Irritable Bowel Syndrome (IBS) is a Gastrointestinal (GI) disorder characterized by altered bowel habits and abdominal pain in the absence of detectable structural abnormalities. It is one of the most common disorders encountered by general practitioners (15-20%) as well as by gastroenterologists (around 50%) [1]. IBS is associated with a wide variety of GI symptoms like functional dyspepsia and Gastro-Esophageal Reflux Disease (GERD) [2], and extra-intestinal symptoms like urinary complaints, sexual dysfunction, bronchial hyper-responsiveness and asthma [3]. Asthma is a chronic inflammatory disease of the airways, characterized by increased responsiveness of the tracheobronchial tree to a variety of stimuli. It manifests as episodes of widespread reversible narrowing of airway leading to clinical symptoms of dyspnea, cough and wheezing. The prevalence of chronic functional bowel disorders in India is 10 to 20%, with IBS constituting 4.2% [4]. Approximately 20 to 30% of Indian population is affected by one or more of the allergic diseases like allergic rhinitis, asthma, rhinitis, anaphylaxis, drug, food and insect allergy, eczema, urticaria and angioedema [5].
The pathophysiology of IBS is still not well understood. Several studies have reported association between IBS and broncho-pulmonary diseases [3,6–9]; however, other studies have not confirmed this association [10,11]. It has been shown that, asthmatics have increased prevalence [12,13] and risks [14,15] for developing IBS. Patients with IBS have also been reported to have increased airway resistance when compared to healthy subjects [16]. The presence of generalized smooth muscle or autonomic nervous system dysfunction involving abnormal visceral sensitivity and neurotransmitter imbalance has been proposed [17,18]. Despite the increasing incidence of IBS in India, there continues to be paucity of literature on IBS in this region. The dietary habits such as fiber intake, allergy disorders and health seeking behaviour of this region are different from the western cohort. The aim of our study was to assess the prevalence of asthma in IBS, in a cohort of Indian patients.
Materials and Methods
This study was performed at the Gastroenterology Department of a tertiary medical center in India. The study was approved by the local ethics committee and informed consent was obtained from all the patients. All adult patients who presented to the gastroenterology clinic for a period of two months in November and December 2008 with symptoms of chronic lower GI complaints were included in the study. The diagnosis of IBS was made by a questionnaire based on Rome III criteria [19].
The ROME III criterion for IBS diagnosis is the presence of recurrent abdominal discomfort (or pain) for three or more days every month which must be present in the last three months with its onset at least six months before the time of diagnosis. They must also be associated with at least any two of the three complaints:
1) Improvement of discomfort (or pain) with defecation
2) Change in frequency of stool
3) Change in form (appearance) of stool with onset.
Patients who had symptoms atypical of IBS like pain that awakens or interferes with sleep, diarrhoea that awakens or interferes with sleep, blood in the stool (visible or occult), weight loss, fever or presence of any abnormal physical examination findings were excluded from the study. Patients who were smokers, more than 60 years of age or with history of recent respiratory tract infection that would affect the outcome of spirometry were also excluded from the study. The control group constituted of the healthy family members of the IBS patients.
The IBS patients were questioned for GI symptoms:
i) pain relieved with defecation
ii) stool consistency (hard, normal or soft); iii) sensation of incomplete evacuation
iv) passage of mucus with stools, constipation/diarrhoea alternation v) feeling of distension of abdomen and vi) frequency of stool.
For this study, increased stool frequency was described as more than three times per day while normal was defined as symptoms more than once every three days to less than three times per day and decreased frequency was defined as symptoms fewer than once every three days.
The patients also underwent a respiratory system evaluation with questions for respiratory symptoms:
i) cough
ii) dyspnoea
iii) asthma attacks in past
iv) waking in night with shortness of breath or coughing
v) report of having taken treatment for asthma and
vi) previous diagnosis of asthma or any family history of asthma.
Spirometry was then performed by a single clinician using ‘SPIROWEB’ machine (manufactured by drcdrecare, Hyderabad, India) with the patient in sitting position. Multiple attempts were made to familiarize the patient with the procedure in order to obtain the accurate result. The Forced Vital Capacity (FVC), Forced Expiratory Volume in first second (FEV1), FEV1/FVC were recorded. Patients with FEV1 less than 75% of the predicted value were given two actuations (200μg) of Salbutamol from a metered dose inhaler and spirometry was repeated after 15 minutes. An increase in more than 15% of FEV1 was considered as positive reversible bronchoconstriction, which was interpreted in this study as positive criterion for bronchial asthma.
