Introduction: The prognosis of myocardial dysfunction in critically ill patients with sepsis and its association with mortality is controversial. We aim to determine the significance of left ventricular systolic dysfunction in septic shock patients and their associated outcome.
Materials and Methods: A prospective, single center, observational study was carried out at an intensive care unit of a tertiary care hospital. A total of 66 patients diagnosed with septic shock were enrolled in the study from September 2010 to June 2012. The 2D echocardiography was performed for all the patients. Ejection fraction <50% was the diagnosing parameter for the patients with systolic dysfunction in septic shock. Acute Physiology and Chronic Health Evaluation III (APACHE III) score was calculated.
Results: The mean age of patients were found to be 53.71 ± 16.76 years. The mortality rate was found to be 48.48% and among them 43.75% patients had ejection fraction <50%. Non-survivors exhibited significantly lower mean blood pressure (74.19 ± 10.28 versus 80.59 ± 11.31; p = 0.008), lower ejection fraction (52.59 ± 16.37 versus 62.56 ± 8.31; p = 0.029) and higher APACHE III score (89.34 ± 15.41 versus 70.65 ± 13.27; p <0.001). The receiver operating characteristic curves APACHE III score (area under curve = 0.830) and ejection fraction (area under curve = 0.656) were used to predict the mortality in septic patients.
Conclusion: Low ejection fraction, a marker to measure left ventricular systolic dysfunction is a predictor of mortality in septic shock patients. However, more research is needed to confirm the findings.
Introduction
Sepsis is a serious medical condition affecting millions of patients each year. The average documented incidence of sepsis worldwide is 56-91 cases per 1,00,000 people, with a reported mortality rate of 30% [1]. Myocardial dysfunction is a common feature of sepsis. Cardiac dysfunction in septic shock is a crucial component of multiple organ dysfunction [2] and is an important cause of fatality [3,4]. Dysfunction of left ventricle (LV) associated with sepsis has been reported decades ago [2], but was not absolutely recognised until the widespread use of echocardiography in intensive care unit (ICU) [5,6]. The mechanism is still unclear and is probably multifactorial [7].
The pathophysiology and various types of myocardial dysfunction are well documented in literature. Numerous echocardiographic parameters have been developed to assess the LV function in sepsis [8]. Among these parameters, ejection fraction (EF) is most commonly used to evaluate LV systolic function [4,9].
In spite of larger data, the presence of LV systolic dysfunction and its relation with the outcome is still conflicting especially in septic shock patients [5,10]. The correlation between low ejection fraction and mortality is not clear [2,10,11]. The aim was to evaluate the significance of LV systolic dysfunction in the patients with septic shock and its association with the mortality in these patients.
