Early Post-Operative Coronary Thrombosis Following Repair of a Proximal Coronary Artery Fistula
Yashasvi Chugh1, Bryan Lau2, Cynthia C Taub3
1 Resident, Department of Internal Medicine, Jacobi Medical Center/Albert Einstein College of Medicine, Bronx, New York, USA.
2 Resident, Department of Internal Medicine, Harbor UCLA Medical Center, Torrance, California, USA.
3 Director, Non-invasive Cardiology, Montefiore/Einstein, Professor of Clinical Medicine, Albert Einstein College of Medicine, Bronx, New York, USA.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Yashasvi Chugh, Resident, Department of Internal Medicine, Jacobi Medical Center/Albert Einstein College of Medicine, Bronx, New York-10461, USA.
E-mail: yashasvichugh@hotmail.com
Patients with aneurysmal coronary artery fistulas are often a treatment challenge. We hereby, report a case of aneurysmal left main coronary artery to coronary sinus fistula repair, complicated by an early post-operative thrombosis of the left main coronary artery, necessitating an orthotropic heart transplant. Routine use of peri-procedural and long-term anti-coagulation is usually not a standard recommendation in these cases; however, early institution of the same may prevent flow stasis, thrombus formation and unfavourable outcomes pre- or post-operatively.
Coronary artery aneurysm, Heart transplant, Thrombus formation
Case Report
A 59-year-old female with a known congenital Left Main Coronary Artery (LMCA) to Coronary Sinus (CS) fistula, presented with worsening dyspnoea. The patient refused to consider any intervention previously. Physical examination revealed a continuous murmur over the precordium and evidence of volume overload.
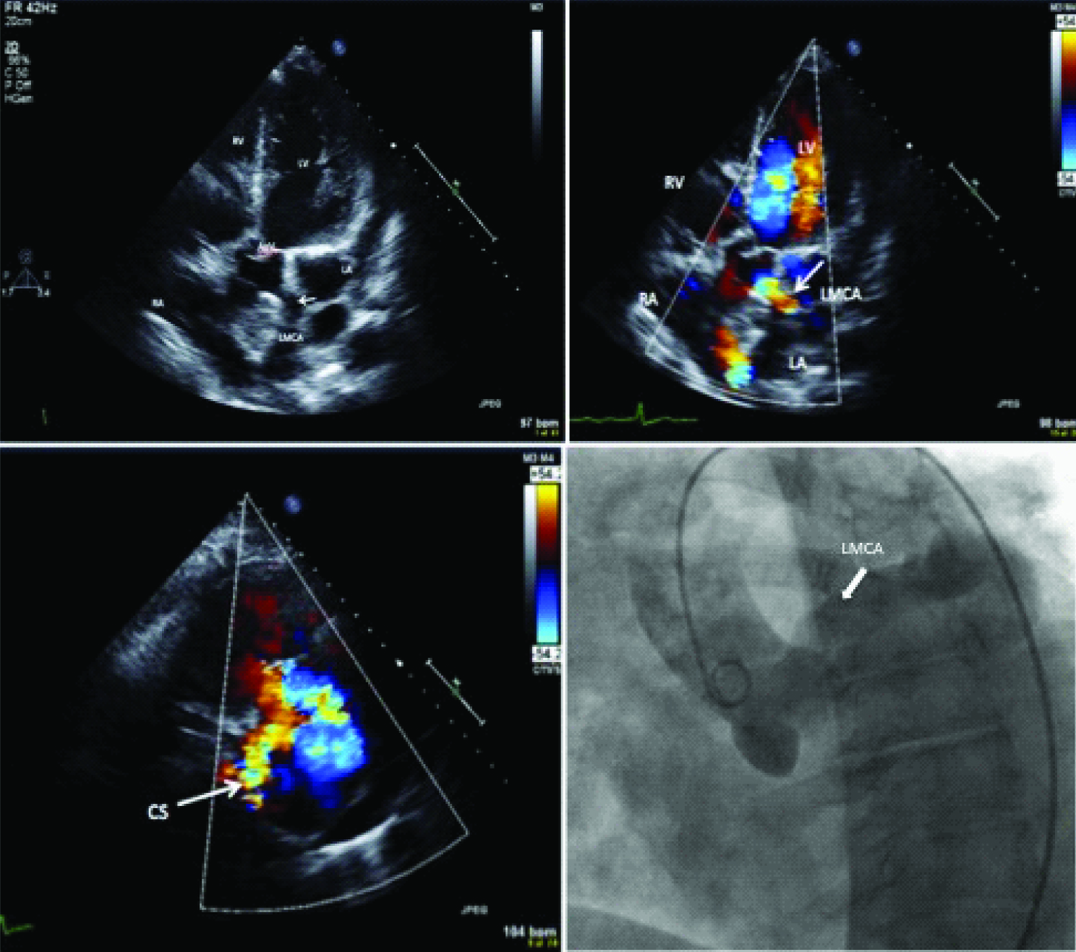
Further evaluation with a Transthoracic Echocardiogram (TTE) revealed dilated cardiac chambers, a Left Ventricular Ejection Fraction (LVEF) of 35% which was 60% two years ago, dilated CS and proximal LMCA, with evidence of left to right shunting between them [Table/Fig-1a-c]. Subsequent coronary angiogram showed a dilated LMCA [Table/Fig-1d]. A right heart catheterisation revealed a step-up in oxygen saturation in the right atrium (Qp/Qs 1.8).
