Malignant Mixed Mullerian Tumour of the Ovary (OMMMT), also referred to as carcinosarcoma is a very rare tumour accounting for less than 1% of all ovarian cancers. Due to the rarity of OMMMT, little is known about the disease course and outcome of women with these tumours. It is important to evaluate because of its aggressive behaviour with extremely unfavourable prognosis. These tumours are composed of both malignant epithelial and mesenchymal elements. Current data in the literature is still limited to small case series and case reports, therefore, its optimal treatment is somewhat controversial. In the current report, we introduce a case of OMMMT which was successfully treated with Platinum-based combination chemotherapy after optimal cytoreductive surgery. The clinical manifestations, pathologic characteristics, diagnosis and management of these tumours are reviewed here. Although the most effective treatment is currently unknown, optimal cytoreductive surgery and platinum-based chemotherapy appears to improve the outcomes. Despite the aggressive nature of this tumour and its poor response to the treatment, management works best when cancer is found early. The stage of the disease is the most important prognostic factor. Therefore, the crucial question is how to diagnose the cancer at earlier stages rather than seeking the optimal treatment.
Cytoreductive surgery, Ovarian neoplasms, Platinum-based chemotherapy
Case Report
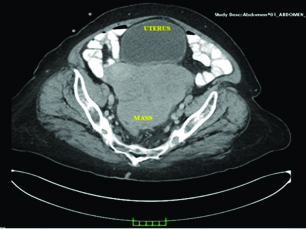
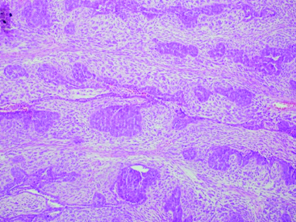
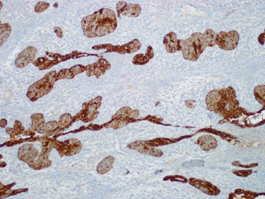
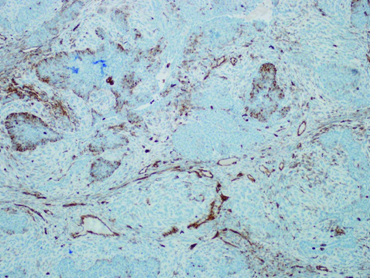
A 65-year-old, G3, P3 woman referred to gynaecology clinic due to sensation of fullness in the pelvis and a palpable mass in the abdomen since 2 weeks. She had a medical history of osteoarthritis, hypertension and non-insulin-dependent diabetes mellitus. The patient’s body mass index was 36 kg/m2. Physical examination revealed a large palpable, relatively mobile, non-tender mass in the pelvic region. Ultrasound demonstrated a loculated heterogeneous, cystic mass in pelvis and mild free fluid in the Pouch of Douglas. The lesion had mixed echogenicity with hypo echoic and hyper echoic components, contained solid parts within distinct margins, and were 18cm×15cm×12cm in size. Computed tomography was performed because the lesion extended beyond the pelvis [Table/Fig-1]. Computed tomography showed a large complex, well-circumscribed mass measuring 18 cm in the largest transverse diameter occupying the pelvis. Her CA-125 levels were 36U/L. Based on the clinical findings and imaging studies malignancy was highly probable, so the patient was prepared for surgery. The patient underwent an exploratory midline laparotomy from above the umbilicus to the symphysis pubis. At surgery, the pelvic and abdominal organs were closely inspected. The tumour originated from the left ovary and abdominal ascites was noted. The gross appearance of the tumour was predominantly solid and lobulated mass, with varying degrees of haemorrhage and necrosis. We found that no organ was infiltrated, and the right ovary was atrophied. Peritoneal washings were obtained. Frozen section revealed a malignant tumour. The patient then underwent comprehensive surgical staging procedures, including transabdominal hysterectomy and bilateral salpingo-opherectomy, infracolicomentectomy and bilateral pelvic and para-aortic lymphadenectomy. A histopathological examination demonstrated Malignant Mixed Mullerian Tumour of the Ovary (OMMMT) and the patient was diagnosed with surgical stage IA disease [Table/Fig-2,3 and 4]. Adjuvant chemotherapy consisting of systemic Paclitaxel (175 mg/m2) and Carboplatin (area under the curve = 6.0) every 3 weeks for six cycles was offered. The patient tolerated chemotherapy well without any significant adverse events. Currently, one year after completing the chemotherapy, the patient showed no evidence of recurrent disease.
Computed tomography showed a large complex, well-circumscribed mass measuring 18 cm in the largest transverse diameter occupying the pelvis.
