Uterine Fibroid (Leiomyoma) with Acute Urinary Retention: A Case Series
Sweta Singh1, Saubhagya Kumar Jena2, Monalisha Naik3, Lipsa Ray4, Satyanarayan Behera5
1 Assistant Professor, Department of Obstetrics and Gynaecology, All India Institute of Medical Sciences, Bhubaneswar, Odisha, India.
2 Assistant Professor, Department of Obstetrics and Gynaecology, All India Institute of Medical Sciences, Bhubaneswar, Odisha, India.
3 Senior Resident, Department of Obstetrics and Gynaecology, All India Institute of Medical Sciences, Bhubaneswar, Odisha, India.
4 Senior Resident, Department of Obstetrics and Gynaecology, All India Institute of Medical Sciences, Bhubaneswar, Odisha, India.
5 Senior Resident, Department of Obstetrics and Gynaecology, All India Institute of Medical Sciences, Bhubaneswar, Odisha, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sweta Singh, Assistant Professor, Department of Obstetrics and Gynaecology, All India Institute of Medical Sciences (AIIMS), Bhubaneswar, Odisha-751019, India.
E-mail: swetsingh@hotmail.com
Uterine leiomyomas are an extremely rare cause of acute urinary retention in women. The delay in diagnosing uterine leiomyomas presenting with acute urinary retention further complicates the management. The rarity of the condition makes it difficult to plan either prospective or retrospective trials. Hence, most of the evidence comes from case reports or series. We report a case series of acute urinary retention in women with uterine leiomyomas and discuss the pathophysiology, diagnosis and management options.
Myomas, Pathophysiology, Uterine obstruction
Case Series
We present a single institution case series of women who presented with acute urinary retention due to uterine leiomyomas and discuss the pathophysiology, diagnosis and management.
The data of 4 women, who presented to our institute with acute urinary retention due to uterine fibroids from April 2014 to March 2015 were prospectively collected and retrospectively analysed. Women with urinary retention in the same period due to other causes like pregnancy, neurological disorders or psychosomatic illnesses were excluded from the analysis.
The age, parity, duration of symptoms and modality of treatment were recorded. Any previous surgical and/or urological consultations for acute urinary retention were also documented. The location and size of the tumours were documented during the initial preoperative scans {ultrasound/Computed Tomography (CT)} and also at operation. Renal function tests including routine urine examination were recorded to document baseline renal function. Case details are presented in [Table/Fig-1].
Patient demographics, symptoms, clinical findings, investigations and surgical details [Table/Fig-2,3,4,5 and 6].
| Patient | Age(years) | Parity | Symptoms | Clinical findings | Investigations | Surgery |
|---|
| 1 | 42 | 3 | Retention of urine – 5 days, urination only on pressure; burning micturition; had surgical consultation before and was referred; cycles regular, normal flow. | P/ A- Mass 16 weeks P/S- cervix deviated anteriorly P/V- uterus 16 weeks with a large posterior myoma. | Hb-11.2 g% USG- uterus 12.9 X 4.3 X 10.3 cm, with a large posterior fibroid measuring 7.8 X 6 cm [Table/Fig-2a] and a smaller anterior fibroid of 3.8 X 3 cm; ureters normal, bilateral mild hydronephrosis Urine C/S- Enterococcus 104/HPF Renal functions-within normal limits | TAH with BSO done. Findings- Uterus 16 weeks, posterior sub serous fibroid just above cervix on left side measuring 7 X 6 cm [Table/Fig-2b]; smaller anterior sub- serous fibroid measuring 4 X 3cm. |
