Root canal therapy has provided dentistry with the ability to retain the teeth that just a few decades ago would have been extracted without hesitation. However, endodontically treated teeth are considered to be more susceptible to fracture than vital teeth. After the completion of endodontic treatment, restoration and protection of the remaining tooth structure is compulsory.
Non-restored, endodontically treated teeth are more prone to coronal leakage and fracture, which can lead to bacterial contamination and even failure of root canal therapy. Numerous clinical studies have shown that 11%- 13% of extracted teeth with endodontic treatment are associated with vertical root fractures [1]. The reason often cited is removal of tooth structure during endodontic treatment and dehydration of dentin. The major goal of endodontic therapy should be reinforcement of the residual tooth structure [2]. Since the retention of an adhesive restoration is based on micromechanical retention and does not require macro-retentive elements, minimal invasive preparation with maximal conservation of dentinal tissue can be realized. Coronal reinforcement of the tooth has been demonstrated through bonded restorations.
Thus there is a need for different materials and/or techniques to overcome the shortcomings of current endodontic filling materials such as guttapercha or resilon to reinforce roots that is known as intra-orifice barriers. Intra-orifice barrier is an efficient alternative method to decrease coronal leakage in endodontically treated teeth [3]. This procedure includes placing additional material into the canal orifices immediately after removal of the coronal portion of gutta-percha and sealer [4]. Swartz et al., stated that “failure rate of endodontically treated teeth was almost double in cases without adequate post endodontic restoration” [5].
The aim and objective of this study is to compare and evaluate the fracture resistance of roots obturated with guttapercha using bonded amalgam, GC Light cure GIC (resin modified glass ionomer cement) and Tetric N Flow (flowable hybrid composite) as different Intra orifice barriers.
Materials and Methods
1. Selection of Specimens
Human single canal mandibular premolars extracted for orthodontic purposes were collected from the department of Oral & Maxillofacial Surgery, Yenepoya Dental College, Mangalore, Karnataka, India.
Inclusion Criteria: Eighty freshly extracted mandibular premolars selected on the basis of their macroscopically similar size and straight roots reduce to 14 mm from the coronal aspect.
Exclusion Criteria: Teeth with fracture, craze lines and curved roots excluded.
2. Specimen Preparation
Soft tissue & calculus were mechanically removed from the root surface of 80 selected specimens [Table/Fig-1]. The teeth were reduced to 14 mm from the coronal aspect to standardize the specimens. After that all specimens were examined under a stereo- microscope to ensure the absence of cracks. A size 10 K-type file was placed into the canal until it was visible at the apical foramen. The working length was established 1 mm short of this length.
80 selected mandibular premolars were arranged

3. Canal Preparation
The root canals instrumentation done with 0.06 taper Hero shaper rotory files in conjunction with RC-Prep lubrication and 2ml of 5.25% sodium hypochlorite irrigation between each files. All canals enlarged to ISO size 30 to the working length [Table/Fig-2]. The root canals had a final irrigation of 5 ml 17 % EDTA and 5 ml 2.5% NaOCl, after which the canals flushed with distilled water to avoid the prolonged effect of EDTA (RC- Prep) and NaOCl. The canals subsequently dried with paper points.
Root canals were cleaned and shaped with rotory instruments

4. Canal Obturation
The root canal of each tooth was dried with paper points. AH plus sealer was mixed according to the manufacturer’s instructions. Root canal was coated with sealer and obturated with guttapercha cones of 0.06 taper single cones.
5. Placement of Intra Orifice Barriers
Except for control group specimens the coronal 3 mm of root fillings of all other group specimens removed with the aid of heated finger plugger and verified with the help of william’s periodontal probe. Obturated specimens divided with respect to the intra orifice barrier material placed over the root canal fillings into the following groups.
GROUP 1: NO BARRIER (CONTROL)
In this group, there were no removal of gutta-percha and no placement of intra-orifice barriers.
GROUP 2: FUJI GC LC GIC
The specified amounts of powder and liquid dispensed onto the paper pad in the ratio of 3:1, then divided the powder into two equal parts. Mixed the first portion into the liquid with agate spatula and added the second portion into the remaining liquid. Mixed GIC (FUJI GC RESIN MODIFIED GIC) placed into the canal orifices and it was cured for 20 seconds with Blue phase C5 curing light (Ivoclar Vivadent).
GROUP 3: Tetric n Flow
Prior to the restoration with composite, the root canal orifices were etched with 37% phosphoric acid (scotch bond etchant) for 15-20 sec. Then the surface was rinsed with water and the excess water was removed with an air syringe. Then the Adper Single bond 2(3M) adhesive was applied to enamel and dentine and was light cured for 10 sec. Finally placed the flowable hyrid composite (Ivoclar vivadent) and cured for 20 sec.
GROUP 4: Bonded Amalgam
Prior to the restoration with amalgam, mixed the equal amounts of ED PRIMER II A and B (Kuraray), applied with super fine microbrushes on the canal orifices and waited for 30 sec and air dried it. Then dispensed the equal amounts of Panavia F2.0 (Kuraray) luting paste A & B mixed and placed into root canal orifices. Then the amalgam was triturated in an amalgamator and the condensation was commenced immediately. Removed the excess cement and cured for 20 sec. The specimens of all groups were stored at 37oC and 100% humidity for one week to allow the materials to set completely.
6. Fracture Strength Test
The apical root ends were embedded along their long axis in self-curing acrylic blocks, prepared from Leukhardts L-pieces mould leaving 9 mm of each root exposed [Table/Fig-3]. Thereafter, the specimens were mounted in a universal testing machine [Table/Fig-4] (Manipal college of dental sciences, manipal). A custom stainless steel loading fixture with a 2-mm spherical tip was centered over the canal opening [Table/Fig-5]. A compressive force was applied at a crosshead speed of 1 mm/min until fracture occurred. The forces necessary to fracture each root were recorded in newtons (N). The mode of failure for each of the specimens was noted by visual inspection.
Tooth mounted in a self cure acrylic block

