In India, like many other developing countries, there is not always an imposition to bring a valid prescription for buying the prescription only drugs. Except narcotics and few tranquilizers, most of the medicines including antibiotics can be bought even without a prescription [1].
There have been previous researches in India showing various patterns of inappropriate dispensing and use of antibiotics [2–4]. The rate of self medication is also found to be rising worldwide including India [5]. The prescribing patterns of antibiotics are not well controlled in many countries especially the developing ones [6]. All these factors emphasize the need to investigate and tackle such unhealthy practices.
Through this study, we aim to analyse the knowledge, attitude and practice of antibiotics use by the parents for their children and correlate it with the demographic characteristics. This may help in identifying the subgroups of population with high rates of antibiotic abuse and help in developing proper interventional programs to improve the public knowledge of antibiotics and hence, take a step towards controlling antibiotics resistance.
Materials and Methods
It was a cross-sectional study conducted at Dr. Yewale’s Multi-speciality Hospital for Children in Vashi, Navi Mumbai, India. It is a tertiary care hospital with both outpatient and inpatient facilities. A total of 1000 parents who visited the OPD in the months of September to November 2014 were included in the study. Informed consent was taken from all the participants after explaining them the nature and aim of the study. Those unwilling to participate were not given the questionnaire. All the information was collected in anonymous form and confidentiality was maintained.
A short questionnaire of 13 questions was designed by the authors after reviewing other questionnaires in earlier studies [1,7]. Participants were given the option of having the questions read to them and their answers recorded by the researcher or they could read and answer the survey on their own. Both the options were provided to overcome any discomfort in respondents who may have literacy difficulties and also to increase the participation rate. The questionnaire was made available in both English and the local language, Marathi in an attempt to increase the participation rate. If both parents were present, only one of them was supposed to answer the questionnaire.
To test the reliability and face validity, a pilot study was conducted on 28 subjects with similar characteristics like the study population and who were not included in the final analysis. Based on the results, minor changes were made in the framing of questions.
The demographic details collected included age, sex & education level as mentioned in [Table/fig-1]. Questions were mainly used to assess three major categories:
| Parameters | Knowledge of Antibiotics |
|---|
| Yes | No |
|---|
| No. of Cases | 872 | 128 |
| Age of child (y) Mean SD Range | 3.922.7200.2 – 15.00 y | 2.362.3000.8 – 15.00 y |
| Sex (%) Male Female | (N = 871)382 (43.9)489 (56.1) | 44 (34.4)84 (65.6) |
| Education (%)upto High School Graduate Post graduate | 175 (20.1)496 (56.9)201 (23.0) | 124 (96.9)04 (03.1)- (-) |
Knowledge related to purpose of antibiotics (Bacteria, virus, parasites or any microbe), use of antibiotics (fever, cough, skin infection, etc), side effects of antibiotics and antibiotic resistance.
Attitude towards consumption of antibiotics like the need to use antibiotics in every sick child, frequency of antibiotics use in a year.
Practice of antibiotics like use of left over antibiotics, completing the course of antibiotics.
Data was entered in MS Excel. Responses were coded and analysed using SPSS version 10.0. Descriptive and categorical statistics were used for the study. Categorical variables were compared using Chi-square test. The level of statistical significance was set at p<0.05.
Out of 13 questions, seven questions were used for scoring KAP [Table/fig-2]. Each correct answer was given one point each and wrong answer zero, making a maximum score of seven and minimal score of zero. No answer was also scored as zero. KAP score was then divided into three categories as 0-2, 3-4 and 5 or more indicating poor, moderate and good knowledge respectively. Association of respondents’ KAP score with gender, education level and previous use of antibiotics was analysed using Chi-Square test. 95% confidence interval and p-values were also mentioned. p-values less than or equal to 0.05 were considered significant.
