Primary Hydatid Cyst of the Diaphragm Mimicking Diaphragmatic Tumour: A Case Report
Vinay Kumar Doddaballapur Prasanna Kumar1, Shama Shetty2, Rajat Saxena3
1 Assistant Professor, Department of Radiodiagnosis, Adichunchangiri Institute of Medical SciencesBellur, Mandya District, Karnataka, B.G.Nagar, India.
2 Junior Resident, Department of Radiodiagnosis, Adichunchangiri Institute of Medical SciencesBellur, Mandya District, Karnataka, B.G.Nagar, India.
3 Junior Resident, Department of Radiodiagnosis, Adichunchangiri Institute of Medical SciencesBellur, Mandya District, Karnataka, B.G.Nagar, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Vinay Kumar Doddaballapur Prasanna Kumar, Assistant Professor, Department of Radiodiagnosis, Adichunchangiri Institute of Medical Sciences Bellur, Mandya District, Karnataka, B.G.Nagar-571448, India. E-mail : vinaykumardp.8@gmail.com
Echinococcus commonly affects the liver and the lung, but several organs can be affected by this disease. The isolated primary diaphragmatic hydatid cyst, not associated with liver or lung, is very rare. We report a case of hydatid cyst in a 55-year-old male, located in the abdominal side of the left hemidiaphragm which mimicked a hypovascular diaphragmatic tumour and exophytic splenic cyst. In our case the diagnosis was confirmed only with histopathological examination done after surgical excision of the cyst. The aim of this work lies in the fact that knowledge of this clinical entity especially in endemic areas as in India will enable radiologists to guide the clinicians in proper diagnosis and adequate pre-operative planning.
Cystectomy, Echinococcus, Hydatid disease
Case Report
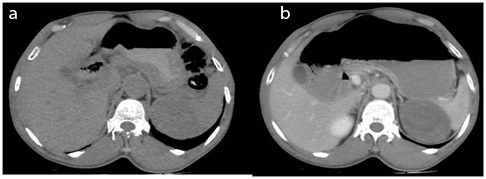
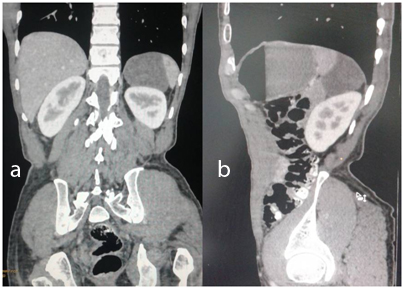
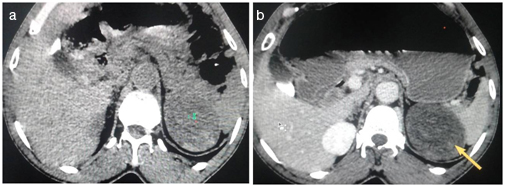
An elderly male 55-year-old presented with history of dull aching pain in left hypochondrium since 2 years. The pain was intermittent in nature and radiated to left back. He was referred to the Department of Radiology for USG which revealed heterogenous mass in left suprarenal area closely abutting superior pole of spleen. It was followed by CECT examination performed with multislice scanner (GE Brivo 385- 16 slice scanner) with reconstruction in multiple planes. CT examination revealed a well defined soft tissue density lesion in left suprarenal region in close approximation with left dome of diaphragm closely abutting the spleen laterally. The lesion demonstrated thin smooth peripheral enhancement. The relationship of the lesion was better evaluated with reconstructed images in multiple planes [Table/Fig-1a,b,2a,b]. Since the lesion was thought be arising from diaphragm, a hypovascular diaphragmatic tumour was suspected. Differentials considered were benign tumour of diaphragm – fibroma, cystic lymphangioma. Splenic exophytic cyst was considered a rare possibility. Lack of experience with this unusual location of hydatid cyst failed us to include the possibility of hydatid cyst in the list of differential diagnosis. Retrospective examination of the images revealed a unilocular cystic lesion with subtle evidence of floating membranes and hyperdense contents within the lesion representative of turbid hydatid sand which could have clinched the diagnosis [Table/Fig-3a,b].