Universal testing machine

Mounted tooth kept on universal testing machine for fracture resistance

Statistical Analysis
Data was analysed for significance by Analysis of Variance (ANOVA) and further pair wise comparison was performed by Bonferroni test. Level of significance was taken as 0.05.
Results
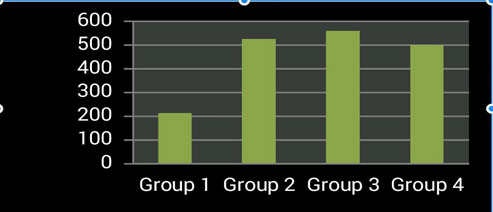
Mean strength of Group 1 was 212.9±55.9, Group 2 was 525.25±66.4, Group 3 was 560.5±75.4 and that of Group 4 it was 500.1±77.8 respectively. Mean of Group 1 is least followed by Group 4, Group 2 & Group 3. ANOVA tests shows that there is significant difference as p=0.000<0.01. Further post hoc test was performed by Bonferroni tests, showed that Group I is significantly less as compared to Group II, Group III & Group IV. (p<0.01).Whereas Group II with Group III and Group IV, there is no significant difference (p>0.05). Group III shows significant difference with IV (p<0.05). Group III is having better fracture resistance as compared to all other groups and Group I is worst among the groups. Results are shown in tables & graph [Table/Fig-6,7,8].
Fracture esistance of each group in newtons (N)
| Group 1 (Control) | Group 2 (Fuji Gc light cure GIC) | Group 3 (Tetric N Flow) | Group 4 (Bonded Amalgam) |
|---|
| 1 | 130 | 398 | 501 | 492 |
| 2 | 228 | 527 | 539 | 455 |
| 3 | 197 | 550 | 511 | 535 |
| 4 | 217 | 490 | 492 | 521 |
| 5 | 210 | 553 | 485 | 540 |
| 6 | 170 | 521 | 639 | 467 |
| 7 | 211 | 512 | 702 | 508 |
| 8 | 220 | 517 | 367 | 527 |
| 9 | 190 | 560 | 551 | 508 |
| 10 | 234 | 505 | 628 | 517 |
| 11 | 232 | 607 | 690 | 251 |
| 12 | 234 | 580 | 545 | 540 |
| 13 | 191 | 601 | 560 | 589 |
| 14 | 386 | 495 | 567 | 498 |
| 15 | 180 | 594 | 602 | 518 |
| 16 | 201 | 350 | 581 | 498 |
| 17 | 137 | 525 | 578 | 571 |
| 18 | 228 | 461 | 523 | 534 |
| 19 | 160 | 605 | 544 | 350 |
| 20 | 302 | 554 | 605 | 583 |
| Mean* | Std. Deviation |
|---|
| Group 1 | 212.9 | 55.9 |
| Group 2 | 525.25 | 66.4 |
| Group 3 | 560.5 | 75.5 |
| Group 4 | 500.1 | 77.8 |
Result shown as graphical representation
Discussion
Growing attention has been given to procedures carried out after completion of endodontic treatment as well as their impact on the prognosis of non-vital teeth. But there is no difference in moisture content found between endodontically treated teeth and vital teeth [6].
According to Dietschi et al., [7], the tooth strength is reduced in proportion to coronal tissue lost due to either carious lesions or restorative procedures. There is a connecting link between the amount of remaining tooth structure and its ability to resist occlusal forces [8]. Therefore, it’s very important to provide a restoration after completion of root canal treatment for avoiding fracture of tooth. Several other factors also affect the fracture resistance of teeth are: amount of tissue lost and its location [9,10], magnitude and duration of load [8], tooth type, direction of applied load and slope of the cuspal inclines [9,11].
A study evaluated the relationship between the quality of both the coronal restoration and the root canal filling by examining the radiographs of endodontically treated teeth [12]. They concluded that apical periodontal health depended more on coronal restoration than on the technical quality of endodontic treatment. A perfect restoration to the periapical health is important and confirmed in previous studies [13–16].
Several studies have shown that applying force to the long axis of the tooth transmits the force uniformly [17–19]. In the present study, the force was also applied vertically in a constant speed using a Universal Testing Machine.
Materials used as intra-orifice barriers are resin modified GIC, flowable composite, amalgam, calcium enriched cement, MTA and Cavit in previous studies [20–23]. Although bonded restorative materials might increase the fracture resistance of root filled teeth [24,25]. In this study materials used are bonded amalgam, resin modified GIC and flowable composite based on chemical adhesion to the tooth structure. Both MTA and Calcium enriched cement (CEM) showed good sealing capacity [3] but having least physical properties, so they are not used in this study.