Materials and Methods
Study Design and Patient Population
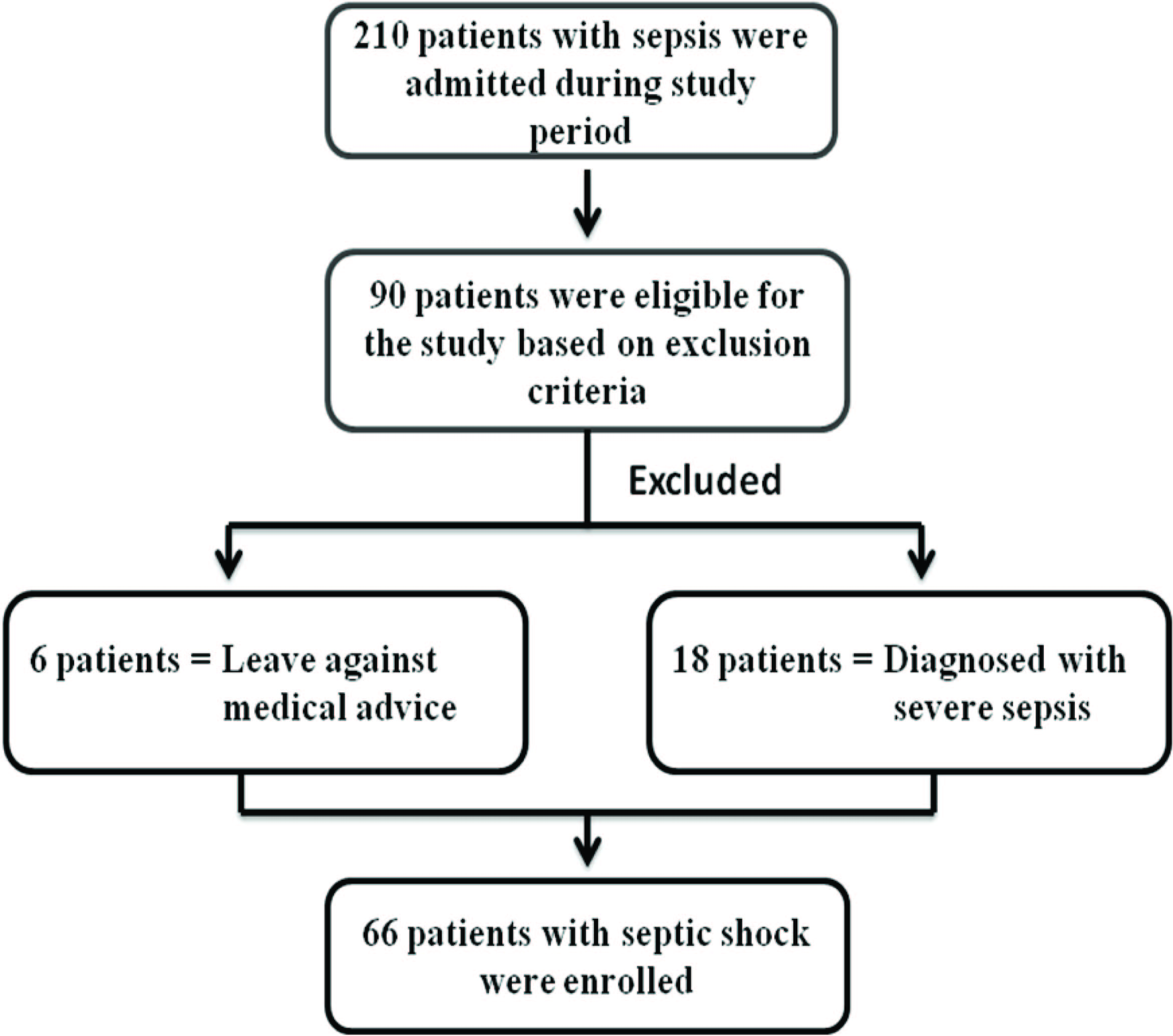
A prospective, single centre, observational study was carried out at Kasturba Medical College & Hospital, Manipal, India, from September 2010 to June 2012. A total of 66 patients with septic shock were enrolled in the study after complying with inclusion and exclusion criteria. The enrollment procedure of patients is shown in [Table/Fig-1]. Informed consent was obtained and the study was approved by the Institutional Ethics Committee. (177/2010 meeting held on 14th December 2010).
The patients have been diagnosed with septic shock as per the guidelines of ACCP/SCCM Consensus Conference Committee [12]. The inclusion criteria included organ dysfunction and acute circulatory failure characterized by (a) persistent arterial hypotension (defined as a systolic arterial blood pressure <90 mm Hg or reduction from baseline by >40 mm Hg), despite adequate volume resuscitation (septic shock) (b) presence of infection, documented or strongly suspected, with a systemic inflammatory response, together with two or more of the following:
- Temperature > 38°C or <36°C
- Heart Rate > 90 bpm
- Respiratory Rate 30/min with PaCO2 < 32
- Total leukocyte count > 12 x 109 /L or < 4x 109 /L or > 10% staff cells
Exclusion criteria included patients with age lesser than 18 years, pregnancy, patients who documented with valvular heart disease, known ischemic heart disease, dilated cardiomyopathy, hypertension, myocarditis, connective tissue diseases, abuse of drugs such as alcohol and cocaine, arrhythmias, diabetes mellitus, hypothyroidism or hyperthyroidism.
Baseline clinical variables were collected including age, gender, co-morbidities, hemodynamic parameters, requirement and dose of inotropes and Acute Physiology and Chronic Health Evaluation (APACHE) III score.
Echocardiography
All patients underwent 12 lead electrocardiogram and 2D echocardiography using Vivid e portable echo machine from GE healthcare using 2.5 MHz transducer and Doppler echocardiography including Tissue Doppler Imaging. Left lateral position was used to analyse the patients. Assessments were made using parasternal long axis, short axis, apical four chamber and two chamber images according to the American Echocardiography Association Criteria. The modified Simpson’s method was used to measure the LV ejection fraction (EF). Left ventricular (LV) systolic dysfunction was defined as LVEF with <50% [13-15]. Cardiac index for assessing systolic dysfunction was calculated by dividing the cardiac output to the body surface area of patients.