Clock wise from the upper left: (a) Transthoracic echocardiogram in the apical 5-chamber view showing dilated chambers and severely dilated left main coronary artery ostium (arrow); (b) Color flow doppler revealing increased flow across the ostium (arrow); (c) Coronary sinus (arrow); (d) Aortogram of dilated proximal left coronary artery (arrow).
RA-right atrium, LA-left atrium, LV-left ventricle, RV-right ventricle, LMCA-left main coronary artery, CS-coronary sinus, AoV-aortic valve
The patient underwent a surgical ligation of the fistula at its origin close to the LMCA. She was stable immediately post-operatively; however, on post-operative day 1, she developed cardiogenic shock (EF 15%); an urgent coronary angiogram revealed complete thrombosis of the LMCA, necessitating emergent coronary artery bypass grafting. Subsequently, she required support with Extra-Corporeal Membrane Oxygenation (ECMO). On post-operative day 7, she failed ECMO clamping and underwent left ventricular assist device implantation. In the following months her clinical course was complicated by repeated heart failure re-hospitalization. She eventually underwent successful orthotopic heart transplantation.
Discussion
Coronary Artery Fistulas (CAF) are abnormal connections between coronary arteries and a cardiac chamber or major vessel [1–3]. They are the second most common congenital coronary anomaly, with an incidence of 0.2% to 0.6% in patients undergoing coronary angiograms [4]. Guidelines for management of adults with congenital heart disease [4] recommend closure of all large CAFs or symptomatic CAFs irrespective of their size [5]. Large fistulas (>three times the normal proximal coronary artery diameter) or shunts (Qp/Qs >1.5) are haemodynamically significant and often symptomatic [1,4].
Coronary steal often leads to myocardial ischaemia, which in turn causes compensatory dilation of the native coronary artery with possible aneurysmal formation [1].
Surgical closure is preferred for CAFs with the following characteristics: i) locations out of reach for percutaneous intervention; ii) multiple fistulas; iii) extreme native vessel tortuosity; (iv) aneurysmal dilation of fistula or proximal coronary artery; iv) presence of normal coronary branches near the fistula’s drainage sites [1].
Transcatheter closure alternatively is considered the procedure of choice, given its shorter recovery time for patients; however, it is limited to smaller and anatomically simpler fistulas [1].
Several studies have reported early and late symptomatic coronary thrombosis after surgical and percutaneous repair of CAF in adults [Table/Fig-2] [5–10]. Distal CAFs [8–10] often are at greater risk of flow stasis and thrombosis following closure, due to greater proximal coronary artery dilation [1]. Whereas, proximally located fistulas, such as in our case, may have formed a blind pouch between the ligated portion of the fistula and the native coronary artery following fistula ligation, leading to thrombus propagation [5–7].
Summary of studies reporting adverse coronary events after proximal or distal coronary fistula closure.
| Reported Case (reference) | Age at Diagnosis (years), Sex | Origin, Termination of CAF | Location and Size of CAF | Associated Coronary Artery Dilation | Treatment Pathway | Timing of Thrombosis | Coronary Anatomy | Outcome | Mortality |
|---|
| Mesko ZG et al., [5] | 4, Female | LMCA, RA | Proximal, Large | - | Surgical | Late (11 years) | LAD and D-1 bifurcation with thrombus | Normal LV function and Coronary Flow | Nil |
| Toyoda Y et al., [6] | 10, Female | RCA, RA | Proximal, Large | - | Surgical | Late (day 9) | Thrombus in dilated proximal segment | Normal LV function | Nil |
| Goldberg SL et al., [7] | 37, Male | LCX, CS and RCA, CS | Proximal, Large and Distal, Small | LMCA, LCX | Surgical | Late (1.5 years) | Occluded proximal LCX | LCX thrombosis with stent placement (1.5 years), OM occlusion requiring CABG (2 years) | Nil |
| Ascoop AK et al., [8] | 69, Female | RCA/RCC, RA | Distal, Large | Proximal RCA | Percutaneous closure, Amplatzer VSD occluder | Early (few hours) | Thrombus in blind pouch of fistula/proximal RCA | Hemodynamic Collapse, CABG | Nil |
| Kharouf R et al., [9] | 48, Female | LCX, CS | Distal, Large | LMCA, LCX | P, Coil Embolisation | Late (4 days) | Thrombsis of complete LCX | LV posterio-inferior wall hypokinesis, Intermittent Atrial fibrillation, Pulmonary Embloism | Nil |
| Hamada M et al., [10] | 26, Male | LAD, RV | Distal, Large | LAD | Surgical | Late (9 months) | Thrombsis of LAD | - | Nil |
| Current Case | 59, Female | LMCA, CS | Proximal, Large | RCA, LCA | Surgical | Early (1 day) | Thrombsis of complete LCA | Cardiogenic Shock, LVAD, OHT | Nil |
*LMCA (left main coronary artery), RA (right atrium), RCA (right coronary artery), RCC (right coronary cusp), S (surgical closure), P (percutaneous closure), LV (Left Ventricle), LCX (left circumflex artery), D-1 (First Diagonal artery from left anterior descending artery), LCA (Left Coronary Artery), LVAD (Left Ventricular Assist Device), OHT (Orthotopic Heart Transplant), OM (obtuse marginal), CABG (coronary artery bypass grafting).
