Sleep is referred a regular, recurring and easily revocable state of organism which is characterized by relative immobility and significant increase in response threshold to environmental stimuli compared to waking state. Sleep is a basic need of human and takes approximately 1/3rd of one’s lifetime [1].
Sleep disorder is a condition characterized by disturbed sleep-related pattern or behaviours [2]. The prevalence of sleep-related problems and disorders is high in patients with end-stage renal disease (ESRD), particularly sleep apnea, restless legs syndrome, and overall poor sleep quality [3]. Chronic disease affects quality of life [4–9]. Studies on sleep disorders effect on quality of life in haemodialysis patients have demonstrated the significant contribution of these disorders to the quality of life [10]. Some studies have reported a direct association between increased mortality and poor sleep quality [11]. ESRD is known to have a negative effect on energy and vitality levels, sometimes reducing or limiting social interactions and affecting mental health. Both poor sleep and depression in haemodialysis patients have been associated with reduced quality of life and increased mortality risk [12]. Using non-pharmacological interventional therapies such as behavioural approaches, sleep restriction therapy, stimulus control, adherence to sleep hygiene behaviours, relaxation techniques, biofeedback, guided imagery, and cognitive approaches, we may overcome many prevalent sleep disorders. “Sleep hygiene” refers to those behaviours that are believed to promote improved quantity and quality of sleep [13].
The term “sleep hygiene” was used by Peter Hauri in 1977 in the context of providing recommendations for patients to help them improve their insomnia [14]. Studies have demonstrated that people with poor sleep health have a considerably higher proportion of sleep disorders. Therefore, the rate of sleep disorders can increase in haemodialysis patients. In Brick et al., study on the association between sleep hygiene and sleep quality in medical students, low sleep quality was largely associated with poor health [15]. Brown et al., also in a study on the association between knowledge about sleep hygiene and sleep quality in university students found similar results [16]. Brown et al., study indicated that variable sleep schedules, going to bed thirsty, environmental noise, and worrying while falling asleep contributed to poor sleep quality [16]. Jefferson et al., also have reported consistent findings, as well [14].
Kakinuma et al., studied to investigate the effect of sleep hygiene education on insomnia in information technology workers reported this approach to be partially effective as it led to decline in daily napping in the participants [17]. Furthermore, Nishinoue et al., investigationed of the effect of sleep hygiene education and behavioural therapy in information technology workers found this education to be an effective approach to decrease the scores for Pittsburgh Sleep Quality Index (PSQI). However, the effect of sleep hygiene education combined with behavioural therapy was more effective [18].
Taken together, sleep disorders are highly prevalent in haemodialysis patients, intensifying their individual and social problems to some extent [19]. Despite many investigations on the prevalence of sleep disorders in haemodialysis patients and the associated factors, interventional approaches to improve sleep quality in haemodialysis patients have been explored much less frequently. In this study, we seek to take a step to improving sleep quality in haemodialysis patients through face-to-face sleep health education.
Materials and Methods
In this controlled, randomized clinical trial, the participants were haemodialysis patients admitted to the Dialysis Ward of Shahid Ayatollah Madani Hospital, Khoy. The inclusion criteria were having medical file in the haemodialysis ward of the hospital under study, being consent to participate in the study and at least 18 years, having at least six-month history of haemodialysis, full consciousness and adequate auditory and verbal ability to respond to questions.
The exclusion criteria were history of confirmed psychiatric disorder, alcoholism, physical and mental retardation and drug addiction. Participation in this study was voluntary and the informed consent was provided by the participants after research purposes and procedure were explained to them. According to the sample size formula, 65 patients were enrolled from 130 patients admitted to the haemodialysis ward under study by random sampling [20]. Sampling was conducted at morning, evening, and night shifts but the patients at night shifts were not enrolled [Table/Fig-1].
Flowchart of participants allocation and outcome assessment.