Statistical Analysis
All data were analysed using SPSS version 16.0. Categorical data are presented as number of patients (percentage). Descriptive statistical analysis is performed for continuous variables. For comparison between groups, either student’s unpaired t-test or Mann-Whitney U test are used for the continuous variables according to the Gaussian distribution. The chi-square test was used to assess differences in categorical variables. All statistical tests were carried out at 5% level of significance. Receiver operating characteristic curve (ROC) analysis was performed to predict the association of APACHE score and ejection fraction with mortality.
Results
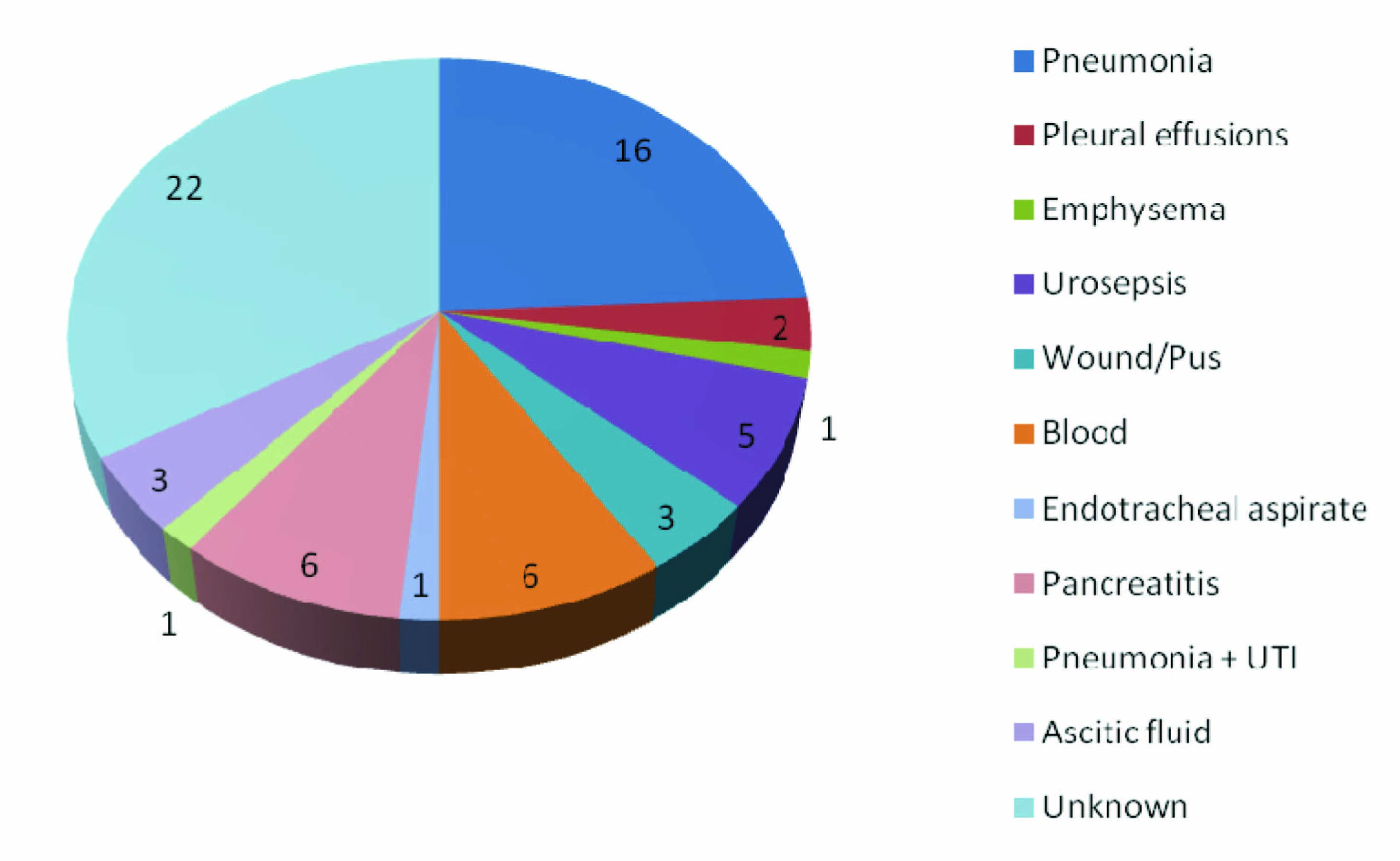
The mean age of patients was found to be 53.71 ± 16.76 years and 34 (51.5%) patients were male. Mean blood pressure (MBP) was observed as 77.48 ± 11.21 mmHg. Baseline characteristics of the patients with septic shock are shown in [Table/Fig-2]. The source of infection was not known in most of the patients (42.8%). Among the known source, the most common source of infection was pneumonia (24.2%). The other sources of infection in various patients are depicted in [Table/Fig-3]. The micro-organism associated with septic shock patients was not known in majority of patients (36.36%). Different types of microbial culture observed in septic shock patients are presented in [Table/Fig-4].
