Road traffic accidents are on the rise and many of these patients suffer from head injuries and lung contusions besides sustaining fractures at the other sites of the body. Besides, pulmonary contusion is a common occurrence in patients sustaining any severity of blunt chest trauma [1]. It can also be caused due to explosion injuries or a shock wave associated with a penetrating trauma. Following the injury to the lung parenchyma, accumulation of blood and fluid develops in the alveolar spaces causing oedema and disruption of normal lung structure and function [2]. This occurs during the first 24 hours after the injury and resolves within approximately seven days [1]. Patients may present initially with minimal respiratory insufficiency while 50% - 60% of these patients may develop acute respiratory distress syndrome (ARDS) requiring mechanical ventilation and this increases the mortality in these cases [3].
Pulmonary contusions may present along with rib fractures and other signs of chest wall trauma like bruising, flail chest, haematomas, etc. Associated pleural effusion, haemothorax and pneumothorax may also be seen [4]. Hypoxemia and respiratory distress occurs due to ventilation-perfusion mismatch, increased intra-pulmonary shunting, segmental lung damage and loss of lung compliance [2].
Management goals traditionally followed are judicious fluid management, supportive oxygen therapy and supportive therapy. Intensive care may be required for close monitoring and provision of mechanical ventilation at the earliest. Mortality in these cases can be prevented by early diagnosis and close monitoring of the treatment in these patients with lung contusion.
Therefore, the present study was done to assess the outcome in all the cases of blunt chest trauma with pulmonary contusions in our intensive care unit and to evaluate the various factors determining the mortality in these patients.
Materials and Methods
A retrospective case study was conducted at KLES Dr. Prabhakar Kore Hospital and MRC, Belgaum between January 2013 to December 2013 of all blunt chest trauma cases with pulmonary contusions was done. Chest X–rays and CT scan of thorax had been used to diagnose pulmonary contusions in all the patients. Hospital records were reviewed for collection of demographic data, duration of hospital admission, hospital course and final outcomes. These patients were evaluated for various variables such as age, associated injuries, APACHE II score, SAPS II score, SOFA score, paO2/Fio2 ratio, fracture of ribs, presence of haemothorax or pneumothorax, requirement of ventilatory support, number of ventilator days, ICU days, use of colloids, PEEP usage, mean positive fluid balance per day, and finally, hospital outcome. Data analysed were divided into two groups – survivors and non survivors. Post mortem examination was done on all patients who died as most of these cases were admitted as Medico-legal cases. A total of five patients with lung contusion died, and post-mortem showed that these patients had severe pulmonary haemorrhage along with haemorrhage in the brain. The study was approved by the Institutional Ethics committee.
Statistical Analysis
Statistical analysis was done using student unpaired t-test and Fisher Exact test. A p-value < 0.05 was considered significant.
Results
A total of 16 cases of pulmonary contusions were included in the study. Baseline characteristics of all the patients within the first 24 hours are shown in [Table/Fig-1]. A total of 5 patients died during the ICU stay and 11 survived. Two patients with coexisting head injuries, and two patients having lower limb crush injuries and liver laceration respectively died of sepsis and one patient had lung laceration with continuous bleeding.
Baseline characteristics of the patients
| Variables | Survivorsn=11 (68.7%) | Non survivorsn=5 (31.3%) | p-value |
|---|
| Age | 35 | 40.4 | |
| APACHE II score | 10.2±8.32 | 29.4±4.56 | <0.001 |
| SAPS II score | 19.6±13.28 | 55.8±7.91 | <0.001 |
| SOFA score | 5.1±4.08 | 13.8±4.08 | <0.001 |
| Coexisting head injury | 1 (9.09) | 2 (40) | 0.243 |
| Fracture of ribs | 8 (72.72) | 3 (60) | 1 |
| Presence of haemo/pneumothorax | 5 (45.45) | 4 (80) | 0.308 |
All patients had associated injuries like head injuries, crush injuries, liver laceration, various bones fractures etc. Three patients in non-survivor group had rib fractures and 4 had associated haemopneumothorax [Table/Fig-2,3]. Most of the patients belonged to the age group of 20-60 years. All the patients were males. The mean age of non survivor was higher than survivors (40.4 v/s 35 years respectively). There was significant difference observed among the survivors and non-survivors in APACHE II score (10.2 ± 8.32 vs 29.4 ± 4.56; p<0.001), SAPS II score (19.6 ± 13.28 vs 55.8 ± 7.91; p<0.001), SOFA score (5.1 ± 4.08 vs 13.8 ± 4.08; p<0.001), mean paO2/Fio2 ratio(196.4 ± 80.89 vs 96.2 ± 42.56; p < 0.022) and mean ventilator days (1 ± 1.48 vs 4.8 ± 2.38; p<0.001) respectively.