Responses to the various statements
| Statement | Number | Percentage (%) | 95% CI |
|---|
| Antibiotics are used againstwhich organismBacteria*VirusParasitesAny microbes | 244228000400 | 28.026.100.045.9 | 25.00 – 30.9623.23 – 29.06-42.56 – 49.18 |
| Did your child receiveantibiotics in the pastone yearYes*No | 818054 | 93.806.2 | 92.21- 95.4104.59- 07.79 |
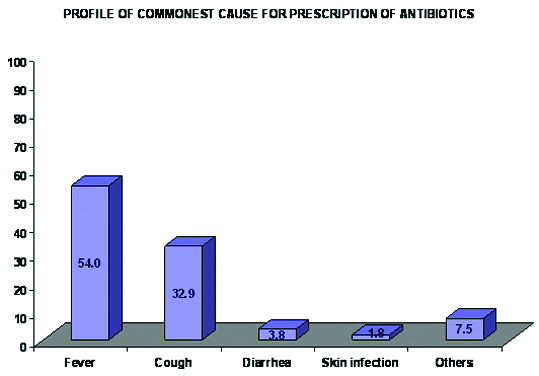
| What was the commonestcause of prescription ofantibioticsFeverCoughDiarrhoeaSkin InfectionOthers | 471287033016065 | 54.032.903.801.807.5 | 50.71 – 57.3229.79 – 36.0302.52 – 05.0500.94 – 02.7305.71 – 09.20 |
| Do you think antibiotics arerequired every time the childfalls sickYesNo* | 737135 | 84.515.5 | 82.12- 86.9213.08- 17.88 |
| Do you complete the courseof antibiotics as prescribed bythe doctorYes*No | 724148 | 83.017.0 | 80.54 – 85.5214.48 – 19.46 |
| Do you think use of antibioticscan harm the childYes*No | 642230 | 73.626.4 | 70.70 – 76.5523.45 – 29.30 |
| Have you ever used left overantibiotics from previousprescription for the childYesNo* | 129743 | 14.885.2 | 12.44- 17.1582.85 – 87.56 |
| Do you know the termantibiotic resistanceYes*No | 135737 | 15.584.5 | 13.08 – 17.8882.12 – 86.92 |
* indicates correct response which was scored as 1 point each
Only data from the parents who knew the term antibiotic was considered for the analysis. Those who had never heard antibiotics were not required to answer the questionnaire further. These cases were coded as missing values and not considered in further analysis to avoid bias [8].
Results
Out of the 1000 parents who were asked to fill the questionnaire, only 872 knew the term antibiotic and hence the remaining 128 were excluded from the analysis, thereby making the participation rate as 87.2%. The demographic details of the participants have been mentioned in the [Table/Fig-1]. Out of the 872 parents included in the study, more than 50% were females (56.1%). Education level was categorized as high school and below, graduate and then, postgraduate. A total of 496 respondents (56.9%) were graduates, while post graduates (23%) and up to High school (20.1%) constituted almost equal numbers.
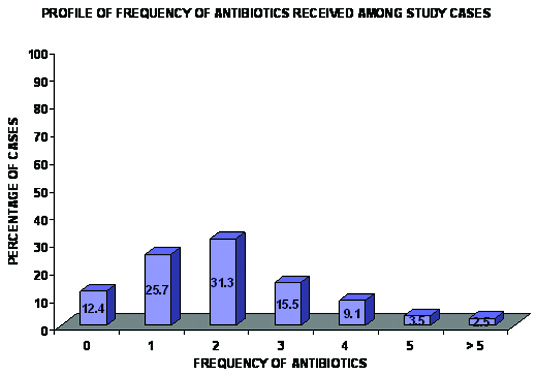
Out of the total, 93.8% parents (CI 92.21-95.41) agreed that their child received a course of antibiotics in the past. One in every four respondents (25.7%, CI 22.75 – 28.58) said that their child received a single course of antibiotics in the past one year, while 16.1% parents said that their child has received four or more course of antibiotics in the last year itself. The individual frequencies have been mentioned in [Table/Fig-3].
Showing frequency of antibiotic courses given to the child in past one year
Concerning the reason of use of antibiotics, majority (54%, CI 50.71 – 57.32) of the parents gave it to the child for fever, followed next by cough and cold (32.9%, CI 29.79 – 36.03). All the reasons of antibiotics use with their frequencies has been mentioned in the [Table/Fig-4].