A total of 18 (27.27%) patients reported LV systolic dysfunction on the first day of admission. The mortality rate of septic shock patients was found to be 48.48%. The comparisons among the survivor and non survivor patients with sepsis are depicted in [Table/Fig-5]. Among the inotropes used for maintaining the blood pressure in patients, 44.1% of the survivors were resuscitate with noradrenaline and combination of noradrenaline and dopamine (59.4%) being the most often used in non surviving septic shock patients.
Among the indices of systolic dysfunction, MBP, APACHE III score and ejection fraction showed significant difference among the survivors and non survivors. It is clear from the table that mortality was linked to lower MBP. Fourteen patients among the non-survivors had ejection fraction <50%.
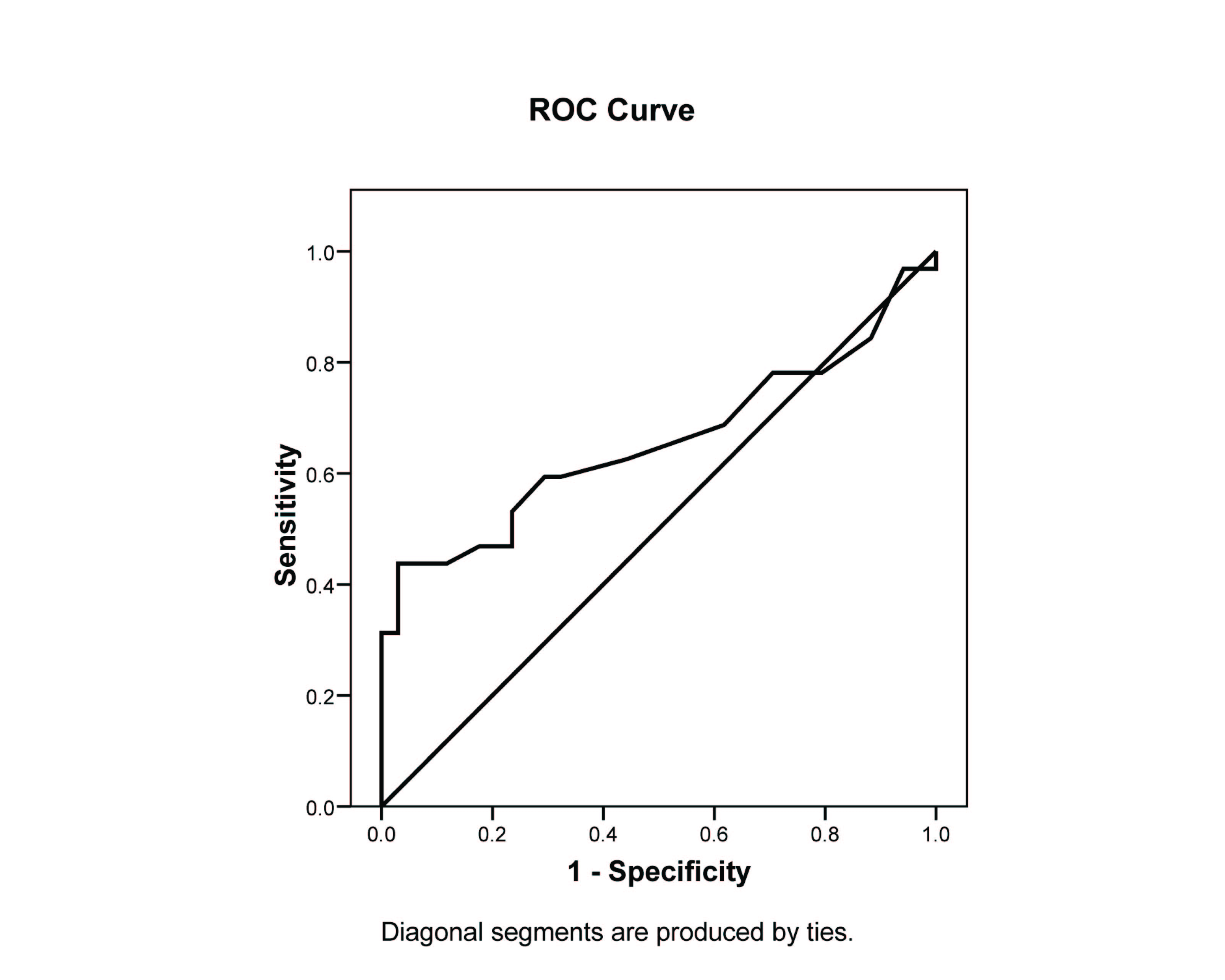
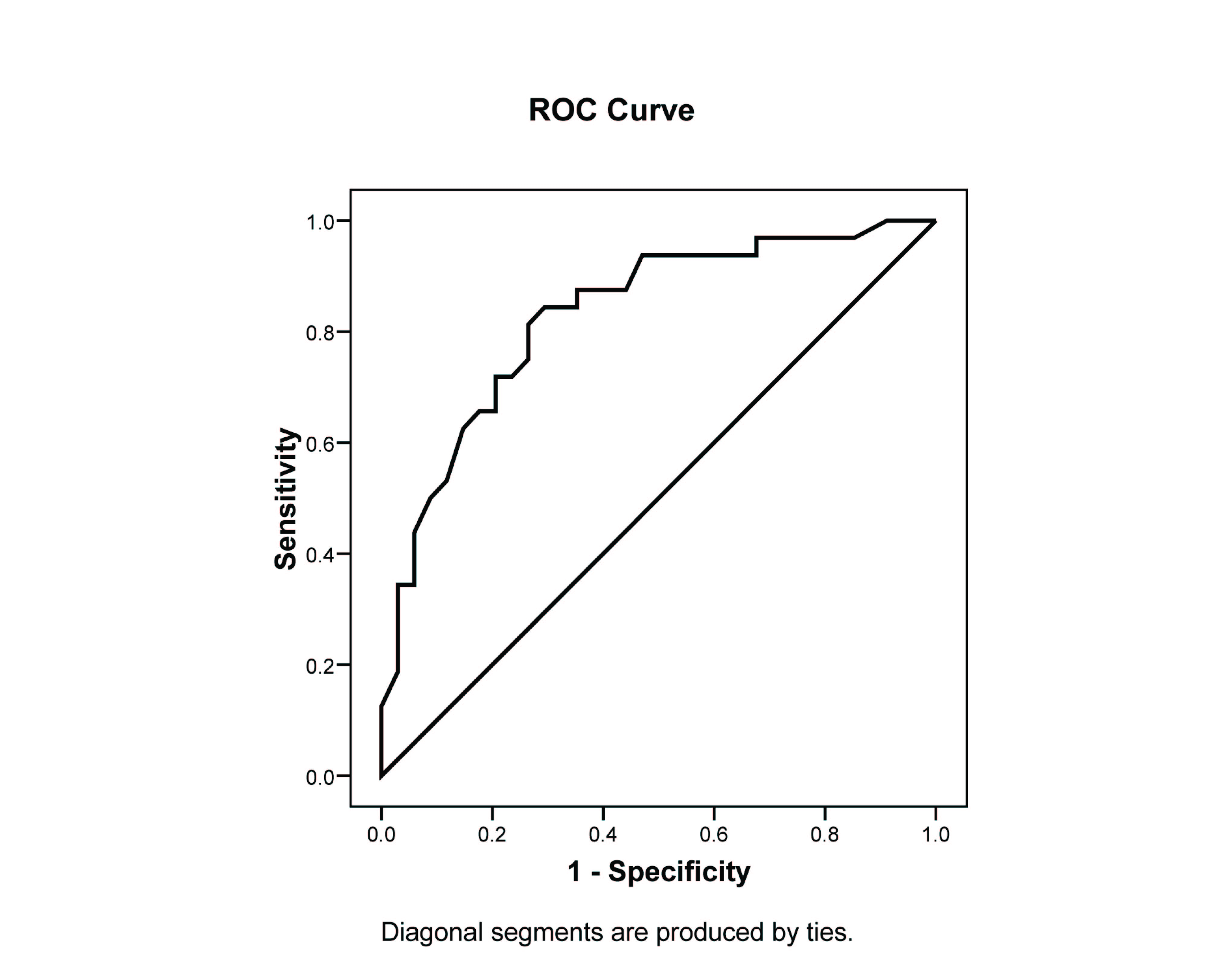
The ability of ejection fraction and APACHE III score to predict the mortality according to ROC curve is shown in [Table/Fig-6,7] respectively. The area under curve for ejection fraction was observed to be 0.656 and that of APACHE III score was found to be 0.830.