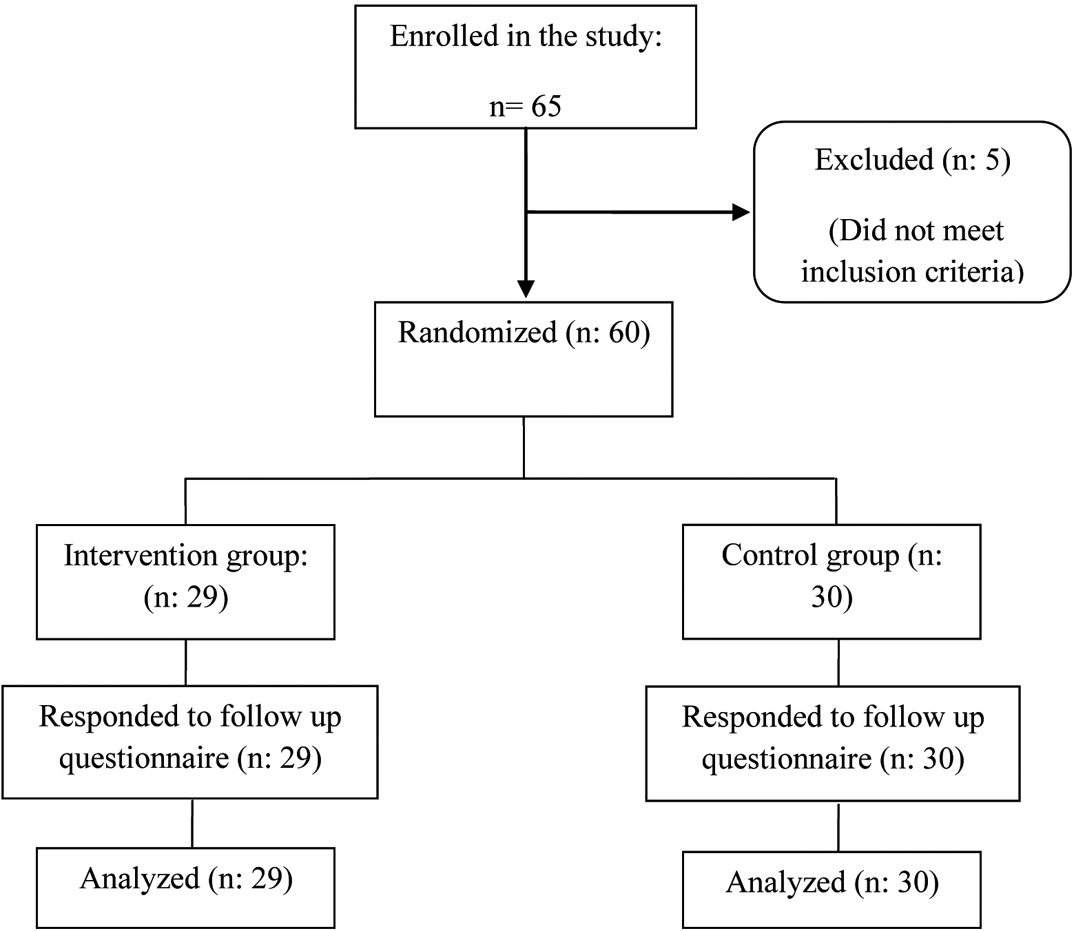
Of the enrolled patients, two were excluded because of Alzheimer’s disease, two were excluded because of changing the dialysis time to the night shift, and one was excluded because of auditory disorder. After sampling was completed, the patients were assigned to two groups, one intervention and one case, of 30 each and in the intervention group, one patient was excluded because of declining to continue participation. The participants were assessed individually through questionnaire interviewing before the intervention. In the intervention group, 53.3% were male and in the control group, 56.7% were male.
The instrument of data gathering was a questionnaire administered during dialysis and recovery of overall conditions of the patients. If a patient was literate, he/she was given the questionnaire to fill out and if the patient was illiterate, the questions were asked and his/her responses were ticked by the interviewer. To examine the sleep quality, Persian version of PSQI was used [19]. PSQI was developed to provide a reliable, valid and standardized measure of sleep quality; to discriminate between “good” and “poor” sleepers; to provide an index that is easy for subjects to use and for clinicians and researchers to interpret; and to provide a brief, clinically useful assessment of a variety of sleep disturbances that might affect sleep quality [20].
PSQI is a standard scale which is widely used for both clinical studies and general health investigations [21]. PSQI consists of seven domains to explore both quantity and the quality of sleep for the last month. These domains are sleep quality, sleep latency, sleep duration, habitual sleep efficiency, and sleep disorders, use of sleep medications, daily sleep disturbance, daily sleep duration. The PSQI score ranges 0-21 and higher scores represent poorer sleep quality. The scores five and higher indicate that one has difficulty in sleeping [22]. This questionnaire has been frequently used to assess sleep quality and to diagnose sleep disorders and therefore its validity, reliability and sensitivity have been explored in several studies in Iran and worldwide (χ2=89.6 and correlation coefficient=0.88) [23]. To determine validity, the Persian version of PSQI and the research purposes were offered to 10 faculty members and the necessary corrections were made. The psychometric characteristics of this scale have already been confirmed for Iranian population [24].
