, Monrovia, CA) is better than the debonding efficiency of Conventional Debonding Pliers (Unitek 3M, Monrovia, CA), for use of metal, ceramic and composite brackets.
In the present study, the results showed that the modified ARI scores between 1 and 2 were maximum for composite brackets and minimum for ceramic brackets among metallic, ceramic and composite brackets. This indicate that the New Debonding Instrument (Unitek 3M, Monrovia, CA) is most effective for composite brackets, followed by metal brackets and least effective for ceramic brackets.
Conclusion
The debonding efficiency of New Debonding Instrument (Unitek 3M, Monrovia, CA) is better than the debonding efficiency of Conventional Debonding Pliers (Jaypee General Agencies), for use of metal, ceramic and composite brackets. The New Debonding Instrument (Unitek 3M, Monrovia, CA) is most effective for composite brackets, followed by metal brackets followed by ceramic brackets.
Test applied- chi-square test; *statistically significant
Test applied- chi-square test; *statistically significant
Test applied- chi-square test (χ2=4); *statistically significant
Test applied- chi-square test (χ2=4); *statistically significant
Test applied- chi-square test (χ2=7.33 ); *statistically significant