Discussion
Sepsis is the major cause of death among critically ill patients and accounts for more than 215,000 deaths per year in the United States alone [16,17]. The incidence and frequency of sepsis is continuously growing due to the factors like aging population, more number of patients with compromised immune systems, and the increased number of patients who had undergone prolonged, high risk surgery [18]. The progression of sepsis often occurs when the host cannot contain the primary infection, a problem frequently related to the characteristics of the micro-organism, the large burden of infection, persistent presence of super-antigens and other virulence factors, resistance of phagocytosis and opsonization often associated with antibiotic resistance [19]. Abnormalities in cardiac function is common in sepsis.
In this study, the mean age of patients with septic shock was found to be 53.71 ± 16.76 years which was comparatively less than the studies reported by David et al., [9]. However, the APACHE III score in septic shock patients (79.71 ± 17.07) was observed to be similar with the other reported study [9].
A prospective study conducted over 106 patients by Pulido et al., demonstrated that lower mean atrial pressure (MAP) in non-survivors is associated with mortality, although they do not show significant difference among survivors and non-survivors. The 0.830significant difference in MBP was reported in our study [7]. The risk of subsequent renal replacement therapy increases as there is increase in the time spent below the MAP of 75 mm Hg which was reported by Dunser et al., [20]. Such findings suggest the importance of addressing ischemic acute renal failure in the absence of frank hypotension [21]. This correlates that vasoactive substance plays an important role in septic patients.
In our study, LVEF was depressed in 18 (27.27%) septic shock patients. A cohort study on the ICU patients by Landsberg et al., reported 9.1% isolated systolic dysfunction [4]. Studies using echocardiography reported a 20-60% incidence of reduced EF in septic shock which was reversible in patients who survive [22-24].
In a landmark study by Parker and colleagues, 50% of the septic shock patients exhibited ventricular dilatation and hypokinesia during the first 48 h after admission [2]. Furthermore, compromised LVEF (43.9% ± 18% versus 55% ± 15%) was observed in survivors during the first 24 h [11]. In other similar studies [25], evidence of septic myocardial dysfunction in survivors was shown by depressed LVEF, although the difference in LVEF between survivors and non-survivors is not significant [4,13]. These results are contrary to our results. In the present study, survivors had better LVEF than non survivors signifying that the low EF is a measure of mortality in these patients. However, a study on 57 septic patients demonstrated by Breukmann et al., found that LVEF is a tool for determining systolic dysfunction [14].
In our study, APACHE III score showed significantly higher values in non-survivors. Amongst the ROC curves of APACHE III score and ejection fraction for predicting the mortality, APACHE III score is considered as a better predictor (AUC= 0.830) of mortality in critically ill patients than ejection fraction (AUC=0.656). Subsequently, other studies had reported the good association of APACHE III score and mortality in intensive care unit patients [26,27].
