Isolated Skull Metastasis of Follicular Carcinoma Thyroid in an Elderly Female: A Rare Case
Archana Shetty1, Vijaya Chowdappa2, Padma Priya Kasukurti3
1 Associate Professor, Department of Pathology, Sapthagiri Institute of Medical Sciences and Research Center, Bangalore, India.
2 Professor and Head, Department of Pathology, Sapthagiri Institute of Medical Sciences and Research Center, Bangalore, India.
3 Assistant Professor, Department of Pathology, Sapthagiri Institute of Medical Sciences and Research Center, Bangalore, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Vijaya Chowdappa, Professor and Head, Department of Pathology, Sapthagiri Institute of Medical Sciences and Research Center, Hesaraghatta Main Road, Street No.15, Bangalore-560098, India.
E-mail: vijayakrshn0@gmail.com
Isolated skull metastasis from a well differentiated follicular thyroid carcinoma, as the presenting feature is a rare manifestation. We report a case of a 79-year-old female who presented to us with only a painful, gradually increasing scalp swelling with associated pain and blurring of vision over the past few days. Neuroimaging findings strongly favoured a diagnosis of meningioma. A bifrontal craniotomy was performed and the tumour was excised. Histopathological examination of the same showed, it to be a case of metastatic thyroid carcinoma. We present this case not only because of the diagnostic challenge it posed, but also because the patient in our case is one of the oldest case of skull metastasis from follicular thyroid carcinoma till date.
Bifrontal craniotomy, Dura, Meningioma, Scalp
Case Report
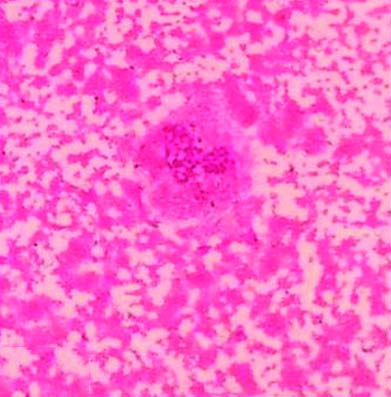
A 79-year-old female presented with swelling on the scalp associated with pain and blurring of vision since three months. The swelling was gradually increasing in size since the past eight months. On examination a single swelling was seen in the forehead region, extending on to the scalp, measuring 8x5 cm. Overlying skin appeared normal. The swelling was soft in consistency. X-ray of the skull showed an osteolytic soft tissue swelling with bony erosions in the frontoparietal region. The lesion was seen destroying the outer and inner table of the bilateral frontal and parietal bones, extending extradurally under the scalp [Table/Fig-1]. Fine needle aspiration, on repeated aspirates yielded haemorrhagic material. The smears were paucicellular, with cytological features favouring an adnexal tumour [Table/Fig-2]. Background showed large areas of haemorrhage.
X-ray of the skull showing an osteolytic legion in the fronto parietal region;

Aspirate smear of the swelling showing large areas of haemorrhage with a small cluster of round to oval cells with indistinct cell borders (H&E stain, 40 x);
Computed Tomography (CT) of the brain showed a well-defined heterogenous soft tissue density lesion in the midline located mainly in the pre frontal region with internal calcification. The underlying lesion showed erosion and destruction of the bone with intracranial extension. The lesion was limited by the duramater and measured 9x6.5 cm, extending upto the frontal sinus and nasion [Table/Fig-3]. Skin over the lesion appeared stretched.
CT brain without contrast showing well defined heterogenous soft tissue density, with internal calcification, eroding the frontal bone. (left to right)

With a strong suspicion of meningioma a bifrontal craniotomy was performed after embolizing the feeding vessel. The tumour was very vascular, with attachments to the dura and sagital sinus.
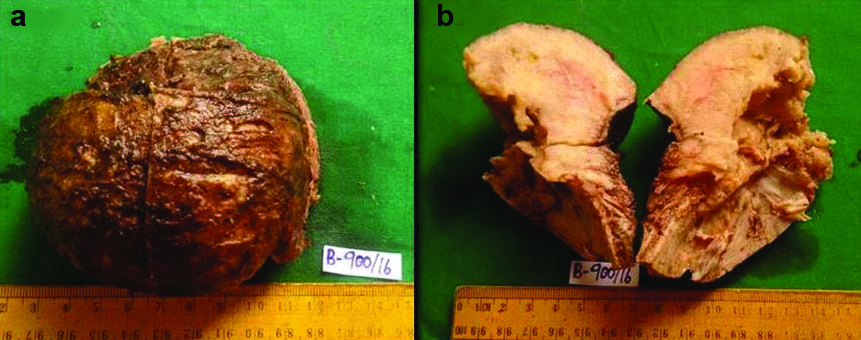
Grossly the excised specimen consisted of a globular dura covered mass of tumour with the underlying frontal bone. Tumour measured 6x4 cm and the bony base measured 5x4 cm. Cut section of the tumour showed a fleshy grey white mass, extending into the underlying bone. All the bony margins except the base were involved by tumour grossly. Tiny areas of haemorrhage were noted [Table/Fig-4a,b].