Statistical Analysis
Statistical analysis was done in STATA version 12 (Stata Corp LP, TX, USA). Chi-square test was used for nominal variables while student’s t test was used for continuous variables. The p-value of 0.05 was set as the limit for evidence of statistical significance.
Results
Seventy patients each were included in both the IBS (group I) and control groups (group II). There were 16 women and 54 men in group I, while group II constituted 14 women and 56 men. Mean age of the patients was 33 and 32 years in group I and II respectively.
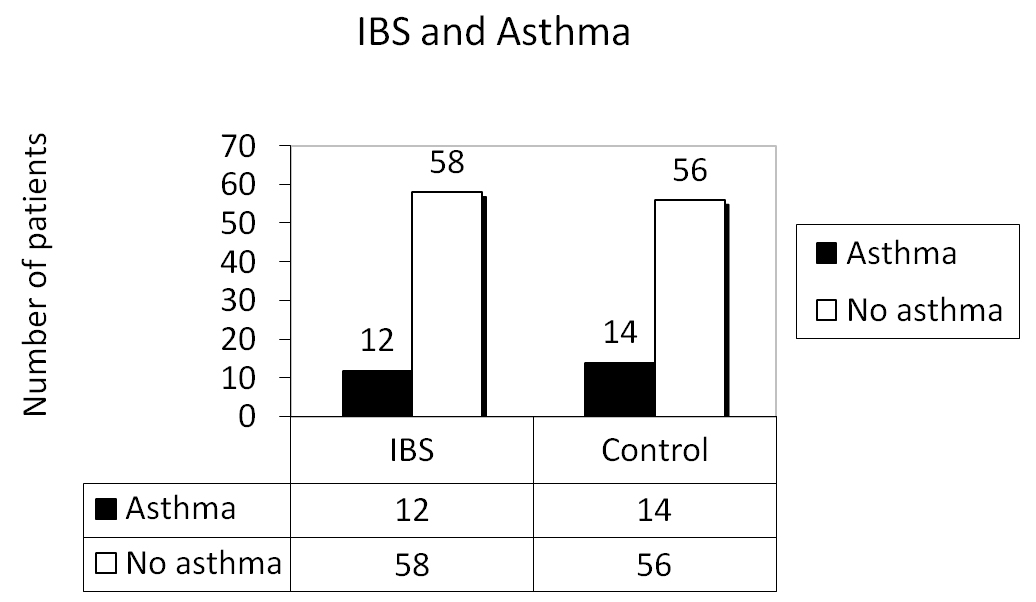
The spectrum of GI and respiratory complains reported by IBS patients are summarized in [Table/Fig-1]. A sensation of incomplete evacuation was the most common complaint followed by soft consistency of stool. Cough, followed by dyspnoea, were the most common respiratory complaint. Eight patients had previous diagnosis of asthma in group I which was confirmed by positive reversible bronchoconstriction with spirometry. The spirometry further diagnosed four more patients with positive reversible bronchoconstriction; thus, increasing the number of asthma patients in group I to 12. Group II had 14 patients with asthma diagnosed by positive reversibility tests. The prevalence of asthma in group I was 17.14% as compared to 20% in group II with Odds Ratio (OR) of 0.828 [Table/Fig-2,3]. Chi-square test yielded a p-value of 0.664 which was not significant for association between IBS and bronchial asthma (p>0.05).
Complaints reported by IBS patients in this study.
| Gastrointestinal Symptoms | n | % |
|---|
| 1. Pain relieved with defecation | 39 | 56 |
| 2. Stool formation | Hard | 34 | 49 |
| Normal | - | - |
| Soft | 42 | 60 |
| 3. Sensation of incomplete evacuation | 57 | 81 |
| 4. Passage of mucus with stools | 24 | 34 |
| 5. Constipation-Diarrhoea alternation | 36 | 51 |
| 6. Feeling of abdominal distension | 38 | 54 |
| 7. Stool frequency | Increased | 31 | 44 |
| Normal | 23 | 33 |
| Decreased | 04 | 06 |
| Respiratory Symptoms |
| 1. Cough | 36 | 51 |
| 2. Dyspnoea | 24 | 34 |
| 3. History of asthma attack | 6 | 9 |
| 4. Waking in night with cough or breathlessness | 12 | 17 |
| 5. Treatment of asthma taken previously | 8 | 11 |
| 6. Previous diagnosis of asthma | 8 | 11 |
| 7. Family history of asthma | 12 | 17 |
Characteristics and asthma prevalence in Irritable Bowel Syndrome (IBS) and control group.
