The kidney proper reacts in a limited number of ways to myriad injurious agents. The clinical manifestations corresponding to these reactions are also limited [1]. Involvement of the renal pelvis by diseases is rare, and includes developmental, reactive and neoplastic disorders causing pelviureteric junction (PUJ) obstruction [2]. One of the most common consequences of PUJ obstruction is hydronephrosis [3]. Upper urinary tract tumours involving the renal pelvis and ureter are relatively uncommon accounting for less than 5% of renal tumours and less than 1% of genitourinary neoplasms [4]. The present study was undertaken to analyse the clinicopathological properties of the renal pelvic and PUJ lesions encountered over a period of 13 years in our institution.
Materials and Methods
The collection of the cases comprised a retrospective study of all the nephrectomies and PUJ resections submitted for histopathological evaluation to the Department of Pathology over a period of 13 years from July 2001 to June 2013. A total of 476 cases were retrieved. Renal parenchymal biopsies and autopsy specimens of the kidney were excluded from the study. Among 476 cases, 410 cases were nephrectomies, 64 cases were PUJ resections and 2 were referred for second opinion. Those cases which had lesions involving the renal pelvis and PUJ junction formed the core group of this study and was noted in 105 out of 476 cases (39 nephrectomies; 64 PUJ resections; 2 slides for second opinion). The renal cortex and medulla was the primary site of involvement in the remaining 371 cases and were not included in the analysis. Clinical information was obtained from the medical archives and the variables analysed were patient age, gender, clinical presentation and investigations. Macroscopic findings were retrieved from the pathology reports along with the anatomic location of the lesions and the laterality. The histopathological findings were reviewed and in the neoplastic lesions particular importance was given to the pathologic subtype, associated lesions, tumour grade and stage, as per the 2004 WHO criteria [5].
Results
Among 105 out of 476 specimens that exclusively involved renal pelvis and PUJ, 72 patients (68.6%) were men and 33 (31.4%) women. The mean age was 54.5 years (range 10 days – 78 years). The 105 cases were segregated into non-neoplastic and neoplastic categories. The non-neoplastic lesions accounted for 76.2% cases and were further classified as congenital, hamartomatous, non-neoplastic proliferations of renal pelvic urothelium and inflammatory. The neoplastic lesions were sub-divided into benign and malignant tumours. [Table/Fig-1] describes the main clinicopathological findings for the 105 cases that involved renal pelvis and PUJ.
Clinical characteristics of renal pelvic and pelviureteric junction lesions.
| Lesions | Number(%) | AgeRange(Mean Age) | Male: FemaleRatio | Right: Left SideRatio | Most CommonPresentation |
|---|
| Non-neoplasticCongenital lesionsPUJ obstruction due to inflammation induced fibromuscular hypertrophyDue to abnormal organisation of smooth muscle bundlesHamartomatous lesionsFibroepithelial polypsNon-neoplastic proliferation of renal pelvic urotheliumVon Brunn’s nests with ureteropyelitiscystica et glandularisFlat urothelial hyperplasiaInflammatoryTuberculosis | 80(76.2%)72(68.6%)61(58.1%)11(10.5%)01(0.9%)01(0.9%)01(0.9%)05(4.8%) | 10d-78y52.7years10d-65y(21.6 years)--73years78years50years24y-50y(40.8years) | 1.6:11.6:1-----1.5:1 | -1.3:1-----1.5:1 | --Abdominal massAbdominal massAbdominal massAbdominal painAbdominal painAbdominal pain |
| NeoplasticBenign tumoursIntramuscular hemangioma of upper ureter at PUJMalignant tumoursUrothelial tumoursInfiltrating urothelial carcinomai) Infiltrating urothelial carcinomaii) Infiltrating urothelial carcinoma with squamous differentiationiii) Sarcomatoid variantNon-invasive urothelial neoplasmsi) Non-invasive papillary urothelial neoplasm, Low gradeii) Non-invasive papillary urothelial neoplasm, High gradeSquamous cell carcinoma | 25(23.8%)01(0.9%)24(22.9%)21(20%)150101030103(2.9%) | 35-71years(59.1years)35years-35y-71y(55.7years)-----55yrs-68yrs(62.6years) | 3.2:1-3:13.2:1-----2:1 | 2.1:1-2:11.6:1-----All three right sided | -Abdominal pain-Painless hematuria-----Abdominal pain |
PUJ obstruction due to inflammation induced fibromuscular hypertrophy with associated hydronephrosis was the most common non-neoplastic lesion in our study accounting for 68.6% of cases. Abdominal mass due to hydronephrosis was seen in all these cases (72 cases, 100%). Other clinical manifestations were abdominal pain (40.3%), recurrent urinary tract infections (27.8%) and haematuria (2.8%). The PUJ obstruction was further sub-categorized depending on the pathology; i.e. secondary to inflammation induced fibromuscular hypertrophy (84.5%) or abnormal organization of smooth muscle bundles (15.3%).