Enrollment procedure of study patients
Baseline characteristics of patients with septic shock
| Variables | Septic Shock |
|---|
| Demographic Parameters |
| Age (years) | 53.71 ± 16.76 |
| Male, n (%) | 34 (51.5%) |
| Length of hospital stay | 9.76 ± 4.21 |
| Length of ICU stay | 6.09 ± 3.45 |
| APACHE III Score | 79.71 ± 17.07 |
| Laboratory Parameters |
| Serum creatinine (mg/dL) | 1.66 ± 1.18 |
| pH | 7.13 ± 0.75 |
| Hemodynamic parameters |
| Mean blood pressure (mm Hg) | 77.48 ± 11.21 |
| Noradrenaline, n (%) | 27 (30.3%) |
| Dopamine, n (%) | 13 (19.7%) |
| Noradrenaline + Dopamine, n (%) | 20 (30.3%) |
| No medication, n (%) | 6 (9.1%) |
| Echocardiographic Parameters |
| Ejection Fraction | 57.73 ± 13.72 |
| Cardiac Index | 4.17 ± 0.90 |
Sources of infection in septic shock patients
Types of microbes involved in septic shock patients
| Types of micro-organism | Number of patients (Percentage) |
|---|
| E.coli | 7 (10.6) |
| Klebsiella | 5 (7.5) |
| Leptospirosis | 4 (6.06) |
| Pseudomonas | 9 (13.6) |
| Pseudomonas + Klebsiella | 1 (1.5) |
| Staphylococcus aureus | 3 (1) |
| Streptococcus | 1 (1.5) |
| Acinetobacter | 6 (9.09) |
| Polymicrobial | 0 (0.00) |
| Candida | 2 (3.03) |
| Enterococcus | 2 (3.03) |
| Klebsiella + E coli | 1 (1.5) |
| Rikettsial | 1 (1.5) |
| Not Known | 24 (36.36) |
Comparative analysis between survivors and non survivors in septic shock patients
| Variable | Survivors (n =34) | Non Survivors(n=32) | p-value |
|---|
| Demographic Parameters |
| Age (years) | 50.35 ± 17.11 | 57.28 ± 15.87 | 0.093 |
| Male, n (%) | 21 (61.8%) | 13 (38.2%) | 0.139 |
| APACHE III Score | 70.65 ± 13.27 | 89.34 ± 15.41 | <0.001 |
| Laboratory Parameters |
| Serum creatinine (mg/dL) | 1.70 ± 1.25 | 1.62 ± 1.11 | 1.00 |
| pH | 7.07 ± 1.04 | 7.20 ± 0.08 | 0.121 |
| Hemodynamic parameters |
| Mean blood pressure (mm Hg) | 80.59 ± 11.31 | 74.19 ± 10.28 | 0.008 |
| Noradrenaline, n (%) | 15 (44.1%) | 5 (15.6%) | 0.006 |
| Dopamine, n (%) | 6 (17.6%) | 7 (21.9%) |
| Noradrenaline + Dopamine, n (%) | 8 (23.5%) | 19 (59.4%) |
| No medication, n (%) | 5 (14.7%) | 1 (3.1%) |
| Echocardiographic Parameters |
| Ejection fraction | 62.56 ± 8.31 | 52.59 ± 16.37 | 0.029 |
| Ejection fraction <50%, n (%) | 4 (11.76%) | 14 (43.75%) | 0.005 |
| Cardiac index | 4.03 ± 0.77 | 4.32 ± 1.01 | 0.311 |
Receiver-operating characteristic curve for predicting mortality by using ejection fraction. Area under curve is 0.656
Receiver-operating characteristic curve for predicting mortality by using APACHE III score. Area under curve is 0.830
Conclusion
In a nutshell, left ventricular systolic dysfunction was observed in our study with an association of mortality in septic shock patients. Decreased ejection fraction may be considered as sole criteria for diagnosing systolic dysfunction and predicting mortality. However, further studies are still needed to provide clear and confirmatory diagnosis.
[1]. I Jawad, I Luksic, SB Rafnsson, Assessing available information on the burden of sepsis: global estimates of incidence, prevalence and mortalityJ Glob Health 2012 2(1):010404 [Google Scholar]
[2]. MM Parker, JH Shelhamer, SL Bacharach, MV Green, C Natanson, TM Frederick, Profound but reversible myocardial depression in patients with septic shockAnn Intern Med 1984 100(4):483-90. [Google Scholar]
[3]. M Maeder, T Fehr, H Rickli, P Ammann, Sepsis-Associated Myocardial DysfunctionDiagnostic and Prognostic Impact of Cardiac Troponins and Natriuretic PeptidesCHEST Journal 2006 129(5):1349-66. [Google Scholar]
[4]. G Landesberg, D Gilon, Y Meroz, M Georgieva, PD Levin, S Goodman, Diastolic dysfunction and mortality in severe sepsis and septic shockEur Heart J 2012 33(7):895-903. [Google Scholar]
[5]. J Hunter, M Doddi, Sepsis and the heartBr J Anaesth 2010 104(1):3-11. [Google Scholar]
[6]. WJ Paulus, C Tschope, JE Sanderson, C Rusconi, FA Flachskampf, FE Rademakers, How to diagnose diastolic heart failure: a consensus statement on the diagnosis of heart failure with normal left ventricular ejection fraction by the Heart Failure and Echocardiography Associations of the European Society of CardiologyEur Heart J 2007 28(20):2539-50. [Google Scholar]
