Papillary Cystadenocarcinoma of the Parotid Gland: A Rare Case Report
Ramesh Babu Telugu1, Anjana Juanita Job2, Marie Therese Manipadam3
1 Assistant Professor, Department of General Pathology, Christian Medical College, Vellore, Tamilnadu, India.
2 Consultant, Department of ENT, Scudder Memorial Hospital, Ranipet, Vellore, Tamilnadu, India.
3 Professor, Department of General Pathology, Christian Medical College, Vellore, Tamilnadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ramesh Babu Telugu, Assistant Professor, Department of General Pathology, Christian Medical College, Vellore, Tamilnadu-632004, India.
E-mail: dr.rameshtelugu@gmail.com
Papillary cystadenocarcinoma is a rare malignant neoplasm of the salivary gland, characterized by noticeable cystic and solid areas with papillary endophytic projections. These tumours lack features that characterize cystic variants of several more common salivary gland carcinomas. It was first described in 1991 by World Health Organization as a separate entity and cystadenocarcinoma with or without papillary component in the AFIP classification. Most of these tumours occurred in the major salivary glands followed by minor salivary glands. Cystadenocarcinoma is the malignant counterpart of cystadenoma. We report a case of papillary cystadenocarcinoma of parotid. A 40-year-old lady presented with gradually progressive swelling below the right ear associated with occasional pain. Clinical and radiological features suggested benign neoplasm. Right lobe superficial parotidectomy was performed. The histopathologic diagnosis showed papillary cystadenocarinoma of the parotid gland. Histologic confirmation of stromal invasion is required to differentiate it from the benign lesion. Conservative wide local surgical excision is the treatment of choice.
Carcinoma, Malignant neoplasm, Salivary gland neoplasms
Case Report
A 40-year-old lady presented with gradually progressive swelling below the right ear since 10 years associated with occasional pain for the past three months. Physical examination revealed a 1.5x0.5cm hard mobile swelling below the right ear. Clinical features suggested pleomorphic adenoma. Ultrasonography performed outside in a private clinic showed a well-defined lobulated hypoechoic lesion of size 15.5x10x17.5mm in the superficial lobe of right parotid gland. No calcification was seen. No evidence of deep lobe involvement seen. Left parotid and bilateral submandibular salivary glands were normal in size and morphology. Few discrete subcentimeter sized lymphnodes of size 5-8mm were seen in level II and level Ib regions on both sides. Features were suggestive of a benign neoplasm. Possibilities included: 1) Pleomorphic adenoma; and 2) Warthin’s tumour. Right lobe superficial parotidectomy was performed and the specimen was sent to the Department of Pathology.
Gross examination revealed a salivary gland tissue measuring 3.5x3x1cm. Sectioning through the gland, demonstrated a circumscribed, unencapsulated lobular soft tissue mass measuring 1.2x0.7x0.4cm. Cut section was firm grey-white with partly solid and partly cystic [Table/Fig-1]. Rest of the salivary gland parenchyma grossly appeared unremarkable. A small lymph node was also sent in the same container measuring 0.5cm in diameter with a tan cut surface.
Gross specimen showing well circumscribed, unencapsulated soft tissue mass with solid (broad arrow) and cystic (narrow arrow) cut surface.

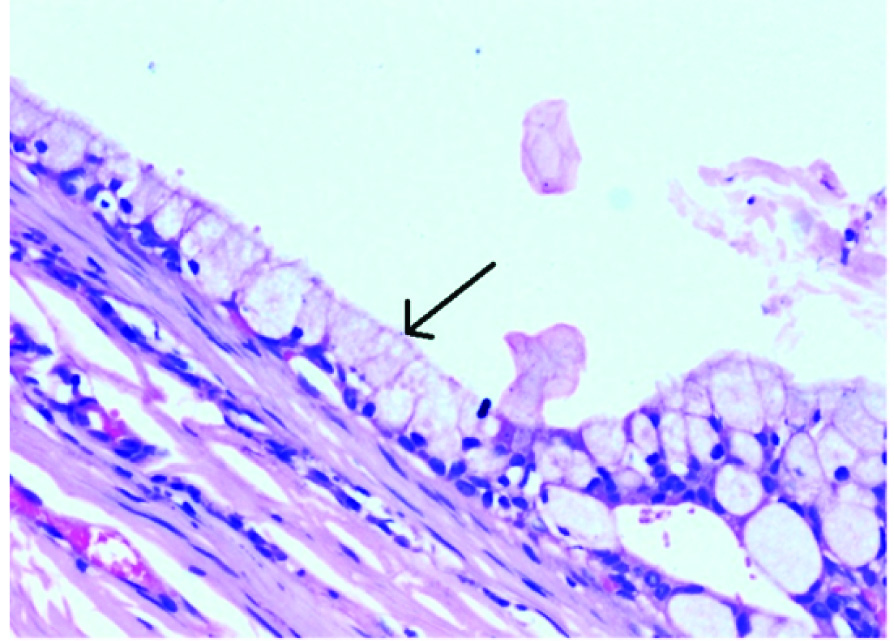
Microscopic examination revealed serous salivary gland tissue infiltrated by a circumscribed but unencapsulated tumour composed of predominantly cystic spaces of variable sizes with intracystic papillary and micropapillary proliferation [Table/Fig-2]. The tumour cells were uniform, low cuboidal with vescicular to hyperchromatic nuclei, inconspicuous nucleoli and moderate amount of eosinophilic to clear cytoplasm. Some tumour cells showed mild nuclear pleomorphism with vescicular nuclei and small visible nucleoli. Pseudostratification of intracystic papillae was seen. Focally the cyst was lined by mucus secreting cells [Table/Fig-3]. Some of the cysts were filled with Periodic Acid-Schiff –Diastase (PAS-D) stain positive mucin and cholesterol clefts. There was focal osseous metaplasia [Table/Fig-4]. Definite invasion of tumour cells into the fibrotic stroma was identified that confirmed the diagnosis of carcinoma [Table/Fig-5]. These findings suggested a diagnosis of papillary cystadenocarcinoma of the parotid gland. One lymph node was noted with reactive change. The patient was discharged and postoperative period was uneventful.