Showing the commonest reason for use of antibiotics in the child in the past
Participants were confused regarding the indication of antibiotics use. This is indicated from the fact that only 244 parents (28%, CI 25.00-30.96) were aware that antibiotics are used against bacterial infection, while 228 parents (26.1%) incorrectly thought that they are used against viruses and 400 parents (45.9%) felt that antibiotics could be used for any microorganism. Only 135 respondents (15.5%, CI 13.08-17.88) knew about antibiotic resistance. More than a quarter (26.4%, CI 23.45 – 29.30) respondents felt that antibiotics don’t have any harm on excessive use. [Table/Fig-5] mentions the individual frequencies to each statement.
Showing association of KAP Score with gender, education status and previous use of antibiotics
| KAP Score | Total | Group A0-2 | Group B3-4 | Group C5-7 | p-value |
|---|
| | No. | % | 95% CI | No. | % | CI | No. | % | CI | p |
|---|
| GenderMaleFemale | 382490 | 006021 | 1.64.3 | 00.32-02.8202.5-06.09 | 048081 | 12.516.6 | 09.24-15.8913.27-19.86 | 328387 | 85.979.1 | 82.37-89.3675.54-82.74 | <0.05 |
| EducationHSC or less | 175 | 007 | 04.0 | 01.10-06.90 | 050 | 28.6 | 21.88-35.26 | 118 | 67.4 | 60.49-74.37 | <0.05 |
| Graduate | 496 | 017 | 03.4 | 01.83- 05.03 | 062 | 12.5 | 09.59- 15.41 | 417 | 84.1 | 80.85- 87.29 |
| Postgraduate | 201 | 003 | 01.5 | 00.18- 03.17 | 017 | 08.5 | 04.61- 12.30 | 181 | 90.0 | 85.91- 94.19 |
| Previous Antibiotic UseYes | 818 | 010 | 01.2 | 00.47- 01.98 | 102 | 12.5 | 10.21- 14.73 | 706 | 86.3 | 83.95- 88.66 | <0.05 |
| No | 54 | 017 | 31.5 | 19.09- 43.87 | 027 | 50.0 | 36.66- 63.34 | 010 | 18.5 | 08.16-28.88 |
It is noteworthy that 83% of the parents agreed that they completed the course of antibiotics as prescribed by the doctor, While 85.2% parents said that they never used leftover antibiotics from the previous prescription for their child.
KAP scores were found to be higher for males with more than 80% (85.9%, CI 82.37-89.36) having scores 5 or more. Respondents with higher grade of formal education were similarly found to have a higher KAP score with 90% postgraduates and 84.1% graduates having a score more than 5 while only 67% of those educated up to high school had a similar score. There was a wide variation seen in the awareness of parents who had given antibiotics to their child in the past and those who didn’t use antibiotics. An 86.3% of the former category scored more than 5 while only about 18% of the latter had such a score. There was significant association between KAP and education, gender and previous use of antibiotics each with a p-value of <0.05.
Discussion
Society plays an important role in use and abuse of antibiotics as well as the spread of uncritical tendencies [9]. Due to higher number of infectious diseases in developing countries like India, the use of antibiotics is widespread. But because of the relaxed laws in India and other developing countries, it is not difficult to obtain antibiotics without prescription (over the counter drugs) and hence, antibiotics abuse by public is common. There are some studies that have also compared differences in rural and urban population for antibiotic prescribing patterns [10,11]. While Yao et al., [10] conducted a study in China to find rural urban disparities and reported that prescribing patterns were higher in urban areas, Godycki Cwirko et al., [11] conducted a similar study in Poland and reported that there wasn’t much difference in antibiotics knowledge among people despite the difference in education levels. Though in this study we didn’t use geographical location as a comparison factor since it was undertaken at a single centre, but education has been used as a variable for comparison. Being aware of the knowledge, attitude, and practices concerning antibiotics among parents may aid in more effective communication between the healthcare practitioners and patients, as well as promote the development of policies and schemes to educate the public [12].
It was clear that people were confused about the use of antibiotics for either bacteria or virus since only 28% knew that they were used for bacterial infection. Majority of parents (45.9%) thought that antibiotics could be used for any microbial infection. This may be attributed to the reason that while counseling, doctors use the general term ‘germs’ for indication of antibiotics, rather than specifically mentioning bacteria [13]. Also, as mentioned by Rousounidis et al., [14] people don’t understand the difference between bacteria and virus and hence, believe that antibiotics are effective against both.