Histopathologic examination of the mass (Haematoxylin and Eosin Staining x 10). Cells forming rosette like structures and various types of sarcomatous components. OMMMT of the ovary has been classified depending on the characteristics of the stroma. These stromal components may be either homologous (composed of tissues native to the ovary) or heterologous (containing tissues not normally found in the ovary, most commonly malignant cartilage or skeletal muscle). The epithelial component is often classified as serous, endometrioid or undifferentiated adenocarcinoma but may also represent clear cell adenocarcinoma or squamous cell carcinoma.
Pancytokeratin positivity in serous epithelial areas (PanCK x 10).
Focal vimentin expression in epithelial and stromal compartment (vimentin x 10).
Discussion
OMMMT, also referred to as carcinosarcoma, is a rare clinical entity, and account for less than 1% of all ovarian cancers [1–3]. It occurs most commonly in postmenopausal women of low parity and often present with disseminated disease at diagnosis [2]. These tumours represent one of the most highly aggressive cancers of female genital tract with poor long-term prognosis [2,3].
OMMMT is rare but important to evaluate because of its aggressive behaviour with extremely unfavourable prognosis. Given the rarity of OMMMT, attempts to conduct prospective trials to illuminate treatment strategies have been mostly elusive [3]. OMMMT is staged according to FIGO criteria for ovarian cancer [1]. Almost 75% of patients present with advanced (Stage III or IV) disease [2]. As a result, the average survival for a woman diagnosed with OMMMT is less than 2 years [2–4]. With regard to poor prognostic factors, the survival for both early and late stage OMMMT is inferior to serous ovarian tumours [4]. Regardless of the treatment, outcomes appear to be poor for women with OMMMT.
Proposed risk factors include obesity, nulliparity, exogenous oestrogen, and long-term Tamoxifen use [5]. Similarly our patient was also obese. Histopathologically, they are biphasic tumours that contain both carcinomatous malignant epithelial and sarcomatous mesenchymal components. It is believed that the predominance of the stromal component aggravates the prognosis, and it is associated with poor response to treatment [1,6]. On the other hand, some other studies have suggested that sarcomatous type was not considered a prognostic factor [7]. According to more recent reports, the histology has no clear influence on patient outcome [2].
These tumours are typically large, ranging from 15-20 cm in diameter [3]. In the present study, the tumour size was large too, with a maximal diameter exceeding 18 cm.
Similar to the reports in the literature, the present case also demonstrates that OMMMT is predominantly a disease of postmenopausal women. Le T et al., reported that the median age of the patients was 67.5 years [8]. All the women in the study of Loizzi T et al., were postmenopausal at the time of diagnosis, with an average age of 65 years [2]. Current data in the literature is still limited to small case series and case reports. Due to rarity of the disease there is not yet agreement regarding the optimal therapeutic procedures for treating this neoplasm [5,6]. Large series of studies about OMMMT are presented in [Table/Fig-5].
Large series of studies about malignant mixed mullerian tumour of the ovary.
| Author | N | Surgical intervention | Chemotherapy regimens | Survival | Stage | Median age |
|---|
| Present case | 1 | Optimal cytoreductiona | Platinum regimens | > 1 year (still alive) | I A | 65 |
| Loizzi T et al., [2] | 13 | TAH, Omentectomy, appendectomy (12)Laparoscopic peritoneal biopsies (1) | Platinum regimens (13) | > 2 years (2)< 2 years (11) | III C (12)IV B (1) | 65,5 |
| Rauh-Hain AJet al., [4] | 50 | Optimal cytoreductiona(37)Suboptimal cytoreductionb(10)Unknown (3) | Platinum regimens (50) | Median survival is 24 months (18 to 29) | III (48)IV (2) | 66,4 |
| Özgüroglu Met al., [6] | 9 | Optimal cytoreduction | Platinum regimens (9) | Not Available | II B (1)III A (2)III B (1)III C (4)IV (1) | 59 |
| Mok JE et al., [7] | 10 | Optimal cytoreductionc | Platinum regimens (10) | > 2 years (4)< 2 years (6) | II C (2)III C (7)IV (1) | 59 |
| Le T et al., [8] | 36 | TAH/BSO ± omentectomy (34) | Platinum regimens (29)Alkeran (2)RT alone (1)No adjuvant therapy (4) | Median survival of 3 years among patients treated with combination cytotoxic chemotherapy | Available 35/36I (2)II C (7)III C (23)IV (3) | 67,5 |