[7]. JN Pulido, B Afessa, M Masaki, T Yuasa, S Gillespie, V Herasevich, Clinical spectrum, frequency, and significance of myocardial dysfunction in severe sepsis and septic shockMayo Clin Proc 2012 87(7):620-28. [Google Scholar]
[8]. N Dittoe, D Stultz, BP Schwartz, HS Hahn, Quantitative left ventricular systolic function: from chamber to myocardiumCrit Care Med 2007 35(8 Suppl):S330-39. [Google Scholar]
[9]. DJ Sturgess, TH Marwick, C Joyce, C Jenkins, M Jones, P Masci, Prediction of hospital outcome in septic shock: a prospective comparison of tissue Doppler and cardiac biomarkersCrit Care 2010 14(2):R44 [Google Scholar]
[10]. T Furian, C Aguiar, K Prado, RV Ribeiro, L Becker, N Martinelli, Ventricular dysfunction and dilation in severe sepsis and septic shock: relation to endothelial function and mortalityJ Crit Care 2012 27(3):e9-15. [Google Scholar]
[11]. A Vieillard-Baron, V Caille, C Charron, G Belliard, B Page, F Jardin, Actual incidence of global left ventricular hypokinesia in adult septic shockCrit Care Med 2008 36(6):1701-06. [Google Scholar]
[12]. RC Bone, RA Balk, FB Cerra, RP Dellinger, AM Fein, WA Knaus, Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. 1992Chest 2009 136(5 Suppl):e28 [Google Scholar]
[13]. L Weng, YT Liu, B Du, JF Zhou, XX Guo, JM Peng, The prognostic value of left ventricular systolic function measured by tissue Doppler imaging in septic shockCrit Care 2012 16(3):R71 [Google Scholar]
[14]. M Brueckmann, G Huhle, S Lang, KK Haase, T Bertsch, C Weiss, Prognostic value of plasma N-terminal pro-brain natriuretic peptide in patients with severe sepsisCirculation 2005 112(4):527-34. [Google Scholar]
[15]. JE Parrillo, Pathogenetic mechanisms of septic shock N Engl J Med 1993 328(20):1471-77. [Google Scholar]
[16]. RS Hotchkiss, IE Karl, The pathophysiology and treatment of sepsisN Engl J Med 2003 348(2):138-50. [Google Scholar]
[17]. DC Angus, WT Linde-Zwirble, J Lidicker, G Clermont, J Carcillo, MR Pinsky, Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of careCrit Care Med 2001 29(7):1303-10. [Google Scholar]
[18]. GS Martin, DM Mannino, S Eaton, M Moss, The epidemiology of sepsis in the United States from 1979 through 2000N Engl J Med 2003 348(16):1546-54. [Google Scholar]
[19]. JA Russell, Management of sepsisN Engl J Med 2006 355(16):1699-713. [Google Scholar]
[20]. MW Dunser, J Takala, H Ulmer, VD Mayr, G Luckner, S Jochberger, Arterial blood pressure during early sepsis and outcomeIntensive Care Med 2009 35(7):1225-33. [Google Scholar]
[21]. JG Abuelo, Normotensive ischemic acute renal failureN Engl J Med 2007 357(8):797-805. [Google Scholar]
[22]. F Jardin, D Brun-Ney, B Auvert, A Beauchet, JP Bourdarias, Sepsis-related cardiogenic shockCrit Care Med 1990 18(10):1055-60. [Google Scholar]
[23]. A Vieillard Baron, JM Schmitt, A Beauchet, R Augarde, S Prin, B Page, Early preload adaptation in septic shock? A transesophageal echocardiographic studyAnesthesiology 2001 94(3):400-06. [Google Scholar]
[24]. B Bouhemad, A Nicolas-Robin, C Arbelot, M Arthaud, F Feger, JJ Rouby, Acute left ventricular dilatation and shock-induced myocardial dysfunctionCrit Care Med 2009 37(2):441-47. [Google Scholar]
[25]. F Jardin, T Fourme, B Page, Y Loubieres, A Vieillard-Baron, A Beauchet, Persistent preload defect in severe sepsis despite fluid loading: A longitudinal echocardiographic study in patients with septic shockChest 1999 116(5):1354-59. [Google Scholar]
[26]. GS Shrestha, R Gurung, R Amatya, Comparison of Acute Physiology, Age, Chronic Health Evaluation III score with initial Sequential Organ Failure Assessment score to predict ICU mortalityNepal Med Coll J 2011 13(1):50-54. [Google Scholar]
[27]. WA Knaus, DP Wagner, EA Draper, JE Zimmerman, M Bergner, PG Bastos, The APACHE III prognostic system. Risk prediction of hospital mortality for critically ill hospitalized adultsChest 1991 100(6):1619-36. [Google Scholar]