Photomicrograph showing: a) papillary cystadenocarcinoma with papillary projections (broad arrow) and variable cystic spaces (narrow arrow) (H&E x 100); b) papillary projections lined by single or double row of atypical cuboidal to columnar epithelial cells (broad arrow) (H&E x 200).

Photomicrograph of papillary cystadenocarcinoma of parotid with cystic space lined by mucus secreting cells (narrow arrow) (H&E x 200).
Photomicrograph showing papillary cystadenocarcinoma with variable cystic spaces and osseous metaplasia (H&Ex100).

Photomicrograph of papillary cystadenocarcinoma showing: a) infiltration of neoplastic epithelium (broad arrow) into the fibrotic stroma (narrow arrow) (H&Ex100); b) neoplastic epithelium with vescicular to hyperchromatic nuclei and occasional visible nucleoli (broad arrow) (H&E x 200).

Discussion
Papillary cystadenocarcinoma is a slow growing, asymptomatic, rare malignant tumour of the salivary gland neoplasms, characterized by prominent cysts and papillary endophytic projections, but lacking features that characterize cystic variants of several more common salivary gland carcinomas [1]. They account for about 2% of all salivary gland tumours. It was first described in 1991 by World Health Organization (WHO) as a separate entity and cystadenocarcinoma with or without papillary component in the Armed Forces Institute of Pathology (AFIP) classification [2]. It was included as cystadenocarcinoma in the recent 2005 WHO classification of head and neck tumours [1]. Previously this tumour was classified as malignant papillary cystadenoma, low grade papillary adenocarcinoma or mucus producing adenopapillary carcinoma [3]. In a study by Foss RD et al., there was no sex predilection [4]. Most of these tumours occurred in the major salivary glands (65%) followed by minor salivary glands (35%). In this series, the average age of patients was about 59 years and over 70 percent of patients were over 50 years of age.
Cystadenocarcinoma of the salivary gland is a distinct group of epithelial malignancy characterized by cystic and solid areas with luminal papillary projections, lined by cuboidal, columnar or mucus secreting cells. Malignant nature of tumour is confirmed by nuclear pleomorphism, mitosis and infiltrative growth pattern [5]. In our case, along with mucus secreting cells, osseous metaplasia was also seen.
In the largest series of 57 cases reported, grossly cysts of varying size (0.4–6.0cm) were identified. Microscopically, all tumours revealed cystic areas with stromal invasion and 75% of cases showed clearly visible papillary structures. In the AFIP series of cases, many cell types have been described. These are small cuboidal (60%), tall cuboidal (16%), and tall columnar (12%) with mixed cell types of mucous, clear, oncocytic and rarely, focal epidermoid cells [4,6].
Magnetic Resonance Imaging (MRI) is very important for confirming the mass lesion, to ascertain whether it is solid, necrotic or cystic, determining its relationship with the salivary gland, adjacent structures and extent of infiltration [7]. In the present case only ultrasonography was done that showed well defined lobulated hypoechoic lesion confined to the superficial lobe of right parotid gland.
Kapila et al., reviewed series of four cases of papillary cystadenocarcinomas of the parotid glands, the diagnostic accuracy in an adequate and properly prepared Fine Needle Aspiration Cytology (FNAC) material was 80–95% [8]. Papillary cystadenocarcinomas of the parotid are rare but can be accurately diagnosed on FNAC. In our case, FNAC was not done.