(a) A well defined hypodense lesion adherent to posterior aspect of left hemidiaphragm, closely abutting spleen laterally and adrenal gland medially. (b) On post contrast study the lesion is noted demonstrating thin, smooth peripheral enhancement
Coronal and sagittal reformatted images (2a and 2b) better demonstrates the relationship of the lesion with spleen and left kidney and the lesion is clearly noted arising from the undersurface of the left hemidiaphragm
(a) Retrospective examination of the NECT images with slight manipulation of window widths reveal hyperdense intracystic contents (blue arrow) corresponding to floating detached membranes and hydatid sand (b) CECT examination reveals peripheral enhancement of the cystic lesion without evidence of internal enhancement
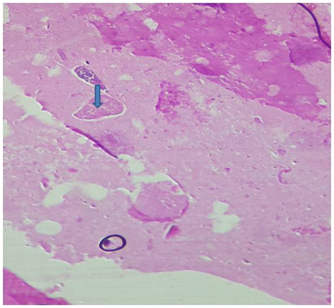
Imaging was followed by laparotomy and surgical excision. Intraoperative findings were that the lesion was adherent to posterior aspect of left hemidiaphragm and spleen. Double breasting of left hemidiaphragm was done following a roof top incision. A part of diaphragm adherent to mass was removed. During the section of the adherences between the cyst and the spleen and the diaphragm, the hydatid cyst began to separate from the spleen and remained attached to the diaphragm and clear cleavage plane was obtained from spleen [Table/Fig-4]. So, it was clear that the cyst originated from the diaphragmatic muscle. The lesion was found to be cystic with a small rent in the cyst wall. Followed by excision, the surgical site was irrigated with a combination of 40% povidone iodine and hypertonic saline. Postoperative histopathological examination confirmed the lesion to be a hydatid cyst [Table/Fig-5].
(a) Photographs taken during resection reveals a cystic mass being resected once its attachments and adhesions were cleared. (b) The resected specimen consists of a single, globular grey white to grey brown tissue mass measuring 6x6x3cm. Small rent was seen probaly due to surgical manipulation. Cut surface- grey white pultaceous material present
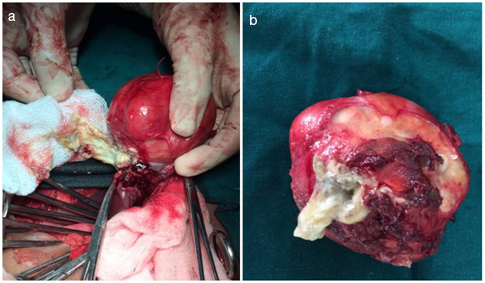
Sections studied show a pericyst made of fibrofatty collagenous tissue with congested blood vessels. Multiple ectocysts of the parasite echinococcusgranulosus in the form of laminated membranes are seen. Endocyst comprising of granular eosinophilic material with brood capsules embedded within it are noted
Discussion
Hydatid disease, caused by the Echinococcus granulosus is a serious problem in which it is endemic like the Asian and Mediterranean countries due to close association with the primary hosts of the pathological agent, the dogs and the intermediate hosts which are sheep and cattle. Humans enter the cycle by contacting infected canine faeces. Liver and lung are the most common sites of the disease, but knowledge of the unusual sites of hydatid is equally important as it can mimic various pathologies. Other unusual sites are brain, mediastinum, heart, bones and kidney [1]. Diaphragmatic localization is very rare with the incidence of around 1% [2]. Though exact number of cases is difficult to comment, only isolated case reports are found in literature. Herein we present a unique case of isolated primary diaphragmatic hydatid cyst. The case is unique not only because of the location but also because of its unusual imaging features which lacked the presence of daughter cysts. Also the lack of experience about this entity made us fail to include the diagnosis of diaphragmatic hydatid in the list of differential diagnosis in preoperative imaging. MRI could not be done due to financial constraints.