(a) Surgically resected tumour mass with underlying attached portion of frontal bone; (b) Cut section of the excised mass showing a fleshy grey white tumour, extending into the bony margins.
Histopathology of the same showed a partially encapsulated neoplasm composed of thyroid follicular cells in macrofollicles, microfollicles and trabecular pattern separated by sinusoids. The cells were round to oval with increased nucleocytoplasmic ratio, vesicular nucleus and conspicuous nucleoli in some cells, with moderate amount of pale to eosinophilic granular cytoplasm. Some of the follicles showed thick colloid with scalloped edges. The follicles were seen invading the mature bony trabecular at places. Focal specks of calcification were noted [Table/Fig-5a,b].
(a) Microphotograph showing a neoplasm comprising of microfollicles, with extension into the bony trabeculae. (H&E, 100X); (b) Microphotograph showing varying sized micro and macro follicles, with colloid. (H&E, 100X).
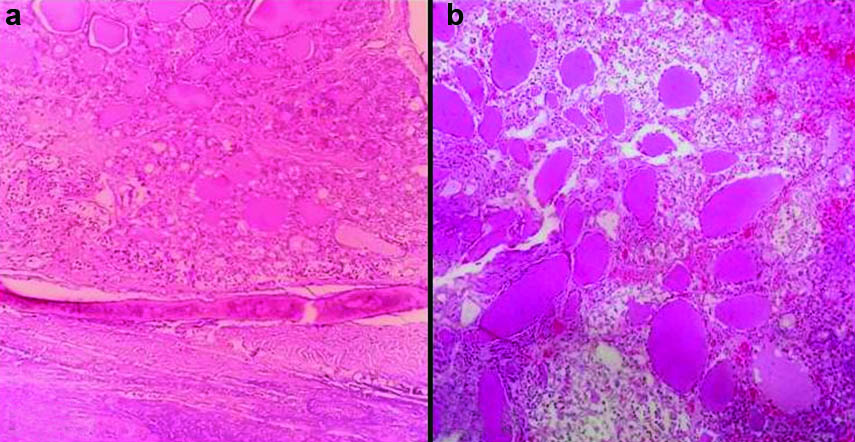
Immunohistochemistry done, showed the tumour foci to be positive for thyroglobulin. A diagnosis of metastatic follicular carcinoma of the thyroid was conferred upon, with a note to work up for the primary lesion. The patient postoperatively suffered a cardiac arrest, was tracheotomised and succumbed to sepsis on the third postoperative day before a primary in the thyroid was worked up for.
Discussion
Follicular Carcinoma of the Thyroid (FTC) accounts for 10-15 % of all clinically evident thyroid malignancies [1,2]. Among patients of differentiated thyroid cancers (papillary and follicular) in spite of an overall good prognosis, 5-23% of them have distant metastasis, leading to a poor prognosis despite adequate surgical and medical treatment [3].
Bone metastasis from FTC is commonly seen in long bones of the body like femur, flat bones like pelvis and sternum, while papillary cancers involve ribs, vertebrae and sternum. [4]. Skull metastasis accounts for only 2.5% of all cases, with intracranial metastasis of FTC seen in only about 1% of these cases [1,5]. The largest series of reported skull metastasis from thyroid carcinoma by Nagamine Y et al., described a frequency of only 2.5% among 473 patients [6]. Because of the rarity of skull metastasis, role of preoperative therapy has not been standardized till date.
Although calvarial metastasis from FTC can occur at any age, the youngest patient till date is just 18 years old, with most patients being in the age group of 60 to 70 years. Calvarial involvement of FTC shows a female preponderance [3]. The patient in our case was a 79-year-old female, probably the oldest documented case of isolated calvarial metastasis from FTC till date. The calvarial metastasis of FTC commonly presents as a painless scalp mass, often growing to large size as to cause neurological symptoms like increased intracranial pressure, headache, and seizures [7]. Our patient presented with a painful forehead swelling. The blurring of vision which the patient complained of was overlooked considering it to be an age related factor.