| IBSGroup I | ControlGroup II | OR[95% CI] | p-value(test used) |
|---|
| Age (Mean±SD) | (32.91±10.42) | (32.10±8.92) | | 0.622(t test) |
| Male | 54 | 56 | | 0.680(Chi2 test) |
| Female | 16 | 14 | | 0.680(Chi2 test) |
| Asthman (%) | 12 (17.14) | 14(20.00) | | |
| Total | 70 | 70 | 0.828[0.320 to 2.121] | 0.664(Chi2 test) |
The Odds Ratio (OR) for prevalence of asthma in IBS is 0.828 with 95% Confidence Interval (CI) between 0.320 and 2.121 (p=0.664).
The prevalence (n) of asthma in Irritable Bowel Syndrome (IBS) and control patients.
Discussion
IBS is being recognized more commonly in younger people, which is in consistency with the average age of 33 years in our study. This is also supported by Indian Society of Gastroenterology (ISG) task force report on IBS in India [4]. Our study showed, an increased number of males with IBS as compared to females. This could be attributed to several reasons. Firstly, because of socio-cultural reasons females may not have easy access to healthcare, particularly for minor complains like pain and altered bowel habits. Secondly, the study was done at a tertiary care center and commonly females from rural areas tend to avoid follow-up with referrals to tertiary care centers. Increased prevalence of IBS in males has been reported in prior studies done in India as well [4]. This is in contrast to western countries where IBS is more predominantly reported among females. The most common complaint in our study was the sense of incomplete evacuation, which is consitent with previous reports from this region [4]. IBS patients in our study commonly reported increased bowel movements (more than three times per day) or a normal pattern. The ISG task force on IBS has also identified one to two bowel movements per day as the normal frequency for the Indian population. They have also noted that, the patient’s perception of constipation or diarrhoea in Indian population does not correlate with the physician judgment based on western criteria [4].
Although our study failed to show any significant association between bronchial asthma and IBS in Indian patients, previous studies around the world have shown mixed results. Studies from Italy [10] and South Korea [11] have shown no association between IBS and asthma; however, reports from USA [14], Iran [8], Canada [9], United Kingdom [7,15], Kuwait [6], Greece [12] and Turkey [3, 13,17] have shown positive association between IBS and either bronchial asthma or Bronchial Hyper-Responsiveness (BHR). It could be possible that the association of IBS and asthma has a regional variation. Multiple studies from Europe have reported this association, which might indicate the presence of regional, genetic, environmental and socio-economic factors leading to the presence of this association in that region. White AM et al., in1991 showed that IBS patients have BHR to methacholine [9]. In 1998, Kennedy TM et al., from United Kingdom (UK) in a questionnaire based study reported the presence of positive association between IBS and BHR [7]. Three studies from Turkey by Yazar A et al., Ekici A et al., Ozol D et al., with Panicker R et al., from Kuwait, Amra B et al., from Iran and Roussos A et al., from Greece reported increased prevalence of IBS in asthma patients versus controls [3,6,8,12,13,17]. There were two large scale robust prospective cohort studies one from USA by Cole JA et al., and the other from United Kingdom by Huerta C et al., that showed a higher incidence of IBS in asthmatic population in comparison to a matched control [14,15].
On the contrary, Riccioni G et al., investigated the link between IBS and asthma in Italy by utilizing Methacholine Challenge test (MCht) for BHR and reported no relation between BHR and IBS [10]. Similarly, Jun DW et al., from South Korea denied the presence of any relationship between BHR and IBS [11]. It is interesting to note that both the above studies utilized positive MCht as a criterion for asthma diagnosis. Steroid use was observed with decreased IBS risk in a study [15], while Roussos A et al., reported no change in IBS risk by any asthma medications [12]. Also there was no reported association between chronic bronchitis and IBS [7,8].
Limitation
Our study had its limitations. The sample size was small and the study was carried out at a single tertiary center rather than a population based cross-sectional study.
Conclusion
The findings in our study and in similar previous reports highlight the need for larger multi-center population based studies to establish a correlation between IBS and bronchial asthma. If there is an actual association between IBS and bronchial asthma, this would need a multi-disciplinary health care team approach to provide good quality care to the patients with IBS.
The Odds Ratio (OR) for prevalence of asthma in IBS is 0.828 with 95% Confidence Interval (CI) between 0.320 and 2.121 (p=0.664).