| Brown E et al., [9] | 65 | Optimally debulkedc (28)Suboptimallydebulkedd (27)Unknown debulking status (10) | Platinum regimens (37)Non-Platinum regimens (6)No CT (22) | Median survival: 8.2 months,2-year survival 23%5-year survival 15% | I (6)II C (6)III C (41)IV (11) | 66,6 |
| Crotzer DRet al., [10] | 10 | TAH/BSO/Tumour reductive surgery (7)TAH/BSO (1)Adnexectomy/Tumour reductive surgery (2) | Platinum regimens (10) | > 2 years (4)< 2 years (6) | II (1)III (2)IV (2)Unstaged (5) | 57 |
| Rutledge TLet al., [11] | 31 | All (12) of the patients with stage IIIB disease or less underwent complete surgical staging. | Platinum regimens (29) | The median survival is 21 months. | I (1)II (6)III (23)IV (1) | 67 |
| Sit AS et al., [12] | 13 | Optimal debulkeda (10)Suboptimallydebulkedb (3) | Platinum regimens (13) | > 2 years (5)< 2 years (8) | I C (1)II C (2)III C (10) | 63,6 |
| Zorzou MPet al., [13] | 9 | TAH/BSO + omentectomy (9) | Platinum regimens (3)Non-Platinum regimens (6) | Median survival is 32.9 months | IC (1)IIA (3)IIB (1)IIIA (1)IIIB (1)IIIC (2) | 68 |
| Cicin I et al., [14] | 26 | Optimal debulkingc (21)suboptimal debulkingd (5) | Platinum regimens (22)Non-Platinum regimens (3) | Median survival is 26 months | I (4)II (4)III (15)IV (3) | 60 |
Abbreviations: TAH, total abdominal hysterectomy; BSO, bilateral salpingooophorectomy; CT, Chemotherapy; RT, Radiotherapy
aLargest residual tumour nodule measuring 1 cm or less.
bLargest residual tumour nodule is greater than 1 cm.
cLargest residual tumour nodule is smaller than 2 cm.
dLargest residual tumour nodule is greater than 2 cm.
“N” and Number in the parentheses indicate the number of patients.
Patients typically present with abdominal symptoms, distension, and bloating, with or without a palpable pelvic or abdominal mass [2,8]. These symptoms are very likely to occur in the advanced stage of the disease. Unlike the majority of the published works, the cancer was detected in the early stage in the present case. It has been estimated that over 90% of women will have disease that has spread beyond the ovary, with one-third of cases involving both ovaries with ascites present [9]. However the lack of specific symptoms or findings on imaging or laboratory studies makes it difficult to identify timely. Although there is conflicting data in the literature on the significance of tumour markers [2,7] according to our study CA 125 was not useful for screening or diagnosis of OMMMT.
The most effective treatment is currently unknown but the preferred treatment for OMMMT consists of cytoreductive surgery followed by platinum-based chemotherapy. Most patients present with widespread metastases at the time of surgery, making optimal tumour debulking difficult [8].
Similar to epithelial ovarian cancer, large residuals (>2cm) and advanced stages are the two most important adverse prognostic factors [8]. It was reported in the study of Rauh-Hain AJ et al., that significant improvement were observed in disease-free survival and overall survival with optimal cytoreduction compared to those with suboptimal cytoreduction [4].
OMMMTs are highly chemo responsive tumours, irrespective of primary site [6]. Additionally, due to the aggressive nature of this tumour, systemic chemotherapy is usually recommended; especially it is advised in patients with stage II or higher [1]. Chemotherapy can be considered for stage I OMMMT. A variety of chemotherapy regimens have been reported in the literature consisting of Dacarbazine, Adriamycin, and Cisplatin [1,6]. Platinum-based combination chemotherapy after optimal cytoreductive surgery may be effective in the treatment with response rates ranging from 65% to 80% [1,7]. Adjuvant radiotherapy (external beam irradiation and/or vaginal brachytherapy) has not shown any overall survival benefit but has been reported to decrease local recurrences [15]. Stage of disease is the most important predictor for survival. Other prognostic factors relevant to a worse outcome in OMMMT include advanced age, residual tumour after initial surgery and suboptimal cytoreduction [6,8,9].
Conclusion
Although the most effective treatment is currently unknown, optimal cytoreductive surgery and platinum-based chemotherapy appears to improve the outcome. Despite the aggressive nature of this tumour and poor response to the treatment, management works best when cancer is diagnosed early. The stage of the disease is the most important prognostic factor. Therefore, the crucial question is how to diagnose the cancer at earlier stages rather than seeking optimal treatment. Large multi-institutional, prospective randomized controlled trials are required.