The lack of knowledge regarding antibiotic resistance was obvious since only 15.5% parents were aware of the term antibiotic resistance. Interestingly, though majority did not know about antibiotic resistance, many parents did appreciate that antibiotics if used in every situation or in large amounts could be harmful. This can be comprehended from the fact that 84.5% parents felt that antibiotics are not required everytime the child falls sick and 73.6% parents recognized that unnecessary and excessive use of the antibiotics could harm their child. These findings were consistent with similar studies done in other countries like Greece where parents considered excessive antibiotics use could lead to antibiotics resistance [3]. These percentages appear higher than other studies done earlier in India and therefore, may not be generalized as they indicate the values of one particular urban population setting.
A heartening observation was that 83% parents stated that they were always compliant with the antibiotics course as prescribed by their paediatrician. The results were comparable to a study done in Malaysia where 71.1% parents stated that they complete the course of antibiotics as prescribed by their doctors [15].
A 14.8% parents were found to have used antibiotics from previous prescription for their child without consulting a doctor. This may be attributed to the easy availability of antibiotics as over the counter drugs, in many countries including India. Left over antibiotics at home from previous prescription could also be due to stopping of treatment earlier than prescribed. The rate of self medication was found to be higher among the medical students as per a study conducted in India [16].
Parents who had previously used antibiotics for their child were better aware about antibiotics and followed healthier practices of antibiotics use. One likely explanation can be that those who had given antibiotics to their children in past might had been advised about the adverse effects from their doctor or pharmacist or learnt from their personal experience with antibiotic use [4]. Even other information regarding antibiotics use, compliance and indications may have been explained to them by their paediatricians.
Gender was found to be significantly associated with the KAP. This was in contrast to a study conducted in Jordan where no significant association was noted between gender and KAP [17].
Significant association was also noted between the education level and knowledge and behaviour of antibiotics use. People with lower level of education were found to lack knowledge regarding antibiotics and misuse antibiotics more. This points to the need of focusing the information campaigns and other interventions to reduce misconceptions about antibiotics to the people with lower level of education. This is comparable to a study in Indonesia where also women and people with low level of formal education were found to have more misconceptions about antibiotics [8].
Limitations
There are a few limitations of this study. Firstly, it was conducted at one hospital only and so the results may not be indicative of the entire population. Secondly, as with other questionnaire studies, it relies on the honesty and recall ability of the respondents. It should be noted that since this study took place in an urban setting where people are usually more literate, with better access to mass media and possibly would have received more information regarding antibiotics than rural settings. Also, it is limited to antibiotics use only in children and further studies may be conducted to evaluate the use of antibiotics in other groups of population.
Recommendations
There is a need to improve parents’ knowledge about antibiotics and promote healthier attitudes and practices. This requires a multi sectorial effort. Firstly, interaction between parents and health professionals can help to improve the parents’ views regarding the use and indications of antibiotics and the importance of completing their course. Mass media can also play an important role in disseminating the appropriate information to the general public. Secondly, stringent laws should be enforced by the government that prohibit the availability of antibiotics as over the counter drugs. Also, pharmacist should be encouraged to give only the amount of antibiotics as mentioned in the prescription and not as per pack sizes. Thirdly, since this study aimed at evaluating the parent’s knowledge and behaviour of antibiotic use, further studies should be conducted to evaluate health practitioners’ attitude and behaviour of antibiotics prescription in children and adults.
Conclusion
Overall, in this study it was found that misconceptions exist about the use and indications of antibiotics. Lack of knowledge regarding antibiotic resistance was prevalent. Confusion was more among female and those with lower formal education. But participants were aware of the risks associated with use of excessive antibiotics. More interaction with paediatricians and involvement of mass media can help to improve the antibiotics knowledge and practices among parents and thus, control the problem of antibiotic resistance. Stringent laws need to be enforced by the government to restrict the access of antibiotics to parents without a prescription.
* indicates correct response which was scored as 1 point each