Fistulas found draining into the coronary sinus tend to have poorer outcomes compared to those draining into the right ventricle, pulmonary arteries or left ventricle [1,11]. It is believed that, following surgical repair there is risk of extension of a thrombus from the dilated coronary sinus into the major epicardial artery [11].
Further, patients who have delayed coronary thrombosis may have better outcomes, compared to those with early thrombosis, as their opposing coronary system can slowly adapt by increasing collateralization [12].
In our case, the patient had a congenital proximal LMCA fistula that led to significant coronary dilation with risk of stasis of blood flow when the shunt was closed.
Conclusion
Consensus on preventing such thrombi is lacking. The decision to start anti-platelet/anti-coagulation therapy in patients following CAF repairs may be determined by the size of the fistula, presence of residual aneurysms and by balancing the patient’s risk of bleeding with thrombosis.
*LMCA (left main coronary artery), RA (right atrium), RCA (right coronary artery), RCC (right coronary cusp), S (surgical closure), P (percutaneous closure), LV (Left Ventricle), LCX (left circumflex artery), D-1 (First Diagonal artery from left anterior descending artery), LCA (Left Coronary Artery), LVAD (Left Ventricular Assist Device), OHT (Orthotopic Heart Transplant), OM (obtuse marginal), CABG (coronary artery bypass grafting).
[1]. Laston LA, Coronary artery fistulas: How to manage themCatheter Cardiovasc Interv 2007 70:110-16. [Google Scholar]
[2]. Buccheri D, Luparelli M, Chirco PR, Piraino D, Andolina G, Assennato P, A call to action for an underestimated entity: Our algorithm for diagnosis and management of coronary artery fistulaInt J Cardiol 2016 221:1081-83. [Google Scholar]
[3]. Gowda ST, Forbes TJ, Singh H, Kovach JA, Prieto L, Latson LA, Remodeling and thrombosis following closure of coronary artery fistula with review of management: Large distal coronary artery fistula-to close or not to close?Catheter Cardiovasc Interv 2013 82:132-42. [Google Scholar]
[4]. Warnes CA, Williams RG, Bashore TM, Child JS, Connolly HM, Dearani JA, ACC/AHA 2008 guidelines for the management of adults with congenital heart disease: A report of the American College of Cardiology/American Heart Association Task Force on Practice GuidelinesJ Am Coll Cardiol 2008 52:e1-121. [Google Scholar]
[5]. Mesko ZG, Damus PS, Myocardial infarction in a 14-year-old girl, ten years after surgical correction of congenital coronary artery fistulaPediatr Cardio 1998 19:366-68. [Google Scholar]
[6]. Toyoda Y, Yamaguchi M, Ohsima Y, Yoshimura N, Tanaka T, Oka S, A surgical case of right coronary artery-right atrial fistula complicated with post- operative myocardial infarctionKyobu Geka 1999 52:326-31. [Google Scholar]
[7]. Goldberg SL, Manchester J, Laks H, Late-term myocardial infarction after surgical ligation of a giant coronary artery fistulaJ Invase Cardiol 2002 14(4):202-06. [Google Scholar]
[8]. Ascoop AK, Budts W, Percutaneous closure of a congenital coronary artery fistula complicated by an acute myocardial infarctionActa Cardiol 2004 59:67-69. [Google Scholar]
[9]. Kharouf R, Cao QL, Hijazi ZM, Transcatheter closure of coronary artery fistula complicated by myocardial infarctionJ Invasive Cardiol 2007 19(suppl):E146-49. [Google Scholar]
[10]. Hamada M, Kubo H, Matsuoka H, Kokubu T, Oosuga Y, Joh T, Myocardial infarction complicating surgical repair of left coronary– right ventricular fistula in an adultAm J Cardiol 1986 57:372-74. [Google Scholar]
[11]. Valente AM, Lock JE, Gauvreau K, Rodriguez-Huertas E, Joyce C, Armsby L, Predictors of long-term adverse outcomes in patients with congenital coronary artery fistulaeCirc Cardiovasc Interv 2010 3:134-39. [Google Scholar]
[12]. Cheung DL, Au WK, Cheung HH, Chiu CS, Lee WT, Coronary artery fistulas: Long-term results of surgical correctionAnn Thorac Surg 2001 71:190-95. [Google Scholar]