A solitary pelviureteric fibroepithelial polyp (FEP) was seen in a 73-year-old woman who presented clinically with hydronephrosis. Grossly, the pelvicalyceal system was dilated and showed an elongated, 2.5cm long, grey white polyp arising in the distal pelvis and extending into the upper ureter.
The nephrectomy specimen of a 78 year old man showed von Brunn’s nests in the renal pelvic urothelium with associated ureteropyelitiscystica and chronic pyelonephritic changes. Flat urothelial hyperplasia of the PUJ associated with a calculus and hydronephrosis was noted in a nephrectomy specimen of a 50-year-old man.
While our geographic locale is non-endemic for infections such as schistosomiasis, it continues to be endemic for tuberculosis. We encountered 5 cases (4.8%) of tuberculosis (TB) affecting the renal pelvis and PUJ. The clinical manifestations of these patients included mass due to hydronephrosis (80%), haematuria (60%), and pain abdomen (40%) and associated renal calculi (20%). Urine culture did not yield any organisms. Grossly, the nephrectomy specimens showed chronic pyelonephritic changes with fibrous scarring and distortion of pelvicalyceal system and areas of caseous necrosis. Microscopically, characteristic caseating epithelioid granulomas and Langhan’s giant cells were noted.
An intramuscular haemangioma was detected in the PUJ of a 35-year-old woman who presented with abdominal pain. Grossly, it showed congestion of the renal pelvis and on microscopy lobules of proliferating capillaries with focal cellular spindle cell proliferation in the intramuscular layer was noted.
Renal pelvic tumours represented 11.2% of all kidney tumours surgically treated at our institution. The mean age of all the neoplastic lesions was 59.1years. Using the 2004 WHO classification of tumours of urinary tract, the malignant tumours were categorized [Table/Fig-1].
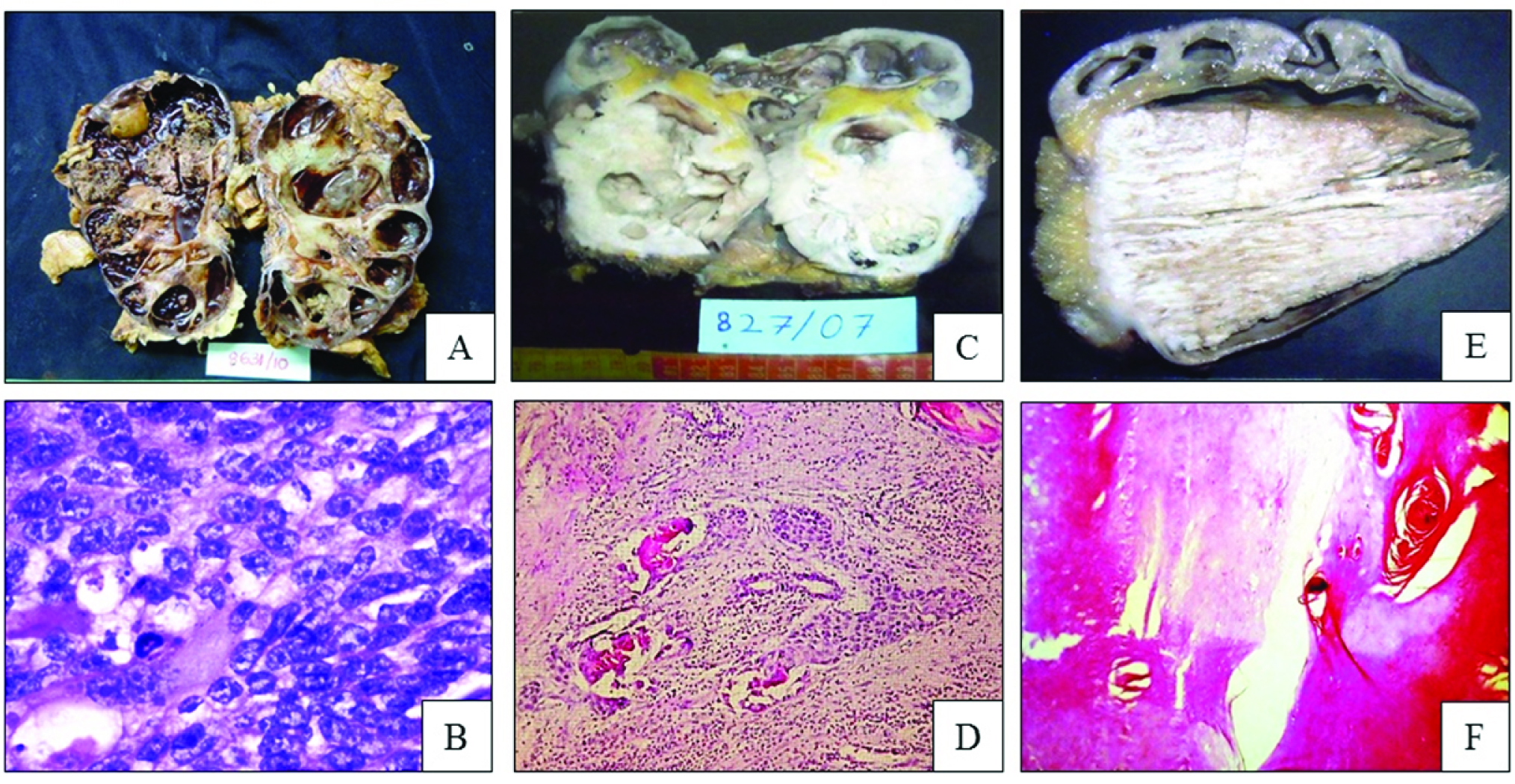
The commonest malignant tumour encountered was infiltrating urothelial carcinoma seen in 15 cases [Table/Fig-2a&b], while non-invasive urothelial neoplasms accounted for 4 tumours. All three cases of squamous cell carcinoma (SCC) had a history of long standing urolithiasis with associated hydronephrosis and on histology were well differentiated tumours. One peculiar case had a huge keratin horn filling and markedly distending the renal pelvis with a rim of invasive squamous cell carcinoma at the base of the horn. Along with this, the distended pelvicalyceal system was filled with more than 200 small stones.