Radiological features of metastatic FTC are often difficult to distinguish from meningioma, as both have overlapping features. These lesions are osteolytic on X-ray and CT scan, and show high vascularity on angiographic assessment. On MRI single lesions, invading the subcutaneous tissue but limited by the duramater, round or oval lesions with osteolytic features, favour a metastatic carcinoma over meningiomas [1,4]. However, these features can also be seen in other metastatic carcinomas like hepatocellular carcinoma.
Histopathology is crucial in the diagnosis of follicular carcinomas, as vascular invasion and capsular invasion can be proven only on these grounds. FNA in such cases is of limited value as it cannot give us any clue of the invasion status. In our case there was no evidence of any thyroid mass or dysfuction, hence no work up was done for the same preoperatively.
Excision of the metastatic lesion in the skull with removal of the thyroid gland is the ideal line of treatment followed by adjunctive radiation with iodine 131, and replacement therapy with L- thyroxine. Bone defects require extensive bone resection, often bleeding profusely with deaths being reported from extreme haemorrhages. Preoperative angiographic assessment is recommended with ligation or emobilization of the feeding vessels [8], as was done in our case. Only 17% of metastatic lesions to the brain take up iodine131, so the effect of radioactive ablation on brain metastasis is very restricted [9].
Our case was challenging because the tumour was also suspected to be a meningioma preoperatively. There was also no evidence of any other organ being involved by tumour to consider the scalp mass as a potential focus of metastasis on clinical examination. Similar case of thyroid carcinoma presenting as a dural metastasis mimicking a meningioma has been reported by Taziel M et al., [1].
Conclusion
Skull metastasis of follicular carcinoma thyroid can mimic meningiomas both clinically and on neuroimaging. Single tumours, confined to the dura with osteolytic features often favour a metastatic focus in the skull. Clinicians must have high index of suspicion when dealing with solitary hypervascular lesions in the head and neck region, keeping in mind the fact that they can be metastatic foci too.
[1]. Taziel M, Essadi I, Errihani H, Thyroid carcinoma presenting as a dural metastasis mimicking a meningioma: A case reportN Am J Med Sci 2011 3(1):39-42. [Google Scholar]
[2]. Ogawa Y, Sugawara T, Seki H, Sakuma T, Thyroid follicular carcinoma metastasized to the lung, skull, and brain 12 years after initial treatment for thyroid gland—case reportNeurol Med Chir (Tokyo) 2006 46:302-05. [Google Scholar]
[3]. Shen J, Wang S, Zhao X, Shao X, Jiang X, Dai Y, Skull metastasis from follicular thyroid carcinoma: report of three cases and review of literatureInt J Clin Exp Pathol 2015 8(11):15285-93. [Google Scholar]
[4]. Shamim MS, Khursheed F, Bari ME, Chisti KN, Enam SA, Follicular thyroid carcinoma presenting as solitary skull metastasis: report of two casesJ Pak Med Assoc 2008 58(10):575-77. [Google Scholar]
[5]. Akdemir I, Erol FS, Akpolat N, Ozveren MF, Akfirat M, Yashi M, Skull metastasis from thyroid follicular carcinoma with difficult diagnosis of the primary lesionNeurol Med Chir(Tokyo) 2005 45:205-08. [Google Scholar]
[6]. Nagamine Y, Suzuki J, Katakura R, Yoshimoto T, Matoba N, Takaya K, Skull metastasis of thyroid carcinoma. Study of 12 casesJ Neurosurg 1985 63:526-31. [Google Scholar]
[7]. Feng D, Rhatigan R, Shuja S, Wolfson D, Makary R, Koch K, Papillary thyroid carcinoma with metastasis to the frontal skullDiagn Cytopathol 2009 37:522-26. [Google Scholar]
[8]. Jehangir A, Pathak R, Aryal M, Qureshi A, Jehangir Q, Alweis R, Thyroid follicular carcinoma presenting as metastatic skin nodulesJ Community Hosp Intern Med Perspect 2015 5(1):26332 [Google Scholar]
[9]. Matsuno A, Murakami M, Hoya K, Yamada SM, Miyamoto S, Yamada S, Clinicopathological and molecular histochemical review of skull base metastasis from differentiated thyroid carcinomaActa Histochem Cytochem 2013 46:129-36. [Google Scholar]