| 2 | 36 | 2 | Incomplete evacuation of bladder since 9-10 months; history of acute urinary retention for which catheterisation was done 7 months back; urology consultation done; cycles regular, normal flow. | P/A- uterus 16 weeks P/S- cervix healthy P/V- Uterus irregularly enlarged to 16 weeks with posterior myoma. | Hb- 12.4 g% USG-Uterus 14.2 X 9.6 X 8.4 cm. Right fundal region intramural myoma 5.5 X 5.3 cm, another smaller myoma 2.7 X 2.5 cm; ureters normal, no hydronephrosis Urine routine examination and renal function-within normal limits. | TAH done; Findings- Large fundal fibroid present [Table/Fig-3]; another smaller myoma present. |
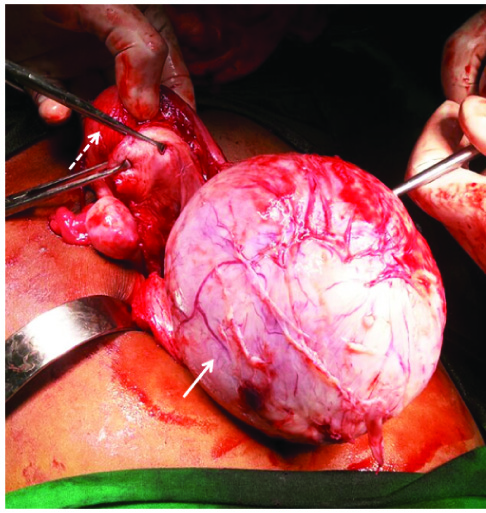
| 3 | 25 | 0 | Dysmenorrhoea; increased frequency of micturition & tenesmus with episodes of acute retention of urine– 2 months; cycles regular, normal flow. | P/A- Uterus 16-18 weeks, firm with restricted mobility P/S & P/V- Not done (patient unmarried). | Hb- 11.0g% USG- Single large cervical fibroid 9.3 X 9.2 cm in continuity with posterior wall of uterus [Table/Fig-4a]; CECT- Homogenously enhancing solid mass of size 11.0 X 10.5 cm seen in continuity with right postero-lateral wall of uterus; uterus and bilateral ovaries normal [Table/Fig-4b]; bilateral hydroureter with hydronephrosis Left > right Urine routine examination and renal function-within normal limits. | Myomectomy done. Findings-15 X 10 cm cervical fibroid, uterus normal [Table/Fig-5]. |
| 4 | 39 | 2 | Pain during micturition-7 days; inability to pass urine 5 days; had urology consultation with indwelling catheterisation; menorrhagic cycles for last 5 months. | P/A-Uterus enlarged to 14 weeks in size P/S-cervix healthy P/V- Uterus 12-14 weeks in size, firm, mobile, fornices free. | Hb- 11.0 g%) USG- Uterus 11.8 X 8.9 X 6.8 cm with a large anterior wall intramural fibroid 6.7 X 5.9 cm [Table/Fig-6a]; no hydronephrosis or hydroureter Urine routine examination and renal function tests- within normal limits. | TAH done. Findings- Anterior wall fibroid of size 7 X 7 cm [Table/Fig-6b]. |
P/A- per abdomen; P/S- per speculum; P/V- per vaginum; Hb- haemoglobin; C/S – culture sensitivity; HPF- high power field; USG- ultrasonography; CECT- contrast enhanced computed tomography; TAH- total abdominal hysterectomy; BSO- bilateral salpingo-oophorectomy
a) Trans abdominal ultrasonography showing posterior myoma (dashed arrow) measuring 7.8 X 6 cm indenting the urinary bladder; bulb of the Foley catheter can also be seen (arrow) and b) The operative specimen showing the large posterior myoma (black arrow) measuring approximately 7 X 6 cm.

Large fundal myoma (black arrow) on right side of uterus measuring 8.5 X 7.5 cm

a) Trans abdominal ultrasonography showing large cervical fibroid (arrow) measuring 9.3 X 9.2 cm with normal sized uterus (dashed arrow) seen on top and b) CECT- large homogenously enhancing solid myoma mass (arrow) measuring 11 X 10.5 cm seen posterior to the bladder (arrow head).

Intraoperative photograph showing normal size uterus (dashed arrow) and large cervical fibroid (arrow) measuring 15 X 10 cm, for which myomectomy was done.
a) Trans abdominal ultrasonography showing anterior wall myoma (arrow) measuring 6.7 X 5.9 cm and b) Intraoperative picture of the anterior myoma (arrow), which measured 7 X 7 cm.

Discussion
Uterine fibroids (myomas, leiomyomas) are an extremely rare cause of acute urinary retention with only a few case reports and series documented in literature [1–4]. Given the rarity of the condition, no prospective or retrospective studies have been attempted and hence, there are no clear consensuses or guidelines available to deal with women presenting with acute urinary retention secondary to leiomyomas. Only a single case report of acute urinary retention due to uterine leiomyoma has been reported previously from India [5].
Leiomyomas are the commonest benign pelvic tumours in women and occur in 20-30% of women in the reproductive age group [6,7]. Most women are asymptomatic with only 25% manifesting symptoms [8]. Symptoms correlate with size, site, number and degenerative changes within the tumour and range from abdominal mass, menorrhagia, dysmenorrhea, pain and recurrent abortions to constipation and tenesmus [7,9–11].