a) Multifocal urothelial carcinoma showing multiple foci of grey white granular tumour tissue; b) Urothelial carcinoma showing nests and sheets of malignant tumour cells. (H&E, 200x); c) Squamous cell carcinoma of renal pelvis showing a diffuse grey white mass infiltrating into the lower pole of kidney; d) Squamous cell carcinoma showing nests of malignant squamous cells infiltrating the stroma and some showing keratin pearls. (H&E, 40x); e) Squamous cell carcinoma with a huge keratin horn filling and markedly distending the renal pelvis; f) Microscopy of the same shows multilamellated keratin (H&E, 40x).
Discussion
Renal pelvis can be affected by various non-neoplastic and neoplastic lesions. However, there are only few comprehensive studies discussing the various lesions of this specific anatomic site. Pelviureteric junction obstruction can present at any age. It is more frequently seen in the left side and boys are more commonly affected [2,6,7]. It is a congenital anomaly caused either due to intrinsic narrowing of the upper ureter or by extrinsic pressure on the ureter caused by aberrant vessels or fibrous bands [8]. Left sided involvement with male predilection and intrinsic narrowing of the upper ureter secondary to fibromuscular hypertrophy was the commonest aetiology for PUJ obstruction in the present study. As in the case of Johnston et al., in present study too, the commonest presenting feature was abdominal mass followed by abdominal pain [7].
Fibroepithelial polyps are rare benign tumours of the renal pelvis, which can mimic urothelial neoplasms and renal cell carcinomas on radiological imaging and hence, should be evaluated with caution. They demonstrate a wide age range with an average age of 40 years. While 65% of renal pelvic FEPs occur in women, 61% of ureteral lesions are seen in men [9,10]. They generally present as solitary exophytic polypoidal lesions frequently producing colicky abdominal pain and may be associated with haematuria [9,10]. These polyps may vary from 1 to 15 cm in length, are usually solitary but rarely, multiple clustered polyps may occur [9,10]. The literature has revealed multiple synonyms for this benign lesion, which is currently believed to be hamartomatous, by consensus [9–12].
Proliferative and metaplastic lesions of the urothelium are commonly encountered in the urinary bladder, but can be observed in any part of urinary tract [11]. Von Brunn’s nests are the small nests of urothelium within the lamina propria that are commonly encountered in bladder trigone but are seen in the PUJ of 10% cases at autopsy [13]. Von Brunn’s nests with central lumina lined by urothelium or columnar glands are designated ureteropyelitis cystica and ureteropyelitis glandularis, respectively. Such changes are commonly associated with calculi [14]. Simple flat urothelial hyperplasia indicates an increase in the layers of urothelium from the usual three or five to more than seven layers, usually associated with inflammation or neoplasia [11].