These tumours need to be differentiated from cystadenoma that depends on identification of infiltrative growth into adjacent salivary parenchyma or surrounding tissues. Cystadenocarcinomas can have mild to moderate nuclear atypia with one or two small distinct hyperchromatic nucleoli and eosinophilc to vacuolated cytoplasm [4]. In the present case, there was infiltration of cystic and solid epithelium of cystadenocarcinoma into the fibrotic stroma. The other differential diagnosis of which included polymorphous low grade adenocarcinoma, papillary cystic variant of acinic cell carcinoma, adenoid cystic carcinoma, salivary duct carcinomas and metastatic papillary carcinoma [9]. Polymorphous low grade adenocarcinoma occurs almost exclusively in minor glands; infiltrates as islands, cords, tubules and linearly arranged concentric whirling fascicles of tumour cells expressing cytokeratin(CK), Epithelial Membrane Antigen (EMA), S-100 and haphazard distribution of p63; myoepithelial markers are negative. Papillary cystic variant of acinic cell carcinoma is often accompanied by a microcystic growth pattern, a feature not expected in cystadenocarcinoma. The neoplastic acinic cells show positivity for DOG-1(Discovered on GIST-1), CK and carcinoembryonic antigen (CEA). Compared with cystadenocarcinoma, salivary duct carcinoma usually has large pleomorphic nuclei, ample eosinophilic cytoplasm and express androgen receptor, HER2 and Gross Cystic Disease Fluid Protein 15 (GCDFP-15). The metastatic papillary thyroid carcinoma reveals characteristic nuclear features and express thyroid transcription factor 1 (TTF-1) [9,10].
Conservative but complete surgical excision (superficial parotidectomy) is the treatment of choice [11]. In a study of 40 patients with follow-up data, all were alive or had died of other causes, four suffered metastasis to regional lymph nodes, one at the time of diagnosis and one after 55 months and three experienced a recurrence at a mean interval of 76 months [4].
Conclusion
Papillary cystadenocarcinoma is a slow growing, asymptomatic, rare malignant tumour of the parotid gland. Histologic confirmation of stromal invasion is required to differentiate it from its benign counterpart cystadenoma. Conservative wide local surgical excision is the treatment of choice.
[1]. Auclair PL, Cystadenocarcinoma. In: Barnes L, Eveson JW, Reichart P, Sidransky D, editors. World Health Organization classification of tumoursPathology and genetics of head and neck tumours 2005 LyonIARC Press:232-33. [Google Scholar]
[2]. Ellis GL, Auclair PL, Atlas of tumour pathology series 4: Tumour of the salivary glands 2008 Washington, DCArmed Forces Institute of Pathology:281-89. [Google Scholar]
[3]. Nakagawa T, Hattori K, Iwata N, Tsujimura T, Papillary cystadenocarcinoma arising from minor salivary glands in the anterior portion of the tongue: A case reportAuris Nasus Larynx 2002 29:87-90. [Google Scholar]
[4]. Foss RD, Ellis GL, Auclair PL, Salivary gland cystadenocarcinomas. A clinicopathologic study of 57 casesAm J Surg Pathol 1996 20(12):1440-47. [Google Scholar]
[5]. Pollett A, Perez-Ordonez B, Jordan RC, Davidson MJ, High-grade papillary cystadenocarcinoma of the tongueHistopathology 1997 31(2):185-88. [Google Scholar]
[6]. Ellis GL, Auclair PL, Tumours of the salivary glandsAtlas of tumour pathology 1996 3rd seriesWashington, DCArmed Forces Institute of Pathology:289-96. [Google Scholar]
[7]. Koc M, Yanilmaz M, Yildirim H, Gök U, Cobanoglu B, MRI findings of papillary cystadenocarcinoma of the submandibular glandDiagn Interv Radiol 2010 16(1):20-23. [Google Scholar]
[8]. Kapila K, Verma K, Cytomorphologic features of papillary cystadenocarcinoma of the parotidDiagn Cytopathol 2002 26(6):392-97. [Google Scholar]
[9]. Wanjari SP, Wanjari PV, Patidar KA, Parwani RN, Papillary cystadenocarcinoma of the hard palateBMJ Case Rep 2014 2014:1-5. [Google Scholar]
[10]. Chan JKC, Cheuk W, Tumours of the salivary glands. In: Christopher D.M. Fletcher, editorDiagnostic histopathology of tumours 2013 4th editionSaunders, Elsevier Limited:270-377. [Google Scholar]
[11]. Aloudah NM, Raddaoui E, Aldhahri S, Al-Abbadi MA, Low-grade papillary cystadenocarcinoma of the parotid gland: presentation of a case with cytological, histopathological, and immunohistochemical features and pertinent literature reviewDiagn Cytopathol 2009 37(2):128-31. [Google Scholar]