A recent review of literature by Wu et al., revealed a total of 37 cases only in literature of uterine leiomyomas causing acute urinary retention (16 case reports and 5 case series); this included their own case series of 6 patients with acute urinary retention [1]. Various mechanisms have been postulated by which acute urinary retention may occur due to a leiomyoma. The commonest theory is that the proximal urethra and bladder neck compression may be caused by anterior and superior displacement of the cervix due to the impacted fibroid. In normal voiding, the cervix is rotated away from the urethra/bladder neck; this movement is hindered by the impacted uterine fibroid [12–14].
A direct compression of only the lower portion of the bladder due to anterior and superior displacement of the cervix has also been postulated; a collapse of the lower bladder during supine position may lead to inadequate urine drainage into the urethra [1]. Other proposed mechanisms include pelvic congestion due to premenstrual hormonal induced factors [1], detrusor muscle ischemia due to vascular steal effect of the fibroid [15], and stretching of nerves that innervate the bladder, i.e., the pudendal and sacral nerves by the fibroid [16].
Rather than the actual size, impaction or incarceration of a leiomyoma or the uterus in the hollow of the sacrum may also be a critical factor for the development of acute urinary retention in the majority of cases [1]. This is borne out by the fact that very large uterine leiomyomas often do not cause acute retention of urine as they grow out of the sacral promontory freely without entrapment into the hollow of the sacrum [1].
Age, duration of symptomatology and size of the leiomyomas in our series were as reported in literature. Yazdani et al., reported that patients presenting to other specialities like urology had a delay of 14 months from diagnosis to surgery whereas this diagnosis-surgery delay was approximately 2.1 months in women who presented to gynaecology [17]. Similarly, in our patients, we found that patients presenting to other specialities like urology had a delay of 6 months from diagnosis to surgery whereas this diagnosis-surgery delay was approximately 2 months in women who presented to gynaecology.
Pelvic Ultrasonography (USG) is usually the first modality of imaging and used to both diagnose as well as monitor the growth of leiomyomas [18]. Both transabdominal as well as transvaginal ultrasound are recommended; transvaginal scans are more sensitive for small fibroids [18]. Leiomyomas appear as well defined solid masses with a whorled appearance but sometimes may be hypoechoic as well. Areas of calcification may be seen as echogenic foci with shadowing; and there may be cystic areas suggestive of necrosis or degeneration within the tumour [18].
Doppler USG usually shows circumferential vascularity which may be absent in necrotic fibroids. CT scan is not the investigation of choice for diagnosing uterine leiomyomas; however, magnetic resonance imaging can accurately characterize pelvic masses and differentiate submucosal, intramural and subserosal fibroids [18]. Of note, in the absence of neurological disorders, urodynamic studies or neuromuscular testing are apparently non-contributory in either diagnosis or management of patients presenting with acute retention of urine due to uterine leiomyoma [1].
It is important to document the renal function as urinary obstruction may cause hydronephrosis with derangement of renal parameters. In our series, 2 patients had hydronephrosis and/or hydroureter, with renal function being essentially normal. Post-surgery, the hydronephrosis and hydroureter rapidly reverted to normal, thus underscoring the importance of early diagnosis and definitive treatment.
There is no current consensus on the management of urinary retention in patients with uterine leiomyomas [19]. Wu et al., have proposed an algorithm for the management of patients with acute urinary retention due to leiomyoma [1]. They suggest that short term management of acute urinary retention due to uterine leiomyoma (size ≥ 5-6 cm) is bladder decompression by catheterization, while long term management is based on either uterus preserving options (in whom fertility is desired) or hysterectomy in those who are menopausal. Pre/perimenopausal women may be tried with hysterectomy or GnRH agonists, aromatase inhibitors or ulipristal acetate.
Conclusion
The rarity of acute urinary retention in woman with uterine leiomyomas precludes the planning of any relevant prospective or retrospective trials. In this regard, the body of evidence from case reports/series form the crux of evidence on which to base management. Therefore, our case series of 4 patients with uterine leiomyomas presenting with acute urinary retention gain importance in adding to the existing level of evidence. In conclusion, acute urinary retention in women should raise the suspicion of uterine fibroids, which warrant both urgent symptomatic management as well as careful long term planning.