Informed Consent: Written informed consent was obtained from the patient who participated in this study.
Abbreviations: TAH, total abdominal hysterectomy; BSO, bilateral salpingooophorectomy; CT, Chemotherapy; RT, Radiotherapy
aLargest residual tumour nodule measuring 1 cm or less.
bLargest residual tumour nodule is greater than 1 cm.
cLargest residual tumour nodule is smaller than 2 cm.
dLargest residual tumour nodule is greater than 2 cm.
“N” and Number in the parentheses indicate the number of patients.
[1]. Duman BB, Kara IO, Gunaldi M, Ercolak V, Malignant mixed Mulleriantumour of the ovary with two cases and review of the literatureArch Gynecol Obstet 2011 283:1363-68. [Google Scholar]
[2]. Loizzi V, Cormio G, Camporeale A, Falagario M, De Mitri P, Scardigno D, Carcinosarcoma of the ovary: analysis of 13 cases and review of the literatureOncology 2011 80:102-06. [Google Scholar]
[3]. del Carmen MG, Birrer M, Schorge JO, Carcinosarcoma of the ovary: a review of the literartureGynecoloncol 2012 125:271-77. [Google Scholar]
[4]. Rauh-Hain AJ, Grodwon WB, Rodriguez N, Goodman AK, Boruta D, Schorge JO, Carcinosarcoma of the ovary: a case–control studyGynecol Oncol 2011 121:477-81. [Google Scholar]
[5]. Ma CJ, Yang SF, Huang CC, Chai CY, Cheng KI, Tsai EM, Malignant mixed mulleriantumour of primary mesenteric origin associated with a synchronous ovarian cancer: case report and literature reviewEur J Gynaecol Oncol 2008 29:289-93. [Google Scholar]
[6]. Ozguroglu M, Bilici A, Ilvan S, Turna H, Atalay B, Mandel N, Sahinler I, Determining predominating histologic component in malignant mixed mullerian tumours: is it worth it?Int J Gynecol Cancer 2008 18:809-12. [Google Scholar]
[7]. Mok JE, Kim YM, Jung MH, Kim KR, Kim DY, Kim JH, Malignant mixed mulleriantumours of the ovary: experience with cytoreductive surgery and platinum-based combination chemotherapyInt J Gynecol Cancer 2006 16:101-05. [Google Scholar]
[8]. Le T, Krepart GV, Lotocki RJ, Heywood MS, Malignant mixed mesodermal ovarian tumour treatment and prognosis: a 20-year experienceGynecol Oncol 1997 65:237-40. [Google Scholar]
[9]. Brown E, Stewart M, Rye T, Al-Nafussi A, Williams AR, Bradburn M, Carcinosarcoma of the ovary: 19 years of prospective data from a single centerCancer 2004 100:2148-53. [Google Scholar]
[10]. Crotzer DR, Wolf JK, Jenkins AD, Gershenson DM, Levenback C, A pilot study of cisplatin, ifosfamide and mesna in the treatment of malignant mixed mesodermal tumours of the ovaryProc Am Soc Clin Oncol 2003 22:474 [Google Scholar]
[11]. Rutledge TL, Gold MA, McMeekin DS, Huh WK, Powell MA, Lewin SN, Carcinosarcoma of the ovary-a case seriesGynecol Oncol 2006 100:128-32. [Google Scholar]
[12]. Sit AS, Price FV, Kelley JL, Comerci JT, Kunschner AJ, Kanbour-Shakir A, Chemotherapy for malignant mixed Mülleriantumours of the ovaryGynecol Oncol 2000 79:196-200. [Google Scholar]
[13]. Zorzou MP, Markaki S, Rodolakis A, Kastritis E, Bozas G, Dimopoulos MA, Clinicopathological features of ovarian carcinosarcomas: a single institution experienceGynecol Oncol 2005 96:136-42. [Google Scholar]
[14]. Cicin I, Saip P, Eralp Y, Selam M, Topuz S, Ozluk Y, Ovarian carcinosarcomas: clinicopathological prognostic factors and evaluation of chemotherapy regimens containing platinumGynecol Oncol 2008 108:136-40. [Google Scholar]
[15]. Berton-Rigaud D, Devouassoux-Shisheboran M, Ledermann JA, Leitao MM, Powell MA, Poveda A, Gynecologic Cancer InterGroup (GCIG) consensus review for uterine and ovarian carcinosarcomaInt J Gynecol Cancer 2014 24:55-60. [Google Scholar]