Resin modified GIC (RMGIC) was introduced in the late 1980, it contains some methacrylate components common in resin composites. It showed superior performance as an acceptable coronal seal over 90 d [26] reported by Tselnik et al., due to the superior performance of RMGIC explained by water sorption by the material, resulting in setting expansion and consequently a better seal is achieved. RMGIC requires no pre-treatment of dentin and can adhere to it and another useful property of RMGIC is the release of fluoride [27].
Resin modified GIC have high flexural strength and modulus of elasticity, and modulus of elasticity values that are similar to dentin, material can withstand large amounts of stress before transmitting the load to the root [28]. This explains that in this study RMGIC (Fuji GC LC GIC) showed no significant difference in fracture resistance as compared to flowable composite (Tetric N Flow) and bonded amalgam, having good fracture resistance as compared to control group and bonded amalgam but less than that of flowable composite [29,30].
Flowable composites are low-viscosity composite resins, making them more fluid than conventional composite resins. Tetric N Flow is a light-curing, radiopaque, flowable nano-hybrid composite (technical product profile) [31]. They are claimed to offer higher flow, better adaptation to the internal cavity wall, easier insertion and greater elasticity [32] than conventional composites. The universal hybrid composites provided the best general blend of good material properties and clinical performance for routine anterior and posterior restorations [33].
Dental amalgam has been used successfully for almost 200 years as a restorative material, without its poor esthetic characteristics and potential mercury exposure; this material still provides strong, durable and the best cost-effective direct posterior restoration [34]. The use of pins for added retention in large amalgam restorations requires the removal of additional tooth structure and weakens the remaining enamel and dentin. In an effort to minimize tooth reduction, bonded amalgam restorations were introduced in the late 1980s [35].
In 1994, Panavia was modified to include a dentin/enamel primer containing hydroxethylmethacrylate (HEMA), N-methacryloyl 5- aminosalicylic acid and MDP, intended to improve bond strength to dentin [36]. The current product, Panavia F 2.0 is bis-GMA resin cement primarily marketed for the cementation of resin-bonded fixed-partial dentures [37]. The original Panavia, initially introduced in the mid- 1980s as a powder and liquid, has since undergone several improvements and today is marketed in a two paste metered-dosed system with a self-etching primer [37].
In the present study the fracture resistance of bonded amalgam is less than that of Tetric N Flow and Fuji LC GIC, may be due to its brittleness and unable to plastically deform under stress [38]. The other reason may be due to the presence of self etching primer in which the acidic monomers of the primer dissolve and incorporate the smear layer, by this superficial penetration of thicker hybrid layer will leads to reduced capacity to absorb loads and reinforcing capacity [39].
In this study, the presence of intra orifice barriers strengthen the fracture resistance of endodontically treated teeth as compared to endodontically treated teeth without intra orifice barriers. After RCT, the teeth will fracture because of loss of vitality and moisture content, but with the help of intra orifice barriers fracture resistance of teeth can be extended without the presence of full coverage restoration like crown, endo crowns, onlay etc. intra orifice barriers provide not only the fracture resistance but also the coronal sealing, so it will definitely boost the treatment outcome of the root canal treated teeth.
Limitations
The limitations of the present study are that the results of the study cannot apply in clinical conditions. The influence of sealer on the bonding of restorations to the root canal walls was not taken in consideration. Further studies are necessary to precisely correlate the results of this study to clinical success.
Conclusion
Within the limitations of this ex-vivo study, the following conclusions can be drawn: Presence of intra-orifice barriers leads to greater fracture resistance and reinforcement of endodontically treated teeth. Tetric N Flow and Fuji GC LC GIC can be used as intra-orifice barriers with good fracture resistance in obturated roots.