P/A- per abdomen; P/S- per speculum; P/V- per vaginum; Hb- haemoglobin; C/S – culture sensitivity; HPF- high power field; USG- ultrasonography; CECT- contrast enhanced computed tomography; TAH- total abdominal hysterectomy; BSO- bilateral salpingo-oophorectomy
[1]. Wu CQ, Lefebvre G, Frecker H, Husslein H, Urinary retention and uterine leiomyomas: a case series and review of literatureInt Urogynecol J 2015 26(9):1277-84. [Google Scholar]
[2]. Mavromatidis G, Dinas K, Mamopoulos A, Delkos D, Rousso D, Acute urinary retention due to a uterine fibroid in a non-pregnant womanClin Exp Obstet Gynaecol 2009 36:62-63. [Google Scholar]
[3]. Novi JM, Shaunik A, Mulvihill BH, Morgan MA, Acute urinary retention caused by a uterine leiomyoma: a case reportJ Reprod Med 2004 49:131-32. [Google Scholar]
[4]. Hosokawa Y, Kishino T, Ono T, Oyama N, Momose H, Two cases of female acute urinary retention caused by an impacted pelvic massInt J Urol 2005 12:1069-70. [Google Scholar]
[5]. Maimoon S, Wilkinson A, Mahore S, Bothale K, Patrikar A, Cotyledonoid leiomyoma of the uterusIndian J Pathol Microbiol 2006 49:289-91. [Google Scholar]
[6]. DeWaay DJ, Syrop CH, Nygaard IE, Davis WA, Van Voorhis BJ, Natural history of uterine polyps & leiomyomataObstet Gynaecol 2002 100:3-7. [Google Scholar]
[7]. Wallach EE, Vlahos NF, Uterine myoma: an overview of development, clinical features and managementObstet Gynaecol 2004 104:393-406. [Google Scholar]
[8]. Sterwart EA, Uterine FibroidsLancet 2001 357:293-98. [Google Scholar]
[9]. Wegienka G, Baird DD, Hertz-Picciotto I, Self-reported heavy bleeding associated with uterine leiomyomataObstet Gynaecol 2003 101:431-37. [Google Scholar]
[10]. Stovall DW, Clinical symptomatology of uterine leiomyomasClin Obstet Gynaecol 2001 44:364-71. [Google Scholar]
[11]. Ezeama C, Ikechebelu J, Obiechina NJ, Ezeama N, Clinical presentation of uterine fibroids in Nnewi, Nigeria: a 5 year reviewAnn Med Health Sci Res 2012 2:114-18. [Google Scholar]
[12]. Barnacle S, Muir T, Intermittent urinary retention secondary to a uterine leiomyomaInt Urogynaecol J Pelvic Floor Dysfunct 2007 18:339-41. [Google Scholar]
[13]. Yang JM, Huang WC, Sonographic findings of acute urinary retention secondary to an impacted pelvic massJ Ultrasound Med 2002 21:1165-69. [Google Scholar]
[14]. Ding DC, Hwang KS, Female acute urinary retention caused by anterior deflection of the cervix which was augmented by an uterine myomaTaiwan J Obstet Gynaecol 2008 47:350-51. [Google Scholar]
[15]. Arleo EK, Tal MG, Fibroid-induced acute urinary retention: treatment by uterine artery embolizationInt Urogynaecol J Pelvic Floor Dysfunct 2008 19:161-65. [Google Scholar]
[16]. Andrada AO, De Vicente JM, Cidre MA, Pelvic plexus compression due to a uterine leiomyoma in a woman with acute urinary retention: a new hypothesisInt Urogynaecol J 2014 25:429-31. [Google Scholar]
[17]. Yazdany T, Bhatia NN, Nguyen JN, Urinary retention and voiding dysfunction in women with uterine leiomyoma: a case seriesJ Reprod Med 2012 57:384-89. [Google Scholar]
[18]. Wilde S, Scott-Barrett S, Radiological appearance of uterine fibroidsIndian J Radiol Imaging 2009 19:222-31. [Google Scholar]
[19]. Lefebvre G, Vilos G, Allaire C, Jeffrey J, Arneja J, Birch C, Clinical Practice Gynaecology Committee, Society for Obstetricians and Gynaecologists of Canada. The management of uterine leiomyomasJ Obstet Gynaecol Can 2003 25:396-418.quiz 419-22 [Google Scholar]