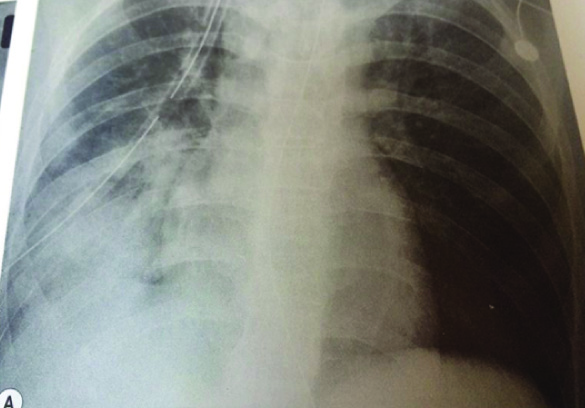
Chest x-ray showing right sided lung contusion with intercoastal tube in situ for haemothorax
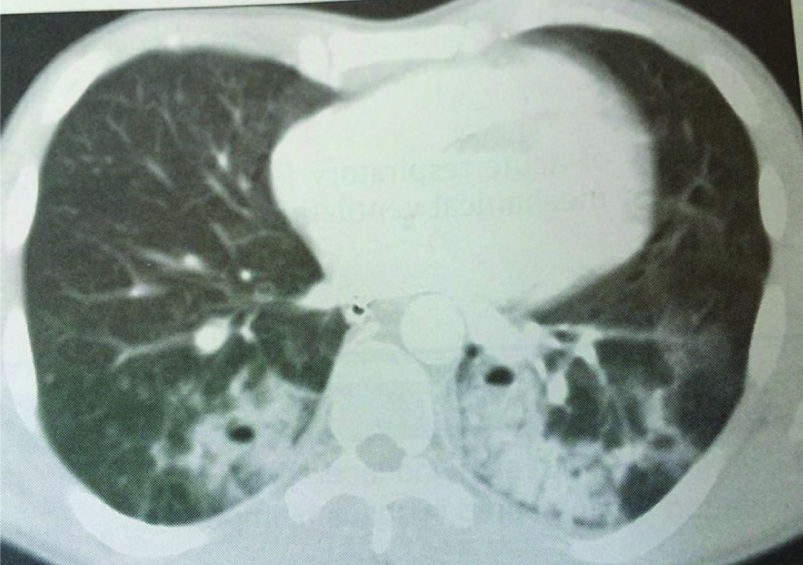
CT scan thorax showing bilateral lung contusions of lower lobes
However, no significant difference was seen in number of ICU days, presence of fracture of ribs and presence of either haemothorax or pneumothorax between the two groups. The detail analysis is presented in [Table/Fig-4].
Mean variables between the survivors and non survivors
| Variables | Survivorsn=11 (68.7%) | Non survivorsn=5 (31.3%) | p-value |
|---|
| Mean paO2/Fio2 ratio | 196.4±80.89 | 96.2±42.56 | <0.022 |
| Mean ventilator days | 1±1.48 | 4.8±2.38 | <0.001 |
| Mean ICU days | 5.5±2.91 | 4.8±2.38 | 0.626 |
| Use of vasopressors | 2 (18.18) | 4 (80) | 0.177 |
There was increased incidence of bleeding through the endotracheal tube, positive fluid balance (1155.4 ± 435.6 ml) in non-survivors versus (448.9 ± 643 ml) in survivors group (p=0.007), but no difference was noted in with either crystalloid or colloid use.
Discussion
Pulmonary contusions occur in 30%-75% of the cases with blunt thoracic trauma following vehicular accidents [5]. Isolated cases can occur due to explosion injury, but most common associated injuries like rib fractures and haemo-pneumothorax are also seen [6]. Respiratory distress is common after lung trauma, with hypoxemia and hypercapnea being greatest at 72 hours [1]. Hypoxemia occurs due to ventilation-perfusion mismatch in spite of proper ventilatory management.
Our study showed mean age of survivors to be lesser than non-survivors which was significant. There was also significant difference in the mean daily positive fluid balance and ventilator days. Whether the positive fluid balance worsened the lung injury and caused refractory hypoxemia in all these patients and caused mortality is unclear. Therefore, standard resuscitation with crystalloids and blood products should be started immediately to obtain euvolemia, which is probably the ideal [7].
Endotracheal bleeding was seen in non-survivors which could have been contributed to mortality in these patients. ICU scoring systems like APACHE II, SAPS II and SOFA scores used for initial assessment of the patient within first 24 hours was higher in non- survivors as compared to the survivors. The risk factors that were associated with higher mortality in patients with pulmonary contusions in the present study were APACHE II score, SAPS II score, SOFA score, paO2/Fio2 ratio, ventilator days and higher positive fluid balance. Wu et al., observed that the risk factors that affected prognosis in patients with acute lung injury due to thoracic trauma were the APACHE score, duration of trauma, age, gastrointestinal haemorrhage, pulmonary contusion, disseminated intravascular coagulation (DIC), multiple blood transfusions in 6 hour, Injury Severity Score (ISS), and aspiration of gastric contents [8]. A study by Stelin showed that age, severity of injury, associated head trauma and shock were the most important factors affecting survival in patients with pulmonary contusion [9].