Hydatid disease most frequently involves the liver (50-93%) [3]. The route of spread in the pathogenesis of isolated/primary diaphragmatic hydatid cyst is not well known to date. Theories proposed to explain this phenomenon are due to the intraperitoneal spread from the liver or intrapleural spread from the lung localizations or due to involvement of the diaphragm frpm blood flow transportation of the embryo [4]. Even in the study by Vega et al., they concluded that isolated diaphragmatic localisation is possible when the embryos reach that site by arterial or lymphatic circulation [5].
In our patient this disease was purely diaphragmatic, without evidence of liver, lung or splenic involvement. The diagnosis of the diaphragmatic location is frequently incidental especially when the cyst is small and isolated. Large cysts on the other hand cause the symptoms related to the compression.
Preoperative diagnosis can be difficult in few cases especially in regions where the disease process is not endemic. A combination of clinical, laboratory and radiological findings helps in arriving at a preliminary diagnosis though organ of origin is not always possible with USG or CT. MRI is superior to CT in localisation as well as characterization of the cystic echinococcosis [6]. As in our case, the lesion was considered to be a primary diaphragmatic tumour prior to resection due to the various factors like lack of typical CT features, lack of awareness of this particular diagnostic entity and absence of subsequent MR Imaging. Retrospective evaluation of the CT images enabled us to identify subtle intracystic hyperdense membranes corresponding to floating membranes and hydatid sand which are consistent with the diagnosis of hydatid cyst.
Differential diagnoses include adrenal tumour, cystic lymphangioma and splenic exophytic hydatid cyst. Intraoperative findings and HPE confirmed the diagnosis as hydatid cyst.
Usually an isolated diaphragmatic hydatid cyst will be asymptomatic or result in a dull aching pain. However treatment is necessary to prevent secondary complications like rupture or infection. Complete resection can be achieved in case of small cystic lesions without any injury to diaphragm [7,8]. However, in large cysts, diaphragmatic reconstruction may be required with the use of prosthetic materials to prevent diaphragmatic hernia [8,9]. In our case, it was possible to perform a total cystectomy with minimal repair of the diaphragm.
Conclusion
Awareness of HD in the diaphragm is necessary to avoid erroneous preoperative diagnosis and the possibility of hydatid disease should be considered in patients with preoperative cross sectional imaging indicating cystic lesions adjacent to the diaphragm, especially in endemic areas like India and if any of the specific imaging features such as calcification, daughter cysts and/or intracystic membranes are seen.
[1]. Polat P, Kantarci M, Alper F, Suma S, Koruyucu MB, Okur A, Hydatid Disease from head to toeRadiographics 2003 23(2):475-94. [Google Scholar]
[2]. Eren Ulku R, Tanrıkulu AÇ, Eren MN, Primary giant hydatid cyst of the diaphragmAnn Thorac Cardiovasc Surg 2004 10:118-19. [Google Scholar]
[3]. Amr SS, Amr ZS, Jitawi S, Annab H, Hydatidosis in Jordan: an epidemiological study of 306 casesAnn Trop Med Parasitol 1994 88:623-27. [Google Scholar]
[4]. Daali M, Hssaida R, Hajji A, Hydatid cyst of the gluteal muscle. Apropos of a casePresse Med 2000 29:654 [Google Scholar]
[5]. De Vega DS, Vazquez E, Tamames S, Hydatid cyst of the diaphragm. Apropos of a caseJ Chir (Paris) 1991 128:76-78.(in French) [Google Scholar]
[6]. Stojkovic M, Rosenberger K, Kauczor HU, Junghanss T, Hosch W, Diagnosing and staging of cystic echinococcosis: how do CT and MRI perform in comparison to ultrasound?PLoS neglected tropical diseases 2012 6(10):e1880 [Google Scholar]
[7]. Gurbanaliev IG, Gadzhiev SI, Dzhavadov E, Echinococcosis of the diaphragmKhirurgiia (Mosk) 1989 3:73-6. [Google Scholar]
[8]. Kjossev K, Losanoff J, Velitchkov N, Belokonski E, Hydatid cyst of the diaphragm: a case report and review of the literatureInternet J Thorac Cardiovasc Surg 2003 6:1 [Google Scholar]
[9]. Khudarbergenov AM, Diaphragmatic echinococcosisKlin Khir 1988 (3):39-40. [Google Scholar]