The demographic data of all the patients were gathered by a questionnaire [25]. After the written approval of the Urmia University of Medical Sciences was provided, the researcher referred to the hospital under study, offered a letter of introduction and obtained the consent of the hospital officials to conduct the study. Then, he referred to the haemodialysis ward of the hospital and identified the haemodialysis patients with the inclusion criteria after introducing himself and explaining the research purposes. After the informed consent was provided by the patients, the researcher asked them to fill out the demographic characteristics questionnaire and the PSQI.
Sleep health education protocol was developed by the researcher and supervisor with reference to reliable references [13,26–28]. This protocol consisted of two sections and was taught within an hour. The first section taught in the first session addressed the sleep process and significance and its effect on daily activities, and the importance of sleep environment. The materials were offered to the participants face-to-face within half an hour.
The second section was offered face-to-face within 20 minutes in the second session and addressed sleep health-related behaviours [Table/Fig-2]. After the second session, within 10 minutes, the participants were allowed to ask their questions and the taught materials were assessed by the researcher.
Contents of sleep hygiene group education.
Sleep Hygiene EducationGet up every day at the same time, including weekends. Avoid taking daytime naps. Avoid the use of caffeinated products, nicotine, and alcohol, especially later in the day. Avoid heavy meals within two hours before going to sleep. Maintain appropriate environmental conditions for sleep. Avoid stressful activities within a few hours before going to sleep (i.e. avoid noisy environments). Pursue regular physical activity, such as walking or gardening, but avoid vigorous exercise within a few hours before going to sleep. Take a bath in body temperature water to relax. Avoid any activities (watching TV, etc.) except sleeping in bedroom. Sexual activity causes no problem.
|
Statistical Analysis
For data analysis, SPSS 16 was used. To investigate the demographic variables in the two groups, chi-square was used and to examine the effect of sleep health education on the scores of sleep quality and its domains, paired t-test (for normally distributed data) and Wilcoxon’s test (for non-normally distributed data) were used. To explore the co-rrelation between total score of sleep quality and sociodemographic characteristics, Pearson’s correlation coefficient (continuous variables), Spearman’s correlation coefficient (ordinal variables), and independent t-test were used.
Results
Five of 65 patients were excluded from the study and 60 patients were randomly assigned to two groups intervention and control group of 30 each. One patient was excluded because of declining to continue participation. Chi-square and t-test indicated no significant difference in age, gender, dialysis duration, education, the amount of caffeine used per day and smoking between the two groups.
Education level and body mass index were not significantly correlated with PSQI score before and after the intervention, but age and PSQI score were significantly correlated after the intervention such that the younger patients had a higher sleep quality [Table/Fig-3].
Correlation of body mass index, age, gender, and education with Pittsburgh Sleep Quality Index score before and after the intervention in case and control groups.
| Groups/Variables | PSQI of Intervention Group | PSQI of Control Group |
|---|
| Before intervention | After intervention | Before intervention | After intervention |
|---|
| BMI | p=0.017 | p=0.397 | p=0.144 | p=0.346 |
| r=0.433 | r=0.163 | r=0.273 | r=0.178 |
| Age | p=0.285 | p=0.001 | p=0.247 | p=0.311 |
| r=0.901 | r=0.600 | r=0.302 | r=0.192 |
| Education | p=0.607 | p=0.084 | p=0.136 | p=0.209 |
| r=0.098 | r=0.327 | r=0.279 | r=0.236 |
[Table/Fig-4] indicates the comparison of total score for PSQI (by t-test) and domain scores of PSQI (by Wilcoxon’s test) between before and after the intervention in the two groups. In the intervention group, the total and all domain scores of PSQI, except taking sleep medications, decreased but in the control group, neither total score nor domain scores decreased. A significant difference in the mean score for PSQI was detected before and after the intervention (p<0.001) [Table/Fig-4]. Despite the high score for PSQI in the intervention group compared to the control before training, a significant decrease was seen in the mean score of PSQI in this group with no significant difference (p=0.704). Even, a minor increase in the PSQI score was detected compared to before the intervention.
Comparison of domain and total scores of Pittsburgh Sleep Quality Index in intervention and control groups between before and after intervention.