Chest X-ray is the first investigation for evaluation but CT thorax remains a better choice. Focal or diffuse homogeneous opacification on chest radiograph is the mainstay of diagnosis for lung contusion. The opacification seen with pulmonary contusions is irregular and does not conform to segments or lobes within the lung. Pulmonary contusion is not always immediately apparent radiographically; one-third of patients fail to demonstrate a lesion on the initial chest radiograph [7] and hence often it requires follow-up chest radiograph for confirmation of the diagnosis. In the present study most of the patients had undergone a CT thorax for detail evaluation of thoracic injuries including haemothorax. Cohn et al., [1] has observed that the CT scan of thorax is highly sensitive in identifying the lung contusions and may help in predicting ventilator requirement.
Tyburski et al., [5] made an attempt to quantify the volume of the pulmonary contusion and correlate this volume with outcome, and they compared the pulmonary contusion score (PCS) with the initial radiograph to a repeat film 24 hours later. The mean increase in the PCS of 7.9 units was nearly equivalent to an entire hemi-lung volume. Miller et al., [10] found that in a series of pulmonary contusion detected by CT thorax scan, a mean of 18% of the pulmonary parenchyma was contused, and that the contusion increased by 11% with a repeat CT scan at 24 hours. Moreover, 82% of patients with a contusion of at least 20% developed acute respiratory distress syndrome (ARDS) versus only 22% of patients with a contusion less than 20%. There was also an increasing trend in the development of pneumonia in cases of greater contusion. Bedside chest ultrasonography can also used to detect injuries in the intensive care unit when in certain situations patient cannot undergo a CT scan. Wustner et al., showed that rib fractures and pleural effusions are commonly diagnosed by ultrasonography in patients with blunt thoracic trauma as compared to chest X-rays (65% versus 36%) and (37% versus 11%) respectively [11].
Effective treatment includes supportive treatment with oxygen support, maintenance of effective fluid balance, monitoring respiratory functions, aggressive pulmonary toilet with coughing, deep breathing and suctioning as needed and postural changes and drainage of haemopneumothorax, if present [6]. Goals of treatment in these patients include prevention of respiratory failure and hypoxia. Lung protective ventilation as per ARDS Net protocols, that is low tidal volume along with high PEEP has been advised, but this can aggravate respiratory acidosis. All the non survivors were hypoxic. All the patients had been ventilated with volume control ventilation to improve oxygenation. For refractory hypoxemia, high PEEP, inverse ratio ventilation and prone positioning can be used, whenever feasible. When the above measures fail, then individual lung ventilation with a double lumen tube should be considered, and also high frequency jet ventilation has shown good improvement in selective patients with bilateral lung contusions [12]. But it has not been shown to improve survival in blunt chest trauma. This was not used for our patients due to non availability.
Use of non-invasive positive pressure ventilation (NIPPV) for chest trauma induced hypoxemia can be considered if there are no obvious contraindications, but this lacks evidence. However, tracheal intubation and mechanical ventilation should never be delayed if the respiratory status worsens under NIPPV. Vidhani et al., have reported good outcome in patients with pulmonary contusions with non-invasive ventilation and questioned the validity of Advanced Trauma Life Support (ATLS) guidelines which strictly advises invasive ventilation for all trauma patients with hypoxia [13]. This requires more trials to be conducted for proving its validity.
Most of the pulmonary contusions heal within 14 days without complications. Patients with severe injuries and having larger lung contusions have fairly consistent symptoms. The most common complaints in these patients include dyspnea, decreased exercise tolerance, and chest pain on the side of the injury. Landercasper et al., studied 62 patients who had flail chest following injury, and 42 of these cases were having concomitant pulmonary contusion [14]. A total of 32 patients were available for mean follow-up for 5 years. It was observed that nearly about 25% had chest tightness, 49% had chest pain, and 63% complained of dyspnea. On examination it was observed that, about 46% had reduced chest expansion of less than 5 cms, and 57% had abnormal spirometry.
Limitations
The limitations of the study were that it was a retrospective type and details about certain interventions done like prone positioning, inverse ratio ventilation were not clearly available. However, close monitoring, to improve the gas exchange and better fluid management will help in improving the survival in these patients. Early measures to prevent worsening of hypoxemia should be undertaken. Finally, ideal and feasible scoring systems should be developed to assess the patients well during the initial 24 hours for better management and this will improve the outcome in these patients.
Conclusion
Pulmonary contusions are common in blunt as well as penetrating chest injuries. The risk factors that were associated with higher mortality in patients with pulmonary contusions in the present study were APACHE II score, SAPS II score, SOFA score, paO2/Fio2 ratio and ventilator days. Close monitoring to improve the gas exchange and better fluid management will help in improving the survival in these patients.