Genitourinary TB is the result of secondary haematogenous spread of tubercle bacilli, most commonly from the lung but rarely from other organs. Tubercle bacilli lodge in the corticomedullary junction of the renal parenchyma and form cortical granulomas. The granulomas may remain stable for many years and subsequently spread to the medulla and renal pelvis. Genitourinary TB exhibits features of local organ dysfunction rather than systemic symptoms such as fever, weight loss and anorexia. Urinary obstruction is commonly encountered leading to hydronephrosis, secondary to fibrous strictures formed by healed tubercular ulcers [15]. Upper urinary tract tumours involving the renal pelvis and ureter are relatively uncommon and seen in less than 5% of renal tumours. Ninety five percent of renal pelvic tumours are epithelial and 80% are malignant [4]. In the present study, renal pelvic tumours accounted for 11.1% of renal tumours. Ninety six percent of them were malignant and 4% benign. Haemangioma of the renal pelvis and ureter are extremely rare, occurring in both children and adults. They can be multiple and frequently cause obstruction. Histology reveals fibrous stroma separating lobules of capillary and cavernous channels, covered by an unremarkable urothelium [2]. An overwhelming majority of upper urinary tract tumours are transitional cell type, with a small number being either squamous or glandular. Urothelial tumours of renal pelvis are most common in older individuals with a mean age of 60 to 65 years. Men are affected in more than 70% of cases. Urothelial tumours usually present with painless haematuria in 80% of the cases. Flank pain and mass are detected in 20% and 10% cases, respectively [2,11]. Most of our cases presented with haematuria (90.5%), abdominal pain (57.1%) and a palpable mass (47.6%). Obstructive hydronephrosis was seen in 85.7% of cases. In the present study, urothelial tumours accounted for 84% of renal pelvic tumours. Since the area where this study was conducted is not in the industrial belt, the high incidence of urothelial carcinoma was probably not due to occupational carcinogenic exposure. Men were more commonly affected with the youngest being a 35-year-old and the oldest, 71-year-old. Korkes et al., reported 61% of renal urothelial tumours to be left sided, which concurred with our findings [4]. Urothelial carcinoma of the renal pelvis may be papillary or non-papillary types, each being further graded as low and high grade, depending upon the nuclear pleomorphism and architectural abnormalities [16]. In the study by Korkes et al., infiltrating high grade urothelial carcinoma accounted for 58% of renal pelvic tumours [4]. In the present study, 81% were infiltrating carcinomas and 19% papillary urothelial carcinomas. High grade tumours accounted for 71.4% and low grade for 28.6% cases. As per the WHO TNM classification, in our study, 42.9% had stage T3 lesions and 38.1% stage T4. The incidence of higher grade and stage tumours was thus more common in the present series [Table/Fig-3].
Distribution & comparison of renal pelvic tumours according to grade and stage
| Tumour type | Grade | Ta | Tis | T1 | T2 | T3 | T4 | Total |
|---|
| Korkes et al., [4] (2006) | LGHGTotal % | 070029.2% | 000000 | 010212.5% | 010212.5% | 010837.5% | 00028.3% | 1014100% |
| Present study(2013) | LGHGTotal % | 040019.1% | 000000 | 000000 | 000000 | 020742.9% | 000838.1% | 0615100% |
SCC of renal pelvis is the second most common epithelial neoplasm. Approximately 300 cases of SCC arising in the renal pelvis are reported in the literature and account for 6.1% of the upper urinary tract tumours [11]. There is a male preponderance, a peak age of 5th to 6th decade and a strong association with nephrolithiasis and chronic inflammation [4]. In the present study, SCC accounted for 2.9% of all the renal pelvic tumours [Table/Fig-2c&d]. Men were more commonly affected and the mean age was 62.6 years. Concurrent lithiasis was documented in all the cases of SCCs of the renal pelvis [11]. We encountered a peculiar case of SCC of the renal pelvis with a superimposed keratin horn overlying this lesion in an overtly distended renal pelvis [Table/Fig-2e]. The calyces were dilated and the renal parenchyma was atrophic. More than 200 stones were seen around the horn and in the calyces. Microscopically, the horn showed multi lamellated keratin [Table/Fig-2f], at the base of which was a moderately differentiated SCC extending through the pelvic wall into the peri-pelvic adipose tissue. It, however, did not infiltrate the renal parenchyma. The lining of the pelvis showed keratinizing squamous metaplasia with dysplasia. Rare reports in the literature have documented that the keratinisation may form cholesteatoma like masses, and desquamate into the passage [17,18]. When persistent, it is a risk factor for the development of dysplasia and SCC. To the best of our knowledge, this is the first such case of a non-cutaneous keratin horn occurring in the renal pelvis.
Conclusion
We conclude that the renal pelvis is more often affected by non-neoplastic diseases (76.2%) than neoplasms (23.8%) and due to the strategic location of these lesions, even patients with non-neoplastic conditions may present with abdominal masses with or without pain that the clinicians and radiologists may interpret as neoplasms, but the histopathological evaluation proves to be a hydronephrotic enlargement of the kidney. Apart from common lesions such as PUJ obstruction due to inflammation induced fibromuscular hypertrophy and urothelial neoplasms, rare lesions like FEPs, von Brunn’s nests, haemangioma and SCCs can also occur at this site and treatment differs in these patients. Knowledge about these rare lesions will aid in planning the further management of the patients.