| Domains of PSQI | Intervention group | p-value | Control group | p-value |
|---|
| Before intervention | After intervention | Before intervention | After intervention |
|---|
| Mean (±SD) | Mean (±SD) | Mean (±SD) | Mean (±SD) |
|---|
| Subjective sleep quality | 2.00 (0.91) | 1.03 (1.05) | 0.0009 | 1.20 (0.96) | 1.73 (1.99) | 0.096 |
| Sleep latency | 2.33 (0.92) | 1.07 (0.92) | 0.0009 | 1.67 (0.99) | 1.47 (0.81) | 0.237 |
| Sleep duration | 2.13 (1.07) | 1.28 (1.03) | 0.002 | 1.33 (1.06) | 1.47 (1.00) | 0.429 |
| Sleep efficiency | 2.13 (1.25) | 1.21 (1.17) | 0.008 | 1.30 (1.34) | 1.30 (1.29) | 0.903 |
| Sleep disturbance | 1.37 (0.49) | 0.97(0.32) | 0.002 | 1.33 (0.547) | 1.33 (0.547) | 1.00 |
| Use of sleep medication | 0.5 (1.13) | 0.28 (0.84) | 0.180 | 0.77 (1.27) | 0.73 (1.25) | 0.705 |
| Daytime dysfunction | 1.70 (1.088) | 1.10(0.939) | 0.002 | 1.73 (1.01) | 1.77 (0.89) | 0.827 |
| Global PSQI Score | 12.7 (4.434) | 7.03 (4.355) | 0.0009 | 9.33 (4.686) | 9.57 (4.584) | 0.704 |
Discussion
Some researchers have argued for sleep hygiene education as the first-line treatment for sleep disorders [29]. Increased demand for sleep of higher quality is a global concern, which is more urgent for haemodialysis patients. Despite the fact that education contributes positively to changing behaviour, the inefficiency of sleep hygiene education as a treatment for sleep disorders has been largely investigated in the studies on sleep [30,31]. Some of the studies have reported sleep hygiene education to contribute only to insomnia. Many of the non-pharmacological therapies including cognitive therapy and behavioural therapy require special conditions such as the availability of specialized staff, which makes their administration limited to some patients [32].
To the best of our knowledge, no study has yet been conducted to investigate sleep hygiene education in haemodialysis patients in Iran. This study indicated that the quality of life improved after the training intervention. The post-hoc analysis indicated significant differences in the scores for PSQI and its domains between the intervention and control groups, indicating the effect of sleep hygiene education on improvement of sleep quality and its domains in haemodialysis patients. This is in agreement with the studies confirming the contribution of sleep hygiene education to sleep quality [17,18].
According to this study, 84.7% of the patients had low sleep quality, which is consistent with Babahaji et al., and Menon et al., studies reporting the prevalence of sleep disorders in these patients to be 64.5% and 67%, respectively [33,34].
In the present study, majority of the patients complained of having difficulty falling asleep, shorter sleep duration, and less efficient sleep. Few patients also reported significant day time dysfunction.
In the present study, sleep hygiene education caused a significant improvement of sleep quality at all domains except taking sleep medications, which is consistent with the works reporting no significant change in the rate of sleep medications taking after sleep hygiene education. This finding may be explained by the fact that to discontinue their sleep medications, the patient needed time and confidence in satisfactory efficiency of the training given. Another explanation is that the number of the participants that took sleep medications was too small to expect a significant result.
The mean total score of sleep quality after sleep hygiene education was over five that represented a poor sleep quality. Although sleep hygiene education caused improvement of sleep quality in the patients but it failed to increase the mean sleep quality to a normal level. This finding may be explained by severe sleep disorders in the patients. Rigney et al., study was the first randomized controlled trial to investigate the effectiveness of a sleep education program on both objective and subjective sleep behaviour of middle-school children. The results showed that the intervention group increased their time in bed through delaying their wake time by 10 minute immediately after receiving the sleep education program [35]. Prince et al., conducted a study on the same target population. Their findings showed that sleep quality significantly improved in the experimental group only [36]. Kakinuma et al., studied the effect of sleep hygiene education on insomnia in 581 information technology workers and found that this education was partially effective because of leading to decrease in napping [17].
Nishinoue et al., explored the effect of sleep hygiene education and behavioural therapy on sleep quality in information technology workers. In that study, one group received sleep hygiene education alone and another group sleep hygiene education alongside behavioural therapy. The hygiene education caused PSQI score to decline in the participants. However, the effect of education alongside behavioural therapy was higher [18].
To determine the effective factors on sleep quality in the patients, the correlation between any demographic characteristics and sleep quality total score was investigated before and after the training intervention. Among the demographic characteristics, young age was significantly associated with high sleep quality after training because younger patients were more likely to cooperate better with the researcher for practicing the taught materials and more willing to improve their sleep quality [37].
Limitation
Small sample size enrolled in this study limits the generalization of the study findings.
Conclusion
Sleep hygiene education, alongside other approaches, is a low-cost, accessible, and practical method which can be implemented within a short period of time. Treatment brings stupendous costs for many of the haemodialysis patients and hence they may fail to afford improvement of quality of their sleep. Sleep hygiene can be trained to patients during haemodialysis within a short time by nurses in haemodialysis wards.
Funding/Support
This study was funded by the Research and Technology Deputy of Shahid Beheshti University of Medical Sciences, Tehran, Iran.